This information will help you get ready for your portal vein embolization (EM-boh-lih-ZAY-shun) at MSK.
What is your portal vein?
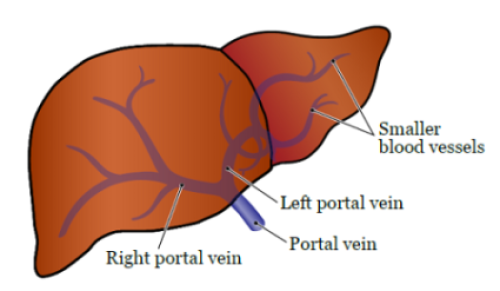
Your portal vein is a vein that carries blood to your liver. It splits into the left and right portal veins that branch into smaller blood vessels. Your blood vessels send blood throughout your liver (see Figure 1).
What is a portal vein embolization?
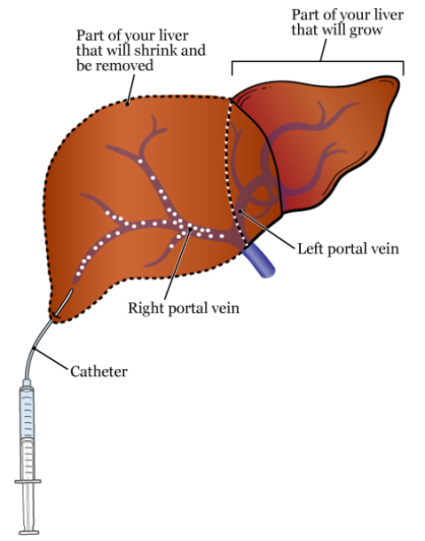
A portal vein embolization (PVE) is a procedure to block blood flow to liver tumors. This shrinks the part of your liver that has tumors. More blood will flow to the healthy part of your liver and make it grow. About 3 to 4 weeks after your PVE, you will have liver resection surgery. This procedure safely removes the shrunken part of your liver that has tumors.
During your PVE, you’ll get contrast dye (also called contrast). Contrast is a liquid used in X-rays. It helps your healthcare provider get a better look at your organs and blood flow. Tell your healthcare provider if you’ve had an allergic reaction to contrast dye in the past. For more information, read Preventing An Allergic Reaction to Contrast Dye (www.mskcc.org/pe/allergic_reaction_contrast).
You will get general anesthesia (medication to make you sleep during your procedure). Your healthcare provider will numb the upper right part of your abdomen (belly) near your liver. An interventional radiologist (IR doctor) will do your PVE. An IR doctor is a specialist in image-guided procedures.
Your IR doctor will use ultrasound and images from fluoroscopy (real-time X-rays) to guide your PVE. They’ll use these images to access your portal vein and decide which branch of your portal vein to block. These images will also help them guide a catheter (small, flexible tube) through your portal vein. Then, they’ll inject tiny particles into your portal vein (see Figure 2). These particles will block blood flow to that part of your liver.
Your PVE will take about 2 to 3 hours.
What To Do Before Your Portal Vein Embolization
Ask about your medicines
You may need to stop taking some of your medicines before your procedure. Talk with your healthcare provider about which medicines are safe for you to stop taking. We’ve included some common examples below.
Blood thinners
Blood thinners are medicines that affect the way your blood clots. If you take blood thinners, ask the healthcare provider performing your procedure what to do. They may recommend you stop taking the medicine. This will depend on the type of procedure you’re having and the reason you’re taking blood thinners.
Examples of common blood thinners are listed below. There are others, so be sure your care team knows all the medicine you take. Do not stop taking your blood thinner without talking with a member of your care team.
|
|
Read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil (www.mskcc.org/pe/check-med-supplement). It has information about medicines you must avoid before your procedure.
Medicines for diabetes
Before your procedure, talk with the healthcare provider who prescribes your insulin or other medicine for diabetes. They may need to change the dose of the medicine you take for diabetes. Ask them what you should do the morning of your procedure.
Your care team will check your blood sugar levels during your procedure.
Diuretics (water pills)
A diuretic is a medication that makes you urinate (pee) more often. Hydrochlorothiazide (Microzide®) and furosemide (Lasix®) are common diuretics.
If you take any diuretics, ask the healthcare provider doing your procedure what to do. You may need to stop taking them the day of your procedure.
Take devices off your skin
You may wear certain devices on your skin. Before your scan or procedure, device makers recommend you take off your:
- Continuous glucose monitor (CGM)
- Insulin pump
Talk with your healthcare provider about scheduling your appointment closer to the date you need to change your device. Make sure you have an extra device with you to put on after your scan or procedure.
You may not be sure how to manage your glucose while your device is off. If so, before your appointment, talk with the healthcare provider who manages your diabetes care.
Arrange for someone to take you home
You must have a responsible care partner take you home after your procedure. A responsible care partner is someone who can help you get home safely. They should be able to contact your care team if they have any concerns. Make sure to plan this before the day of your procedure.
If you don’t have a responsible care partner to take you home, call one of the agencies below. They’ll send someone to go home with you. There’s a charge for this service, and you’ll need to provide transportation. It’s OK to use a taxi or car service, but you still need a responsible care partner with you.
| Agencies in New York | Agencies in New Jersey |
| VNS Health: 888-735-8913 | Caring People: 877-227-4649 |
| Caring People: 877-227-4649 |
Tell us if you’re sick
If you get sick (including having a fever, cold, sore throat, or flu) before your procedure, call your IR doctor. You can reach them Monday through Friday from to
After , during the weekend, and on holidays, call 212-639-2000. Ask for the Interventional Radiology fellow on call.
Note the time of your appointment
A staff member will call you 2 business days before your procedure. If your procedure is scheduled for a Monday, they’ll call you on the Thursday before. They’ll tell you what time to get to the hospital for your procedure. They will also remind you where to go.
Use this area to write down the date, time, and location of your procedure:
If you don’t get a call by noon (12 p.m.) on the business day before your procedure, call 646-677-7001. If you need to cancel your procedure for any reason, call the healthcare provider who scheduled it for you.
The Day Before Your Portal Vein Embolization
Instructions for eating and drinking: 8 hours before your arrival time
|
The Day of Your Portal Vein Embolization
Instructions for drinking: 2 hours before your arrival time
| Stop drinking 2 hours before your arrival time. This includes water. |
Things to Remember
- Take only the medications your healthcare provider told you to take the morning of your procedure. Take them with a few sips of water.
- Do not use cream or petroleum jelly (Vaseline®). You can use deodorant and light moisturizers.
- Do not wear eye makeup.
- Remove any jewelry, including body piercings.
- Leave all valuables at home. This includes credit cards and jewelry.
- If you wear contact lenses, wear your glasses instead, if you can.
What to Bring
- Medications for breathing problems. This includes inhalers, medications for chest pain, or both.
- An extra CGM or insulin pump, if you wear one and had to remove it before your procedure.
- A case for your glasses or contacts, if you wear them.
- Your Health Care Proxy form and other advance directives, if you filled them out.
- Your CPAP or BiPAP machine if you use one. If you cannot bring yours with you, we will give you one to use while you’re in the hospital.
What to Expect When You Arrive
Many staff members will ask you to say and spell your name and birth date. This is for your safety. People with the same or similar names may be having a procedure on the same day. When it’s time for your PVE, you’ll get a hospital gown and nonskid socks to wear.
Meet with a nurse
You’ll meet with a nurse before your procedure. Tell them the dose of any medications you took after midnight (12 a.m.) and the time you took them. Make sure to include prescription and over-the-counter medications, patches, and creams.
Your nurse may place an intravenous (IV) line in one of your veins, usually in your arm or hand. If your nurse does not place the IV, your anesthesiologist will do it in the procedure room.
Meet With Your IR Doctor
You will talk with your IR doctor before your PVE. They’ll talk with you about the procedure and answer any questions you have before you sign a consent form. Signing this form means that you agree to the procedure and understand the risks.
Meet with an anesthesiologist
You will also meet with an anesthesiologist (A-nes-THEE-zee-AH-loh-jist). An anesthesiologist is a doctor with special training in anesthesia. They will give you anesthesia during your procedure. They will also:
- Review your medical history with you.
- Ask if you’ve had any problems with anesthesia in the past. This includes nausea (feeling like you’re going to throw up) or pain.
- Talk with you about your comfort and safety during your procedure.
- Talk with you about the kind of anesthesia you’ll get.
- Answer questions you have about anesthesia.
Inside the Procedure Room
A staff member will bring you into the procedure room when it’s time for your PVE. Your healthcare provider will help you onto the exam table where you’ll lie on your back.
Your care team will attach you to equipment to track your pulse, breathing, and blood pressure. You will get oxygen through a thin tube that rests below your nose, and general anesthesia.
Your healthcare provider will numb the upper right part of your abdomen. The IR doctor will do your PVE. Then, they will remove the catheter and put a bandage over where the needle went into your skin.
After Your Portal Vein Embolization
In the Post-Anesthesia Care Unit (PACU)
You’ll be in the PACU when you wake up after your procedure. A nurse will be keeping track of your temperature, pulse, blood pressure, and oxygen levels. You may get oxygen through a tube resting below your nose or a mask over your nose and mouth. You’ll also have compression boots on your lower legs.
Tell your nurse if you’re feeling pain. They may give you medication for your pain.
Your care team will tell you when it’s safe to go home. You will need a responsible care partner to go with you.
Follow-Up Care
You will have a computed tomography (CT) scan 3 to 4 weeks after your procedure. This will help your healthcare provider see how your liver has changed. The blocked part of your liver should be smaller. The other part of your liver should be bigger. This will help them safely do liver resection surgery to remove the part of your liver that has tumors. Your care team will schedule your liver resection surgery around this time.
When to Call Your Healthcare Provider
Call your healthcare provider if you have:
- A fever of 100.4 °F (38.0 °C) or higher.
- New, or worsening pain that does not get better with medication.
- Shortness of breath or trouble breathing.
- Chest pain.
- Dizziness.
- Bruising.
- Nausea (feeling like you’re going to throw up) or vomiting (throwing up).
- A faster heart rate than usual.
- Any new symptoms.