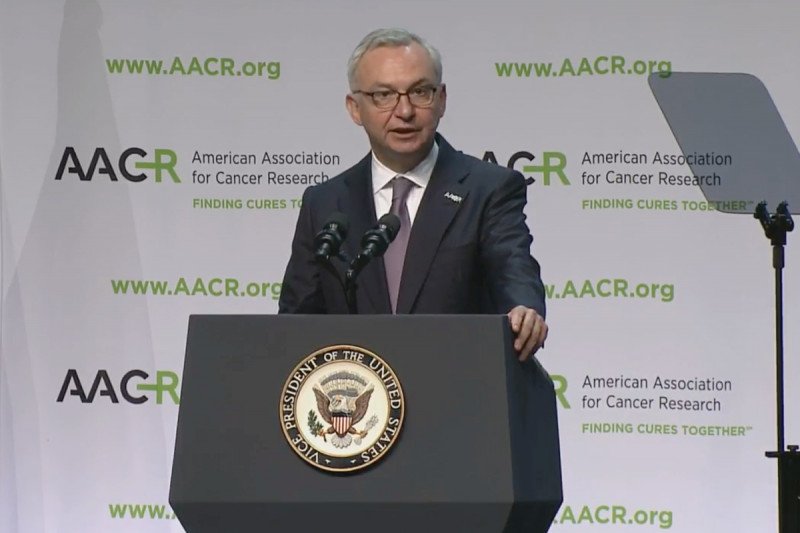
Outgoing AACR President and MSK Physician-in-Chief José Baselga summarized important clinical highlights at the close of the AACR conference on Wednesday.
Memorial Sloan Kettering scientists continued to offer leadership and insight on pressing matters of cancer care at the 2016 American Association for Cancer Research (AACR) conference, held this week in New Orleans. Here are some highlights from the second half of the conference. (Read our highlights from the first half of AACR here.)
Precision Medicine Progress
With advances in technology, it is now possible to rapidly sequence a patient’s entire genome — the complete string of DNA “letters” in a cell. By comparing the genome of a normal cell to that of a cancer cell, it’s possible to identify the particular molecular changes, or mutations, that set cancer cells apart. With this information in hand, doctors can more precisely deliver cancer treatments suited to a particular patient’s needs.
In his presidential address on Sunday, MSK Physician-in-Chief and outgoing AACR President José Baselga focused on the progress made in precision medicine for breast and other cancers. Genomic profiling of tumors is enabling patients at MSK and elsewhere to receive drugs that specifically target the mutations found in their tumors. This can mean more effective treatment as well as fewer side effects. And, re-sequencing tumors allows doctors to rapidly adapt treatment to the evolving tumor to address the problem of drug resistance, Dr. Baselga said.
A further boon of genetic sequencing is that it allows researchers to conduct what are called “basket trials.” In this type of study, patients are enrolled based on a specific genetic mutation they share rather than on the type of cancer they have. MSK was the first institution to successfully pursue this method and demonstrate its efficacy, through a study of a targeted drug called vemurafenib in patients with cancers sharing a mutation in the BRAF gene.
In his summary of clinical advances on Wednesday, Dr. Baselga highlighted the results of the MINDACT study, which looked at whether a genomic test, called MammaPrint, could improve the assessment of recurrence risk for women with early stage beast cancer. The study found that a subset of women who were deemed to be at high risk by conventional methods (like the appearance of cells under a microscope) but low risk by the genomic test, fared equally well whether they received chemotherapy or not. Dr. Baselga called the study of nearly 7,000 women a “tour de force” and said that the results were “practice changing,” in that they provide evidence that nearly half (46%) of women who are currently prescribed chemotherapy following surgery do not need it and can therefore be spared its damaging side effects, including impaired fertility.
Medical oncologist David Solit, who directs the Marie-Josée and Henry R. Kravis Center for Molecular Oncology at MSK, also emphasized the theme of precision medicine in a talk delivered on Tuesday. He discussed how genomic sequencing is allowing scientists at MSK to glean new insights into why some patients respond very well to drugs while others do not. By focusing on so-called exceptional responders, he says, it’s possible to uncover new insights connecting particular gene mutations to drug responses.
At MSK, every patient with advanced cancer has his or her cancer genome sequenced as a matter of course through a program called MSK-IMPACT™. This information is collected in an institutional database called Darwin, which generates an automated letter to the patient’s physician alerting him or her to clinical trials for which the patient is eligible, based on which mutations are found in the tumor.
Less than 3% of adults with cancer in the United States enroll in clinical trials. This means that many trials take longer to perform due to slow patient accrual, which in turn means it takes longer to test a drug’s efficacy. MSK-IMPACT is designed to address this problem. “The fastest way to test the drugs we have is to sequence everyone,” Dr. Solit said.
Targeting Metabolism
For many years, the study of cancer metabolism was seen as a somewhat dry, dusty affair. Researchers believed they knew all they needed to know about the process of metabolism, since most of the pathways had long since been immortalized in biochemistry textbooks. But starting with the work of MSK President and CEO Craig Thompson about a decade ago, researchers have begun to give metabolism a second look.
In a large plenary session held on Monday devoted to cancer metabolism, Dr. Thompson presented recent results from his lab that help to explain how cancer cells manage to acquire the often scarce nutrients they need to grow and reproduce. It’s the ability to access and use nutrients essentially at all times that, according to Dr. Thompson, is what sets cancer cells apart from their normal neighbors.
Think of a tumor as a ball of rapidly dividing cells. The cells on the inside of the ball will begin to starve as they lose access to nutrients and oxygen from the blood supply. Tumors promote the growth of new blood vessels to bring nutrients and oxygen to their center. But before they can recruit these new blood vessels, they are faced with a shortage of essential nutrients — particularly a few key amino acids that the body can’t synthesize on its own.
What Dr. Thompson’s recent work has shown is that certain common gene mutations, such as ones in a gene called RAS, enable cancer cells to do something normal cells cannot: ingest whole proteins from the cellular environment, break them down into component amino acids, and use these as the building blocks of new cell parts. In addition to helping to explain how cancer cells reprogram metabolism to fuel their growth, this finding also opens up new avenues for targeting cancer by interrupting this process.
Turbocharged CARs
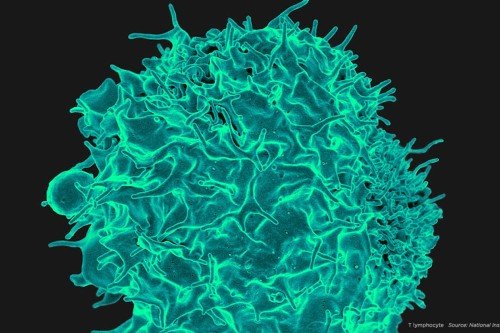
Immunotherapy continued to be a hot topic during the second half of the AACR meeting. Among the immunotherapy approaches generating the most excitement is chimeric antigen receptor (CAR) T cell therapy, in which immune cells are removed from a patient, genetically engineered to make a new protein that recognizes cancer, and given back to the patient in large numbers.
Michel Sadelain, Director of the Center for Cell Engineering at MSK, has been a pioneer in this field, having developed the first CARs that showed clear efficacy at treating cancer in an experimental system back in 2002. These days, the focus of research efforts is on developing next-generation models with superior design and function.
Second-generation CARs were engineered to have both a T cell-activating signal and co-stimulatory signal built in. What Dr. Sadelain called “turbocharged” CARs are second-generation CARs with a third component — the binding partner for a second co-stimulatory molecule. This additional signal boosts the activity and persistence of the T cells, allowing them to fight cancer more effectively, for longer.
Dr. Sadelain said that one potential benefit of these turbo CARs is their ability to activate other T cells in the area, helping to prevent “escape” of the tumor through loss of the original CAR T target (in the case of leukemia, a protein called CD19). These turbocharged CARs will be entering the clinic soon at MSK, he noted.
Turning Up the Heat
The other immunotherapy approach fueling excitement is checkpoint blockade therapy, in which drugs are used to “release the brakes” on the immune system, allowing it to mount a stronger attack against cancer. This approach is being used effectively to treat a growing list of cancers, including melanoma and lung, kidney, and bladder cancers.

Dr. Jedd Wolchok
Despite the dramatic effects of these drugs seen in some patients — including what look like complete cures — other patients do not respond at all. With existing immunotherapy drugs, for example, only about 20 to 40% of patients respond, leaving many others without good options.
MSK immunologist Jedd Wolchok, a leading researcher in this field, is working to improve the response rate to immunotherapies by developing effective combinations of drugs. Dr. Wolchok, a melanoma specialist, noted that patients with metastatic melanoma often have elevated levels of a type of immune cell called myeloid-derived suppressor cells (MDSCs), which act to dampen immune responses. He found that MDSCs are recruited to the site of tumors by a molecule called IDO. Drugs that block IDO are currently in clinical testing, but Dr. Wolchok’s work suggests other ways to intervene in this process — for example, by directing antibodies against a molecule found enriched on MDSCs.
His lab is also exploring the use of oncolytic viruses to kill cancer cells and prime an immune response against cancer elsewhere in the body. It’s through such combinations, Dr. Wolchok says, that physicians will be able to “turn up the heat” against some of the tumors that have so far resisted immune destruction.