Alan’s Story
In the beginning of his 34th year of teaching, Alan began feeling extremely tired and having difficulty breathing. He was diagnosed with T cell lymphoma, a rare type of cancer that originates in blood cells called T cells. Initial treatment put his cancer into remission, but only for a few months. He then came to Memorial Sloan Kettering to receive an experimental chemotherapy drug followed by a stem cell transplant.
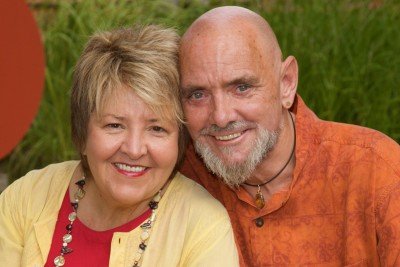
It was the fall of 2006 and Alan Stracke, a 61-year-old sociology professor, had begun his 34th year of teaching at Champlain College, in Burlington, VT. Suddenly, halfway through the semester, he began feeling extremely fatigued and had difficulty breathing.
“I looked in the mirror and discovered I had several lumps on each side of my neck, like marbles underneath my skin,” Alan recalls. “I looked like a reptile or a creature from a sci-fi movie. Then I noticed another lump in my upper leg. I was thinking, ’Whatever this is, it isn’t good.’”
“You Guys Will Just Have to Fix Me!”
Alan’s wife, Lynda, immediately took him to their local hospital. The doctors performed a variety of tests and diagnosed Alan with aggressive T cell lymphoma, a rare type of cancer that originates in blood cells called T cells, which are part of the body’s immune system. The disease was familiar to Alan, whose father had died of lymphoma in 1978. Nevertheless, his response to his doctor was spontaneous and simple: “Well, you guys will just have to fix me! I still have things to do.”
“It was not an attitude, it was just the way I felt,” he reflects. “I somehow knew it was not my time to go.” His wife’s inner determination was also a great comfort to Alan. “Lynda was rock steady and inspired me with her unwaveringly positive attitude.”
Soon after the diagnosis, Alan began a chemotherapy treatment known as CHOP, which is the acronym for the four drugs that he received in six consecutive dosages. By February 2007, Alan’s doctor declared him in full remission, meaning that all symptoms of his disease had subsided. A few months later, Alan and Lynda celebrated with a monthlong vacation on the Caribbean island of Tortola, where they had met in 1997.
“We Needed a Bigger Team of Horses”
Not long after he returned from the trip, Alan discovered that he again had enlarged lymph nodes on his neck. “It was obvious that my disease had come back,” Alan explains. “I began to realize that cancer, for me at least, is something I must learn to live with.”
Alan’s oncologist in Burlington told him he needed a stem cell transplant and advised him to make an appointment at Memorial Sloan Kettering Cancer Center. “He said — using Vermont-ese — that we needed ’a bigger team of horses on this problem,’” Alan recalls. “Those words made me realize my life would never be the same. I wasn’t afraid — I knew I was going to the top cancer facility in the nation. But the uncertainty and lack of control made me anxious.”
The first Memorial Sloan Kettering doctor Alan consulted was Steven Horwitz, a medical oncologist specializing in lymphoma. Dr. Horwitz told him about a new chemotherapy drug called pralatrexate, which, at the time, was beginning to show promise for treatment of Alan’s disease. Dr. Horwitz recommended that Alan enter a clinical trial, and Alan agreed to start right away. “My father had been part of numerous cancer drug studies in the 1970s, and I like to think that some of the findings from those studies may be keeping me and others alive today. It was my turn to assist the next generation.”
Pralatrexate turned out to be very effective in killing Alan’s cancer cells and has since been approved by the Food and Drug Administration for treatment of T cell lymphoma. However, in Alan’s case it also produced side effects, which in turn resulted in an acute blood infection. On two occasions, Alan spent five days in the intensive care unit at the local Burlington hospital. Dr. Horwitz and Alan’s Burlington oncology team kept in regular contact with each other and with Alan’s wife. Once Alan had recovered, he began receiving a chemotherapy regimen called ICE. By the end of this treatment, his cancer was in full remission again.
“Brother, I’ve Got This Little Problem”
At Memorial Sloan Kettering, Alan now met with Miguel-Angel Perales, a medical oncologist who specializes in treating patients with blood cancers such as lymphoma and leukemia by allogeneic (donor-derived) stem cell transplantation. Together, he and other doctors on Alan’s treatment team assessed that this procedure would be necessary to keep Alan cancer-free over time. In November 2007, Alan and Lynda moved to New York City on a temporary basis so that they could begin to prepare for his transplant.
“As was the case with everyone I came to know at Sloan Kettering — from the people who kept my room clean to the seasoned nurses and expert doctors — everyone was compassionate and caring,” Alan recalls. “Dr. Perales was no exception, and he was always completely up front with me. He made it clear that a stem cell transplant is a very serious matter, with many potential complications. He struck me as being very serious minded and professional.”
Alan was lucky to have a brother and a sister who were both what the doctors call “a perfect match,” meaning their blood cells were similar enough to Alan’s that his body was less likely to reject them. Because same-gender transplants tend to have fewer potential complications, Dr. Perales recommended that he receive the transplant from his brother, Paul.
“So I called Paul,” Alan recalls, “and said, ’Brother, I’ve got this little problem.’ And Paul, with whom I had not been in contact in recent years, replied, ’Just tell me where to be and when to be there.’ He was absolutely wonderful, and I fully realized the gift he was giving me. I believe I would have done the same thing for him in a second.”
Because transplantation can be very hard on the body, Alan underwent thorough physical examinations to ensure that he was strong enough to deal with the strains of transplantation. “I knew I was in for a series of challenges for the next stages of my life,” Alan says. “But I also recognized I had the best team of experts in the nation monitoring me constantly. I felt privileged and confident — everyone I came in contact with at Memorial Sloan Kettering genuinely cared for my well-being.”
“We’re Not Going to Have to Do This Again, Are We?”
During the first part of an allogeneic stem cell transplant, chemotherapy and radiation are administered to destroy a patient’s cancerous blood cells and blood-forming stem cells. After that, the patient receives an infusion of donor stem cells, which then migrate to the bone marrow and produce new, healthy blood cells, including cells of the immune system. It is believed that some of these immune cells play a role in fighting the cancer.
For five days in a row, Alan received chemotherapy followed by full-body radiation. “I never became nauseated from the chemotherapy. For me, the most difficult part was the radiation. It made me feel very weak and fatigued.”
Meanwhile, Alan’s brother had received daily injections of filgrastim, a drug that stimulates stem cells to leave the bone marrow and enter the circulating blood. After a few days, he had his blood drawn. “Paul is a super-athlete, and you’d never believe he’s 65,” Alan says. “After giving blood for two days, he took our sister on a three-hour walking tour of Times Square, and all around the city!”
“Afterwards,” Alan remembers, “he sat beside my bed and said, ’We’re not going to have to do this again, are we, bro?’ ’No way,’ I said, ’your stem cells are going to clobber mine, just as you have always clobbered me — in a loving big-brother fashion, of course.’”
“Today Is My New Birthday”
On the morning of the transplantation, a bag with stem cells harvested from Paul’s blood was hung over Alan’s bed and infused into his bloodstream. “I watched each drop as it came out of the bag and down through the line. I kept thinking, ’This is giving me a new life. Today, December 5, 2007, is my new birthday. This is a new me with unlimited possibilities!’”
The body’s ability to produce enough white blood cells to regenerate the immune system and prevent infections is vital for a successful transplant. And so, to protect himself from infections, Alan had to spend three weeks in the hospital in an isolation room while his immune system was built up. Lynda and Alan’s sister, Virginia, stayed in a rental apartment near the hospital and took turns caring for him. Whenever they visited Alan, they had to wear protective gloves and masks. “But I didn’t feel isolated at all,” Alan says. “Virginia and I have always had a riot together, and we pretended my room was a spaceship. She and my wife were the best company and effective advocates.”
Alan was deeply touched by the outpouring of greetings and messages from his friends, family, and students, who could receive regular updates through a Web site Lynda had set up. “One of the things I’ve learned,” Alan observes, “is that cancer is not necessarily the worst thing in the world. It allows people to connect, to express their love and compassion for one another. In a sense, I think it makes us more human.”
The Road Back
By the end of December, sooner than anyone had expected, Alan’s doctors said that he could leave his hospital bed and move into the apartment where his wife and sister were staying. His doctors were very satisfied with his recovery. However, as Dr. Perales had forewarned, the road back to “normal” life would be long and at times painful.
By April 2008, Alan moved back home to Burlington. “The last 20 months have at times felt endless, and pain has been an almost constant companion. At first my feet hurt so much I couldn’t walk,” he recalls. “It felt like I was walking on shards of glass.” Patrick Boland, an orthopaedic surgeon at Memorial Sloan Kettering, explained to Alan that the pain was due to large numbers of small stress fractures that had developed in Alan’s feet as a side effect of chemotherapy.
“As my feet healed and my legs returned to normal size, other pains and side effects emerged. But my ongoing physical therapy sessions, a positive determination, and a new appreciation for patience have helped me to gradually progress.”
A year and a half later, Alan is about to return to full-time teaching. “I grew up in an era when we wouldn’t even say the word cancer,” Alan says. “We’d say ’the big C,’ because if you had cancer it meant you were going to die. But that is no longer the case.”
“I am extremely fortunate to have been treated at Memorial Sloan Kettering,” he adds. “The level of personalized care and compassion I received there was something I had not expected from such a large and world-renowned institution.”



