This information will help you get ready for your thoracotomy surgery at MSK Kids. It’ll also help you understand what to expect during your recovery. In this resource, the words “you” and “your” refer to you or your child.
Read through this resource at least once before your surgery and use it as a reference in the days leading up to your surgery.
About Your Surgery
The word “thoracic” refers to your thorax, which is your chest (see Figure 1). Your thorax contains your heart and lungs.
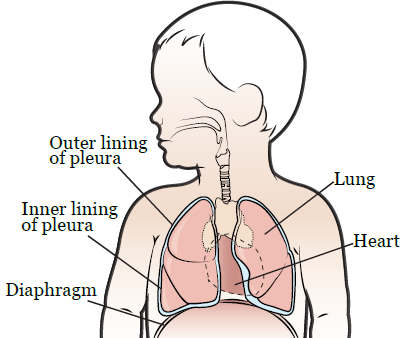
Figure 1. Your thorax
You have 2 lungs, 1 on each side of your chest. Your lungs are made up of lobes. Your left lung has 2 lobes and your right lung has 3 lobes. Your lungs are surrounded by 2 thin layers of tissue called the pleura.
A thoracotomy is a surgical incision (cut) into your chest. It’s done when you’re having surgery on or near one of your lungs.
During your thoracotomy, your surgeon will make an incision on one side of your back below your shoulder blade (see Figure 2). The side your incision is on depends on which lung is being operated on.
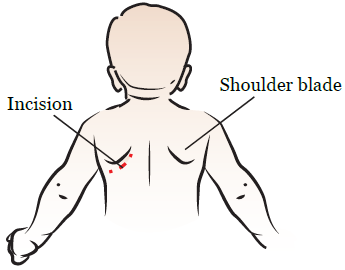
Figure 2. A thoracotomy incision
Before Your Surgery
Your nurse will give you instructions about how to get ready for your surgery. Be sure to follow all the instructions that your doctor and nurse give you. Call your doctor’s office if you have any questions.
You’ll meet with your anesthesiologist (person who will give you medication to make you sleep during your surgery) before your surgery. They’ll talk with you about medications to manage your pain and keep you comfortable after your surgery. There are different ways these medications can be given.
- Epidural catheter: Some people may get pain medication through an epidural catheter (thin, flexible tube in your spine). The medication will be given into the space outside your spinal cord.
- Peripheral nerve catheter (nerve block): Some people may get pain medication through a peripheral nerve catheter, also called a nerve block. The medication will be given to the nerves that give feeling to the area of your surgery.
- Intravenous (IV) pain medication: Some people may get pain medication into a vein through their IV line.
- Oral pain medication: Some people may get oral pain medication (medication they swallow).
You’ll have 1 or more of these things after your surgery.
During Your Surgery
You’ll lie on your side on the operating table. You’ll get anesthesia (medication to make you sleep). Once you’re asleep, your surgeon will make the following incisions:
- An incision on your back below one of your shoulder blades. This will let your surgeon reach your lung.
- One or 2 small incisions on the front of your chest, on the same side of your body as the incision on your back. This is where your surgeon will place a chest tube(s) to remove any blood, fluid, and air that’s around your lung after your surgery.
Central venous catheter (CVC)
Some people will also have a temporary central venous catheter (CVC) placed during their surgery. A CVC is a thin, flexible tube that’s placed in a large vein below your collarbone. Having a CVC makes it easier for you to get things like fluids and medications and means that you won’t need as many needle sticks.
You can learn more about CVCs by reading our resource About Your Central Venous Catheter (CVC) for Pediatric Patients.
After Your Surgery
When you wake up after your surgery, you’ll be in the Post Anesthesia Care Unit (PACU). As soon as you’re settled in the PACU, a nurse will bring your family member(s) in to be with you.
A nurse will be keeping track of your body temperature, pulse, blood pressure, and oxygen levels. You’ll get oxygen through a thin tube that rests below your nose called a nasal cannula.
There will also be other tubes and devices connected to your body to help you recover.
-
You’ll have 1 or 2 chest tubes. The chest tubes will go from your surgical site to a drainage device (see Figure 3).
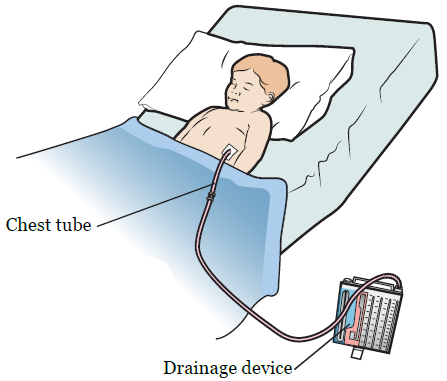
Figure 3. Chest tube and drainage device
- You’ll have a pain pump called a patient-controlled analgesia (PCA) device. The PCA device lets you give yourself pain medication when you need it. You may get the pain medication through an epidural catheter or your IV line.
- You’ll have compression boots on your lower legs to help your blood flow. They’ll be taken off when you’re able to walk.
- You may have a urinary (Foley) catheter in your bladder to keep track of how much urine (pee) you’re making.
You’ll stay in the PACU until you’re fully awake and your pain is under control. Once you’re ready, you’ll be taken to the Pediatric Intensive Care Unit (PICU) or the inpatient unit. The unit you go to depends on how old you are. There, your nurse will tell you how to recover from your surgery.
Below are examples of ways you can help yourself recover safely.
- It’s important to walk around after surgery. This will help prevent blood clots in your legs and lower your risk of developing pneumonia (lung infection). Try to walk every 2 hours, if you can.
- Use your incentive spirometer. This will help your lungs expand, which prevents pneumonia. Younger children can blow bubbles or use a pinwheel instead.
- Do deep breathing and coughing exercises every 1 to 2 hours while you’re awake.
Your nurse will give you a resource called Thoracotomy Pathway. This resource will help you know what to do and expect each day during your recovery.
It’s helpful to use your Goals to Discharge Checklist to track your recovery. We’ll send the checklist to your MyMSK account. For more information, read the resource Frequently Asked Questions About the MyMSK Goals to Discharge Checklist.
Before you leave the hospital, look at your incision with your nurse so you know what it looks like. It may be helpful to use a mirror. This will help you notice any changes once you’re at home.
Commonly Asked Questions
During your hospital stay
Will I have pain after my surgery?
You’ll have some pain after your surgery. Your doctor and nurse will ask you about your pain often. You’ll get medication to manage your pain as needed. If your pain isn’t relieved, please tell your doctor or nurse. It’s important to control your pain so you can cough, breathe deeply, use your incentive spirometer, and get out of bed and walk.
When will my chest tube be removed?
You’ll have chest x-rays to look at your lungs while the chest tube is in place. Once your lung heals, your chest tube will be removed. The area will be covered with a bandage. Keep the bandage on for at least 48 hours (2 days) after your chest tube is removed, unless your nurse gives you other instructions.
Will I be able to eat?
You’ll be able to eat after your surgery. Eating a balanced diet high in protein will help you heal after surgery. Your diet should include a healthy protein source at each meal, as well as fruits, vegetables, and whole grains.
For more information, read our resource Helping Your Child Eat During Treatment.
After you leave the hospital
What is the Recovery Tracker?
We want to know how you’re feeling after you leave the hospital. To help us care for you, we’ll send questions to your MyMSK account. We’ll send them every day for 10 days after you’re discharged. These questions are known as your Recovery Tracker.
Fill out your Recovery Tracker every day before midnight (12 a.m.). It only takes 2 to 3 minutes to complete. Your answers to these questions will help us understand how you’re feeling and what you need.
Based on your answers, we may reach out to you for more information. Sometimes, we may ask you to call your surgeon’s office. You can always contact your surgeon’s office if you have any questions.
To learn more, read Common Questions About MSK's Recovery Tracker.
Will I have pain when I am home?
The length of time each person has pain or discomfort varies. Some people may have soreness, tightness, or muscle aches around their incision for up to 6 months or longer. This doesn’t mean that something is wrong. Follow the guidelines below.
- Take your pain medication as instructed and as needed.
- Call your doctor if the medication prescribed for you doesn’t relieve your pain.
- As your incisions heal, you’ll have less pain and need less pain medication. An over-the-counter pain reliever such as acetaminophen (Tylenol®) or ibuprofen (Advil® or Motrin®) will relieve aches and discomfort. Be sure to follow your doctor’s instructions for how much to take.
- Pain medication should help you resume your normal activities. Take enough medication to do your exercises comfortably, but be sure to follow your doctor’s instructions. Oral pain medication works best 30 to 45 minutes after taking it, so it’s best to plan ahead.
- Keep track of when you take your pain medication. It’s best to take it when you first have pain. It won’t work as well if you take it after your pain gets worse.
Can I shower?
You can shower 48 hours (2 days) after your chest tube is removed. Taking a warm shower is relaxing and can help decrease muscle aches.
When you shower, use soap to gently wash your incisions. Pat the areas dry with a clean towel and leave your incisions uncovered (unless there’s drainage). Call your doctor if you see any redness or drainage from your incision.
For the first 2 weeks after your surgery, don’t submerge your incisions under water (such as in a bath tub or swimming pool).
How do I care for my incisions?
You’ll have 1 main surgical incision on your back and 1 or 2 smaller chest tube incisions on your chest. You may have some numbness below and in front of your incisions. This is because your ribs were spread apart and some nerves were affected.
Main surgical incision
- By the time you’re ready to leave the hospital, your surgical incision will have started to heal.
- Your incision will be covered with glue (Dermabond®) or paper tape (Steri-Strips®) that will fall off or peel away on their own.
- If any liquid is draining from your surgical incision, write down the amount and color and call your doctor.
Smaller chest tube incision(s)
- You’ll have a bandage covering your chest tube incision(s).
- Keep the bandage on your incision(s) for 48 hours (2 days) after your chest tube is removed, unless it gets wet. If it gets wet, change it as soon as possible.
- You may have some thin, yellow or pink-colored drainage from this area. This is normal. Put a bandage (such as a Band-Aid®) or dry piece of gauze over the area. Change the bandage as needed.
How can I prevent constipation?
You may be constipated (have fewer bowel movements than usual) after your surgery. This is a common side effect of pain medication. To avoid constipation:
-
Take an over-the-counter medication such as docusate sodium (Colace®), which is a stool softener, and senna (Senokot®), which is a laxative. Keep taking them until you’re no longer taking prescription pain medication.
- Take _____ capsules of docusate sodium 3 times a day.
- Take 2 tablets of senna before bed.
- Drink plenty of liquids. Aim for 8 to 10 (8-ounce) glasses (2 liters) each day. Choose liquids without caffeine, such as water, juices, soups, and ice cream shakes.
- If you feel bloated, avoid foods that can cause gas. Examples are beans, broccoli, onions, cabbage, and cauliflower.
How can I help my lungs heal?
- Continue to exercise or walk for at least 30 minutes every day. This will help you get stronger, feel better, and heal your lung. Keep using your incentive spirometer, straw, or pinwheel, and do your coughing and deep breathing exercises at home.
- Drink liquids to help keep your mucus thin and easy to cough up. Ask your doctor how much you should drink each day. For most people, this will be at least 8 (8-ounce) glasses of water or other liquids each day.
- Use a humidifier in your bedroom during the winter months. Follow the directions for cleaning the machine. Change the water often.
- Be careful not to get sick. Avoid close contact with people who have a cold, sore throat, or the flu. If you do get sick, call your doctor or nurse.
Is it normal to feel tired after surgery?
It’s common to have less energy than usual after your surgery. The time it takes to recover is different for everybody. Increase your activities each day as much as you can. Always balance activity periods with rest periods. Rest is an important part of your recovery.
Can I go back to doing my normal activities?
It’s important for you to go back to doing your normal activities after surgery. Spread them out over the course of the day. Walking and climbing stairs are excellent forms of exercise. Gradually increase the distance you walk. Climb stairs slowly, resting or stopping as needed.
Your body is an excellent guide for telling you when you have done too much. When you increase your activity, pay attention to how your body feels. You may find you have more energy in the morning or the afternoon. Plan your activities for times of the day when you have more energy.
Can I travel by plane?
Don’t travel by plane until you’ve discussed this with your doctor at your first appointment after your surgery.
When can I lift heavy objects?
Most people shouldn’t lift anything heavier than 10 pounds (4.5 kilograms) for at least 4 to 6 weeks after their surgery. However, this depends on the type of surgery you had. Ask your doctor how long you should avoid heavy lifting.
When can I play sports?
Don’t play sports until your doctor tells you it’s safe. When you start again, remember that it’ll take time for you to return to your previous level of activity. Start out slowly and increase your activity as you feel better.
How can I cope with my feelings?
After surgery for a serious illness, you may have new and upsetting feelings. Many people say they felt weepy, sad, worried, nervous, irritable, or angry at one time or another. You may find that you can’t control some of these feelings. If this happens, it’s a good idea to seek emotional support.
The first step in coping is to talk about how you feel. Family and friends can help. Your nurse, doctor, and social worker can reassure, support, and guide you. It’s always a good idea to let these professionals know how you, your family, and your friends are feeling emotionally. Many resources are available to patients and their families. Whether you’re in the hospital or at home, the nurses, doctors, and social workers are here to help you and your family and friends handle the emotional aspects of your illness.
When is my first appointment after my surgery?
When you’re discharged home from the hospital, your doctor or nurse practitioner will tell you your follow up appointment date. During this appointment, your doctor will discuss the pathology results with you in detail and check how you’re recovering.
When to Call Your Doctor or Nurse
Call your doctor or nurse if you have:
- New or worsening shortness of breath
- A fever of 100.4 °F (38 °C) or higher
- Pain that doesn’t get better with your medications
- Redness, swelling, or foul-smelling or pus-like drainage around your incisions
- No bowel movement for 3 days or longer
- Any new symptom
- Any questions or concerns
Contact information
If you have any questions, contact a member of your healthcare team directly. You can reach them Monday through Friday from to
If you’re a patient at MSK and you need to reach a provider after , during the weekend, or on a holiday, call 212-639-7900. Ask to speak to the pediatric surgeon on call.
