
Before the pandemic, Dr. John Chodera’s lab focused on building computational models to improve the discovery of new cancer drugs. But during the pandemic, the lab pivoted to help find new drugs against COVID-19. Lessons from the effort are already aiding in the search for new cancer medicines.
Update: The COVID Moonshot team formally reported their results in Science in November 2023. The article was accompanied by a perspective titled “Preparing for the next pandemic.”
A billion billion operations per second — 1 million times faster than a high-end PC and 10 times more powerful than the world’s faster supercomputer.
That was the combined might of a volunteer DIY effort by scientists and science enthusiasts around the world who lent the processing power of their personal computers to the search for new medicines to treat COVID-19.
Dubbed the COVID Moonshot, the ambitious drug discovery project harnessed a distributed computing platform called Folding@Home to achieve this record-setting response.
For John Chodera, PhD, a computational chemist at Memorial Sloan Kettering Cancer Center’s Sloan Kettering Institute and one of the founders of the COVID Moonshot, it was more importantly an effort with its heart in the right place.
“Drug discovery is extremely difficult. Trying to develop a new drug can take a decade and cost tens of millions of dollars,” he says. “Our idea was to speed up that process by adopting a collaborative, open science, patent-free approach — and also ensure any new therapy we discovered would be available equitably and affordably across the globe.”
Before the pandemic, Dr. Chodera’s lab focused on building computational models to accelerate and improve the discovery of new cancer drugs, primarily targeted therapeutics known as kinase inhibitors.
Today, as the third year of the pandemic draws to a close, Dr. Chodera has a new title that grew out of the Moonshot: Co-Principal Investigator of a $69 million National Institutes of Health (NIH)–funded antiviral drug discovery center. Called ASAP, for Artificial Intelligence-driven Structure-enabled Antiviral Platform, the center is tasked with delivering new drug candidates against a host of viruses — from coronaviruses like SARS-CoV-2, to flaviviruses like Zika and dengue (which alone sickens 100 million people per year), to picornaviruses like the reemergent poliovirus — while prioritizing equitable and affordable global access.
ASAP will be one of the Antiviral Drug Discovery (AViDD) Centers for Pathogens of Pandemic Concern funded by NIH’s National Institute of Allergy and Infectious Diseases (NIAID) as part of the Antiviral Program for Pandemics (APP).
“One of the great things about the Sloan Kettering Institute is the mission is really to follow the science for the public good,” Dr. Chodera says.
And while that may seem like a 180-degree pivot for a cancer research lab, lessons from the Moonshot effort are already aiding in the search for new cancer drugs, he says.
“Many of the same problems we run into in antivirals apply to cancer, only instead of populations of people, we’re talking about populations of cells inside the body,” Dr. Chodera says. “The questions are the same, though: How can we develop better, more targeted small molecule therapeutics? How can we understand, anticipate, and short-circuit the emergence of drug resistance?”
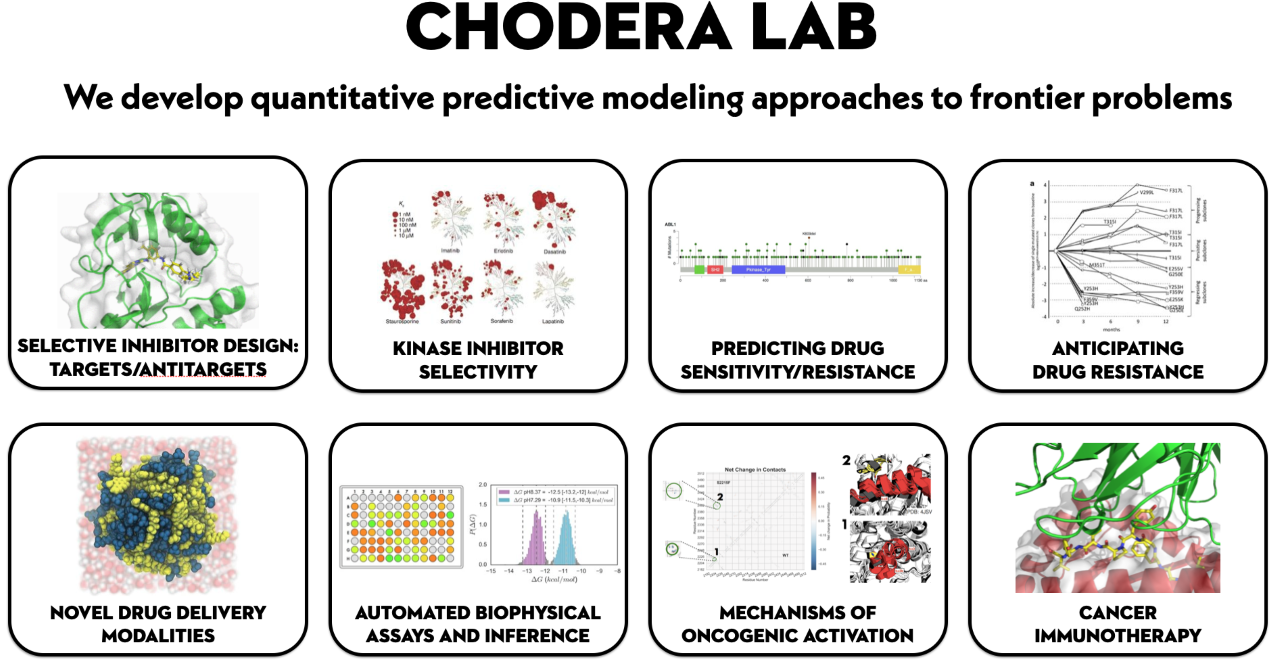
The Chodera Lab uses multiple approaches to anti-cancer drug discovery.
The Search for a COVID-19 Pill Begins
It was March 2020. America was just waking up to a new normal that included a strange new practice known as social distancing, an unprecedented enthusiasm for hand sanitizer, and a general pause on public life.
Scientists had quickly published the new coronavirus’ genome in January of that year. Then in February, a key part of the virus — the main viral protease — was crystallized by the Haitao Yang Lab in Shanghai. But when the lab was forced to shut down due to COVID-19, the members shared their material with researchers at Diamond Light Source, a billion-dollar government-run synchrotron in the United Kingdom.
There, in a matter of weeks, researchers completed a high-throughput X-ray crystallography screen using many pieces of druglike molecules — a comparatively cheap and efficient way to narrow down the field of initial candidates — and shared the results immediately online and through Twitter. The snapshots they obtained revealed a map for how a drug could potentially bind to the viral protease.
Trying to develop a small molecule inhibitor that targeted the protease — an enzyme critical for the replication of SARS-CoV-2, the virus that causes COVID — made good sense, Dr. Chodera says.
The protease is such a vital piece of the virus’ machinery, it would be less likely to be affected by mutations, unlike the virus’ spike protein where continuous changes have created new strains that evade the protection offered by vaccines. Plus, an oral pill could eliminate the need for subzero cold storage, making it easier to distribute worldwide. Moreover, unlike a vaccine, such a pill could potentially be taken after an exposure to prevent infection, or to reduce symptoms and avoid hospitalization.
Collaborations to attack the virus began to blossom on Twitter.
“We thought, ‘Surely with all of the scientists working on this, we could do this faster than the normal 10 years it usually takes,’ ” Dr. Chodera says. “In the beginning, there were a lot of people who said the pandemic was going to be over before we could possibly get a drug into the clinic — but obviously it’s still going on.”
Soon the open science approach drew collaborators from around the world.
Alpha Lee, DPhil, a scientist from Cambridge and co-founder of PostEra, a company that harnesses machine learning to improve drug discovery, enabled an online portal to help refine the results and solicit additional drug design ideas.
The response was overwhelming: thousands of designs ranging from the thoughtful to the bizarre (including the chemical structure of ethanol — booze — with the note, “I’m sure it works, on a dish at least”).
The best submissions were evaluated for how easily their components could be synthesized by partners like Enamine in Ukraine, which maintains an extraordinary catalog of synthetic chemistry building blocks, as well by as others around the world.
Meanwhile, medicinal chemist Ed Griffin, PhD, of MedChemica, lent his expertise to develop a list of properties that the drug should ultimately have — what’s known in the pharmaceutical industry as a target candidate profile — including how well it enters cells to inhibit the protease, how well it spares heathy cells, and whether it can be sufficiently potent in pill form.
To prioritize which compound designs are likely to be the most potent, the Chodera Lab develops computational tools called alchemical free energy calculations — a computational approach involving impossible-in-the-real-world (hence alchemical) molecular transformations that integrate physical models and machine learning.
But applying these models on the scale and pace of an accelerated discovery program like the COVID Moonshot required an enormous amount of computational power. So the group tapped into the Folding@Home Consortium to run computer simulations to prioritize candidates for testing in the lab. More than 1 million volunteers — primarily gamers with powerful graphics hardware — signed up to donate their effort to the cause.

In September 2021, Dr. Chodera and two colleagues penned an editorial for Knowable Magazine titled “Why we are developing a patent-free Covid antiviral therapy.”
Promising Compounds Headed to Clinical Trials
While most drug discovery happens behind closed doors, the COVID Moonshot made its data openly available right away.
“In a first for a structure-based drug discovery campaign, all compound designs (>18,000 designs), crystallographic data (>500 ligand-bound X-ray structures), assay data (>10,000 measurements), and synthesized molecules (>2,400 compounds) for this campaign were shared rapidly and openly, creating a rich open and [intellectual property]-free knowledgebase for future anti-coronavirus drug discovery,” the group wrote in a January 2022 preprint about the effort.
Dr. Chodera adds: “We went from a fragment screen to the preclinical phase in just 18 months, spending less than $1 million.
“This is one of these cases where we didn’t want to wait for a prestige journal to publish our work because people are dying — so we put everything online for free,” he continues. “This is pretty rare in the drug discovery world. The only similar model of patent-free therapeutics I’m aware of is the Salk polio vaccine.”
At the outset, the entire project was self-funded by the researchers and their home institutions, and supplemented by crowdfunding, though it eventually received a $10 million grant from the Wellcome Trust.
To date, the group has identified several compounds with excellent antiviral activity against the main SARS-CoV-2 protease. These are currently undergoing preclinical evaluation with a goal of starting the first human clinical trials in 2024.
The open science approach also led Japanese pharmaceutical company Shionogi to identify a promising COVID-19 drug based on a compound in their existing catalog, and for which clinical trials have already been launched.
“Stunningly, our lead compounds are equally potent against the original SARS virus, SARS-CoV-1,” Dr. Chodera says. “There’s no reason someone couldn’t have done exactly what we did back in 2004, and we would have had an oral antiviral that was clinic-ready at the start of this pandemic.”
He continues: “So this is a huge, huge market failure, right? Nobody wanted to spend just a few million dollars to take an antiviral all the way to clinic readiness because they were worried that they wouldn’t be able to make their money back in the lifetime of the patent. That’s why we need new models.”
Lessons for Cancer Drug Development
Meanwhile, the Chodera Lab at the Sloan Kettering Institute continues to work on cancer drug discovery, bringing insights from the COVID Moonshot to bear.
The process of developing tools to tackle a collaborative global initiative to find COVID-19 drugs was instructive in and of itself.
“We rarely have the funds to be able to do an experiment over and over again, where hundreds of molecules are synthesized and then tested in rapid iterations,” Dr. Chodera explains. “It’s been an immense learning opportunity to rapidly improve the effectiveness and utility of these discovery tools, which we will be able to pivot and apply directly to cancer.
“One of the things that we’ve been able to build to support the ASAP antiviral center is a fully automated workflow that uses Folding@Home to much more rapidly scale up these calculations,” he says. “So we are excited to be able to apply these tools at scale, using the infrastructure that we developed for antivirals, toward therapeutic discovery in cancer.”
Further Reading
- Artificial Intelligence-driven Structure-enabled Antiviral Platform (ASAP) website
- Why we are developing a patent-free Covid antiviral therapy, Knowable Magazine
- A white-knuckle ride of open COVID drug discovery, Nature commentary
- The coronavirus pandemic turned Folding@Home into an exaFLOP supercomputer, Ars Technica
- Folding@Home COVID-19 page
