This information will help you get ready for your ovarian transposition surgery at MSK. It will also help you know what to expect during your recovery.
About ovarian transposition
Ovarian transposition is a surgery that moves your ovaries out of the field of radiation. This will lower the amount of radiation your ovaries are exposed to during your radiation therapy. It may also help your ovaries keep working properly after your treatment. If your ovaries are working properly, you have a better chance of having children after your cancer treatment. You will also be less likely to go into early menopause (permanent end of menstrual cycles).
Your ovaries are located in the lower area of your pelvis (see Figure 1). In adults, the ovaries and fallopian tubes have to be separated from the uterus to move them far enough away (see Figure 2). In children, the ovaries and fallopian tubes can usually be moved out of the field of radiation without having to separate them from the uterus.
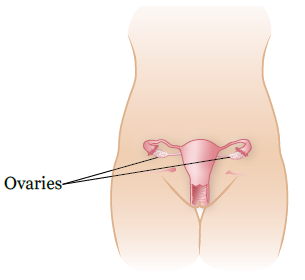
Figure 1. Location of ovaries before ovarian transposition surgery
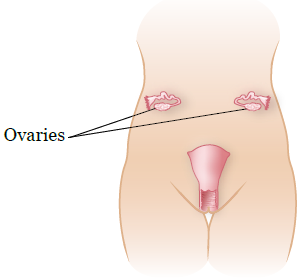
Figure 2. Location of ovaries after ovarian transposition surgery in adults
Having children after your cancer treatment
If you want to have children after your cancer treatment, here are some things you should know.
- If your ovaries and fallopian tubes are separated from your uterus during your ovarian transposition surgery, they can’t be reconnected or moved back after your treatment is over. This means that you won’t be able to get pregnant on your own. If you might want to get pregnant in the future, you will need to see a reproductive endocrinologist (fertility specialist).
- Even if you have an ovarian transposition, your ovaries will still be exposed to some radiation. This can affect your chances of having biological children, especially if you’re also getting chemotherapy.
- Some women have eggs collected and frozen before the surgery to improve their chances of having biological children. Ask your doctor if this is an option for you. If it is, and you’re interested in this, ask for a referral to a reproductive endocrinologist .
- We can’t move your uterus outside the field of radiation. Depending on the dose of radiation you’re getting, your uterus may be damaged. This could affect your ability to get pregnant or carry a child. Ask your radiation oncologist if you will be able to carry a pregnancy after your radiation therapy.
To learn more about fertility and fertility preservation, read Fertility Preservation Before Cancer Treatment: Options for People Born with Ovaries and a Uterus.
Before your surgery
Presurgical testing (PST)
You’ll have a PST appointment before your surgery. You’ll get a reminder from your surgeon’s office with the appointment date, time, and location.
You can eat and take your usual medicine(s) the day of your PST appointment.
It’s helpful to bring these things to your appointment:
- A list of all the medicines you’re taking, including prescription and over-the-counter medicines, patches, and creams.
- Results of any medical tests done outside of MSK in the past year, if you have them. Examples include results from a cardiac stress test, echocardiogram, or carotid doppler study.
- The names and telephone numbers of your healthcare providers.
You’ll meet with an advance practice provider (APP) during your PST appointment. They work closely with MSK’s anesthesiology (A-nes-THEE-zee-AH-loh-jee) staff. These are doctors with special training in using anesthesia during a surgery or procedure.
Your APP will review your medical and surgical history with you. You may have tests to plan your care, such as:
- An electrocardiogram (EKG) to check your heart rhythm.
- A chest X-ray.
- Blood tests.
Your APP may recommend you see other healthcare providers. They’ll also talk with you about which medicine(s) to take the morning of your surgery.
Ask about your medicines
You will need to stop taking some medicines before your surgery. Your nurse will give you the resource How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil. It has important information about these medications and what you can take instead.
There are some medicines that you may need to talk with your doctor about before your surgery. Some examples are listed in the following table:
| Examples of blood thinners | |||
|---|---|---|---|
| apixaban (Eliquis®) | dalteparin (Fragmin®) | meloxicam (Mobic®) | ticagrelor (Brilinta®) |
| aspirin | dipyridamole (Persantine®) | nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil®) or naproxen (Aleve®) | tinzaparin (Innohep®) |
| celecoxib (Celebrex®) | edoxaban (Savaysa®) | pentoxifylline (Trental®) | warfarin (Coumadin®) |
| cilostazol (Pletal®) | enoxaparin (Lovenox®) | prasugrel (Effient®) | |
| clopidogrel (Plavix®) | Fondaparinux (Arixtra®) | rivaroxaban (Xarelto®) | |
| dabigatran (Pradaxa®) | heparin (shot under your skin) | sulfasalazine (Azulfidine®, Sulfazine®) | |
Please read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil. It has important information about medicines you’ll need to avoid before your procedure and what medicines you can take instead.
Medicines for diabetes
If you take insulin or other medications for diabetes, ask the doctor who prescribes the medication what you should do the morning of your procedure. You may need to change the dose before your procedure.
Arrange for someone to take you home
You must have a responsible care partner take you home after your surgery. A responsible care partner is someone who can help you get home safely. They should be able to contact your care team if they have any concerns. Make sure to plan this before the day of your surgery.
If you don’t have a responsible care partner to take you home, call one of the agencies below. They’ll send someone to go home with you. There’s a charge for this service, and you’ll need to provide transportation. It’s OK to use a taxi or car service, but you still need a responsible care partner with you.
| Agencies in New York | Agencies in New Jersey |
| VNS Health: 888-735-8913 | Caring People: 877-227-4649 |
| Caring People: 877-227-4649 |
The day before your surgery
Note the time of your surgery
A staff member will call you after the day before your surgery. If your surgery is scheduled for a Monday, they’ll call you the Friday before. If you do not get a call by , call 212-639-5014.
The staff member will tell you what time to get to the hospital for your surgery. They’ll also remind you where to go.
This will be at one of these locations:
|
|
|
Instructions for eating and drinking before your surgery
|
The day of your surgery
Remember, starting 8 hours before your scheduled arrival time, do not eat or drink anything except the things listed earlier.
Instructions for drinking before your surgery
| Stop drinking 2 hours before your arrival time. This includes water. |
Things to remember
- Wear something comfortable and loose-fitting.
- If you wear contact lenses, wear your glasses instead. Wearing contact lenses during surgery can damage your eyes.
- Take only the medications you were instructed to take the morning of your surgery. Take them with a few sips of water.
- Don’t put on any lotion, cream, powder, deodorant, makeup, powder, or perfume.
- Don’t wear any metal objects. Remove all jewelry, including body piercings.
- Leave valuables, such as credit cards and jewelry, at home.
- Before you’re taken into the operating room, you will need to remove your hearing aid(s), dentures, prosthetic device(s), wig, and religious articles.
Where to go
Check your appointment reminder, which will tell you where to go for your surgery.
What to expect
Once you arrive at the hospital, doctors, nurses, and other staff members will ask you to state and spell your name and date of birth many times. This is for your safety. People with the same or similar name may be having surgery on the same day.
You will change into a hospital gown and meet your nurse. They will place an intravenous (IV) line into a vein, usually in your hand or arm. At first you will get fluids through the IV, but it will be used later to give you anesthesia (medication to make you sleepy). Your doctor will explain the surgery, and answer any questions you have. When it’s time for your surgery, you will be brought into the operating room.
Once you’re in the operating room, you will be attached to equipment to monitor your heart, breathing, and blood pressure. You will also receive oxygen through your nose or mouth. You will receive anesthesia through your IV to make you sleepy.
During your surgery, your surgeon will make a small incision (surgical cut) on your abdomen (belly). They will put a small, telescope-like tool into the incision to see the inside your body. A gas (carbon dioxide) will be pumped into your abdomen so that your surgeon has room to work.
Then, your surgeon will make more small incisions and place other small tools inside your body. The exact location and number of incisions depends on how the surgery is done.
Then, your ovaries and fallopian tubes will be moved as far as possible from the area being treated and held in place with sutures (stitches). You won’t be able to feel your ovaries in the new position.
After your surgery
In the Post-Anesthesia Care Unit (PACU)
You’ll be in the PACU when you wake up after your surgery. A nurse will be keeping track of your temperature, pulse, blood pressure, and oxygen levels. You may get oxygen through a tube resting below your nose or a mask over your nose and mouth. You’ll also have compression boots on your lower legs.
You will feel some pain after your surgery, but your nurse will give you medication to help. If your pain doesn’t get better, tell your nurse.
You will have many small incisions on your abdomen. The incisions will be closed with Steri-Strips® (small strips of tape) or Dermabond® (surgical glue). Before you leave the hospital, your nurse will show you how to care for your incisions.
Most people can go home on the day of their surgery. You can go home once you:
- Can eat solid food. It may take many weeks for your appetite to return to what it was before your surgery.
- Can urinate (pee).
- Can walk.
- Aren’t in too much pain.
At home
You can shower 24 hours (1 day) after your surgery.
Clean your incisions with soap and water every day. If you go home with Steri-Strips or Dermabond covering your incisions, you can shower with them on. The Steri-Strips will begin to peel off in about 1 week. If they haven’t fallen off after 7 to 10 days, remove them in the shower. If you have Dermabond on your incisions, don’t remove it. It will dissolve over time.
Bowel function
You may not have a bowel movement for a few days after surgery. This is normal. If you don’t have a bowel movement for 3 days, call your doctor or nurse.
If you have diarrhea (loose, watery stools) call your doctor or nurse. Don’t take an antidiarrheal medication, such as loperamide (Imodium®) or bismuth subsalicylate (Kaopectate®), until you talk with your doctor or nurse.
Activities after your surgery
It will take 2 to 4 weeks for your incisions to heal. Until your doctor or nurse has told you that your incisions have healed:
- Don’t strain yourself or lift anything over 10 pounds (4.5 kilograms).
- Don’t place anything in your vagina or have vaginal intercourse for 4 weeks or until your doctor tells you it’s okay.
- Don’t drive if you’re taking prescription pain medications. If you aren’t taking prescription pain medications, you can drive 24 hours after your surgery.
If you’re traveling by plane within a few weeks after your surgery, get up and walk around every hour while you’re on the plane. Be sure to stretch your legs, drink plenty of liquids, and keep your feet raised whenever possible.
When to call your healthcare provider
Call your healthcare provider if you:
- Have swelling or tenderness in your calves or thighs.
- Have trouble breathing.
- Cough up blood.
- Have a fever of 101° F (38.3° C) or higher.
- Have serious abdominal pain that doesn’t get better after taking pain medication.

