MSK thoracic oncologist Charles Rudin presented his research on small cell lung cancer at a press briefing on Sunday morning.
With more than 30,000 attendees, the American Society of Clinical Oncology (ASCO) annual meeting is the largest cancer conference in the world. It’s currently housed in North America’s largest convention center — McCormick Place in Chicago — which means that anyone who attends gets some good exercise walking back and forth between sessions.
When we weren’t busy hiking the crowded halls of the convention center, we compiled a roundup of highlights from the first half of the conference, with a focus on emerging areas of inquiry.
“Smart Bomb” for Small Cell Lung Cancer
Despite the encouraging downward trend in US smoking rates, lung cancer remains a major public health challenge, with more than 220,000 Americans diagnosed every year. Several new and effective therapies exist for people with non-small cell lung cancers, who account for about 85% of new diagnoses. But for the 15% diagnosed with small cell lung cancers (SCLC), no significant treatment advance has been made since the 1970s.
Until this week. Yesterday at ASCO, MSK Thoracic Oncology Service Chief Charles Rudin presented results from an early-stage clinical trial evaluating an experimental targeted therapy called rovalpituzumab teserine (referred to as Rova-T). The therapy is what’s called an antibody-drug conjugate, consisting of a cancer-targeting antibody linked to a toxic payload.
“This type of therapy works like a Trojan horse,” said Dr. Rudin, the trial’s principal investigator. “After the antibody seeks out and binds to the cancer cell, it delivers the toxin to the inside of the cell, and the cell is destroyed. This particular toxin is too dangerous to be used on its own. But when it’s delivered in such a precise way, it can be well tolerated.”
In other words, a cancer smart bomb.
The protein to which Rova-T binds, called DLL3, is found at high levels in about 70% of SCLC tumors but is essentially absent from healthy adult tissues.
In this trial, a multicenter study sponsored by the drug maker Stemcentrx, 74 patients who had already received at least one other treatment were treated with Rova-T. Among the 26 patients with the highest levels of DLL3, 10 (39%) had a partial or complete response, meaning that their tumors decreased by at least 30%. About a third of these high-DLL3 patients were alive one year after treatment — substantially better than would be expected with current treatment options.
The Rova-T study was highlighted in the ASCO press program and Dr. Rudin presented the results at a press conference on Sunday. Based on the findings from this study, a larger trial has been initiated.
SCLC is a particularly aggressive type of lung cancer — most patients have extensive-stage disease at diagnosis, and the median survival is less than a year — which makes the results of the Rova-T trial so welcome.
“We’ve seen too few successes in recent years for small cell lung cancer, which makes these early signs of efficacy all the more encouraging,” Dr. Rudin said.
Combo Checkpoint Blockade in Non-Small Cell Lung Cancer
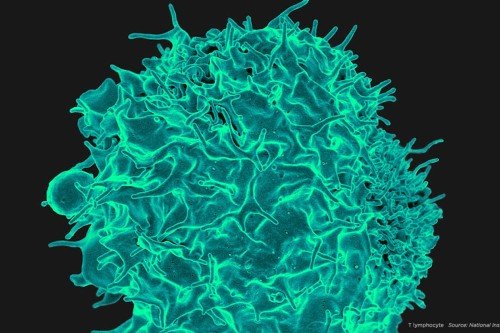
The other big source of excitement at ASCO this year is immunotherapy, treatments that harness the power of the immune system to fight cancer. Given how well some patients seem to do on the treatments — essentially being cured — that excitement seems justified.
And yet, one of the most frustrating aspects of current immunotherapy treatments is that they work for only a small subset of patients, typically between 10 and 20%. To try to get those numbers up, researchers are increasingly turning toward immunotherapy drug combinations.
On Saturday, MSK’s Matthew Hellmann presented results from a phase I study of one such combination — nivolumab and ipilimumab — in patients with previously untreated, advanced non-small cell lung cancer. Noting the “profound efficacy” of this combination in melanoma and the recent discovery that lung cancer is a type that the immune system can recognize, Dr. Hellmann said doctors were eager to test this combination in the disease, which is the world’s leading cancer killer.
In the trial, called CheckMate012 and sponsored by Bristol Myers-Squibb, 148 patients received one of several different dosages of the drug combination. The primary objective of the study was to determine a safe dosage of the two drugs. The secondary objective was to determine their efficacy. For the dosage groups discussed in this presentation, the overall response rate for the combination ranged from 39 to 47%, which is more than twice the response rate of nivolumab alone (23%). There were no treatment-related deaths in these groups and the side effects were manageable.
Nivolumab and ipilimumab are what are known as immune checkpoint inhibitors. By “releasing the brakes” on the immune system, these drugs empower it to mount a stronger attack against cancer. Nivolumab releases a brake called PD-1, while ipilimumab targets one called CTLA-4.
Strikingly, the efficacy of the combo treatment correlated with the level of a protein called PD-L1 expressed by a patient’s tumor. Cancer cells make PD-L1, the binding partner of PD-1, as a way of warding off immune attack. By binding to PD-1 on immune cells, PD-L1 essentially steps on the immune-system brake. According to Dr. Hellmann, the response rate was much higher in patients with more PD-L1 expression in their tumor. For patients with more than 50% PD-L1 in their tumors, for example, the response rate was 92%.
These results indicate that for certain patients, immunotherapies can indeed be a very powerful and effective treatment.
A Deep Dive into the Biology of Bladder Cancer
Before they can hope to boost overall response rates to immunotherapy, researchers need to have a good understanding of the underlying biology of tumors.
MSK’s Jonathan Rosenberg took ASCO attendees on a deep dive through the biology of bladder cancer, to help make sense of who responds to immunotherapy and who doesn’t.
Dr. Rosenberg led the phase II trial leading to FDA approval of the immunotherapy drug atezolizumab (Tencentriq®) for advanced bladder cancer last month. Atezolizumab is an immune checkpoint inhibitor that targets the PD-L1 protein found on cancer cells and immune cells. Overall, about 15% of advanced bladder cancer patients respond to atezolizumab, though those with higher levels of PD-L1 in their tumors have a higher response rate (about 28%).
As part of the above-mentioned trial, the investigators looked at three variables that they hypothesized might influence response to treatment: PD-L1 expression; specific gene signatures indicative of tumor subtype; and mutational load, or the number of genetic mutations found within a tumor. While all were independent predictors of response to atezolizumab, Dr. Rosenberg noted, mutational load was the best and most powerful of the three.
Mutational load is increasingly recognized as an important factor that can influence whether a patient responds to immunotherapy. MSK researchers have shown previously that in both melanoma and lung cancer, patients with a higher mutational load, on average, do better than those with lower numbers of mutations. Other studies on colorectal cancer have suggested the same effect of high mutational load.
But as MSK medical oncologist Alexandra Snyder Charen pointed out in her discussion of these studies, there are important exceptions to this rule. A few patients with low mutation burden respond, and a few with high burden do not. This raises the possibility that it is less the absolute number of mutations that is important and more the occurrence of a mutation that is particularly good at being spotted by the immune system. A high frequency of mutations may simply increase the chances that one of these “good” mutations will be formed.
Because of these exceptions, Drs. Rosenberg and Snyder Charen believe it would be wrong to withhold immunotherapy treatment from a patient on the basis of either PD-L1 expression or mutation burden.
“I’m not ready to exclude anyone at this time,” Dr. Rosenberg said during the question and answer session of the panel.
One reason why a person with a PD-L1-negative tumor might still respond to PD-1 therapy is that both cancer and the immune system are dynamic. Tumors that are PD-L1–negative at the beginning of treatment might become PD-L1–positive over time as the immune system revs up and starts fighting the cancer.
On Saturday, MSK medical oncology fellow Samuel Funt looked at yet another possible predictor of response to atezo in bladder cancer: the number and diversity of immune cells circulating in the blood before treatment. He found a strong correlation between diverse numbers of circulating immune cells and ultimate response to atezo.
Researchers hope to one day find a biomarker that will reliably predict who will respond to these therapies, to be able to offer the right drug, at the right time, to the right patient.