Some breast cancer treatments can increase the risk of heart disease.
The American Heart Association recently issued a statement about the dangers of heart problems in women treated for breast cancer. We spoke with the cardiologist Richard Steingart, to understand the link between the two.
What should a woman with breast cancer know about her risk of heart problems after treatment?
The first thing she should know is what the condition of her heart is before going into treatment. She should have a pretty good understanding of her risk of cardiovascular disease when she gets to the point of diagnosis.
From there, the cardiovascular risk of cancer therapy varies according to each woman. For example, does she have high blood pressure or an arrhythmia, which is an irregular heart rhythm? Has she had a heart attack? All of those factor into the decision-making process about the choice of breast cancer therapy.
So ideally, before she even starts treatment, there would be a discussion about her heart health.
That’s right.
What about women who have already completed treatment?
They also need to understand their heart health. Every woman should have that discussion with her primary care doctor. Does she have heart disease? What are her risk factors for developing it as time goes by? Then she needs to compile a full list of what her breast cancer treatments were and have a discussion with her doctor about whether or not those treatments impact her current or future heart health.
What research are you doing on breast cancer treatment and cardiovascular risks?
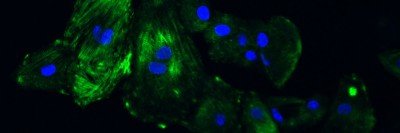
We’re trying to figure out how best to monitor women while they’re being treated. Although there are substantial concerns about the side effects of treatment, only a small proportion of women are affected. It’s not easy to know ahead of time which women are impacted by the toxicities of breast cancer therapy. When women are diagnosed and going through treatment, it’s overwhelming. We don’t want to add unnecessary cardiovascular testing and worry for anyone. We have a very general idea of the subgroup of women who are affected, but it needs to be further refined.
We’re also studying the best ways to react when these women develop heart problems. Does the cancer treatment have to stop, or can it continue? And if we can continue it, what are the best drugs to protect the heart during that time?
The other question we’re addressing is, once a woman survives breast cancer and is years down the road, are there measurable differences in her heart function due to the cancer therapy? We’re doing very elaborate exercise tests and cardiac-imaging procedures to see if women who survive breast cancer are in fact different from a hearth-health perspective than control patients. Are there differences in their muscle strength, in their lung capacity, in the strength of their heart function?
How many women are affected with heart problems after breast cancer treatment and why does it happen?
Anthracyclines, like doxorubicin, and trastuzumab [Herceptin®] are the main culprits. Other drugs like pertuzumab [Perjeta®] do not seem to add to heart toxicities. But those two medications are the key elements of therapy for HER2-positive breast cancer. With the combination of anthracyclines and trastuzumab, somewhere between 2% and 4% of women develop heart failure. But between 10% and 20% develop heart function problems that are not serious enough at that time to produce heart failure. We’re trying to figure out ways of identifying women who’d be less likely to develop that complication. If they do develop it, we’re studying how to effectively treat them so they can finish their cancer therapy. The answer is not giving less cancer therapy, but it may be giving different cancer therapy. There has been a lot of collaboration between the Cardiology and Breast Medicine services at MSK — especially between breast cancer oncologist Chau Dang and cardiologist Anthony Yu — to make breast cancer therapy more safe and effective.
How is monitoring for heart problems different in women who currently have breast cancer versus survivors?
If she’s still having treatment, we’re trying to treat her with these heart drugs while continuing cancer therapy, so our surveillance is ramped up. We monitor her very closely.
When a woman has recovered from cancer treatment, it’s a little easier. We as heart doctors don’t have to deal with the other side effects of breast cancer therapy, like loss of appetite, fatigue, anemia, and so on. We just have to focus on the heart.
Are there steps a woman with breast cancer can take to keep tabs on her heart health?
Each woman is the best diagnostic and therapeutic instrument we have right now. For example, consider a 50-year-old woman who shows up in an emergency room because she is short of breath and wheezing. The doctors might say it’s bronchitis, pneumonia, or the flu, but it’s really heart failure. If the woman says, “I’m taking a drug that can cause heart failure,” then instead of being treated with a Z-Pak [a type of antibiotic] and steroids, she’ll get the proper treatment. Trying to be well-educated on heart health is really important.