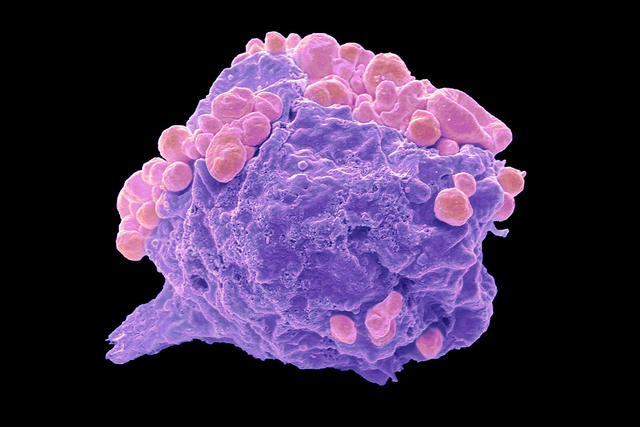
Lymphoma begins in the infection-fighting white blood cells of the immune system. Peripheral T cell lymphoma is an aggressive type of this disease. (Steve Gschmeissner/Science Source)
Peripheral T cell lymphoma (PTCL) is a rare, aggressive type of non-Hodgkin lymphoma. In November 2018, treatment for this blood cancer took a major step forward when the US Food and Drug Administration approved a combination therapy for people newly diagnosed with the disease.
The combination therapy involves adding a drug called brentuximab vedotin (Adcetris®) to chemotherapy. In the phase III clinical trial that led to the approval, the treatment combination more than doubled the time in which the disease didn’t worsen and also helped people with PTCL live longer.
We spoke with Memorial Sloan Kettering medical oncologist Steven Horwitz, who played a leading role in the trial, about what went into this research and what it means for people with PTCL.
How will this new approval change the treatment of PTCL?
For two decades, there has been little change in treatment for people newly diagnosed with PTCL. The standard therapy has been a chemotherapy combination known as CHOP, which is named after the drugs in the mixture. Doctors had tried an intensified variation of that regimen, but it didn’t produce any clear-cut improvement in long-term effectiveness.
That’s what makes the results from this trial so striking. Adding brentuximab vedotin to standard chemotherapy made a huge difference in progression-free survival, which is how long a person lives without the cancer growing. In people who received the combination, progression-free survival was a median of 48 months. In those who received only CHOP, it was 21 months. There was also an increase in overall survival. More people who received the brentuximab vedotin combination were alive after three years.
What does brentuximab vedotin do?
The drug is a monoclonal antibody that targets a protein, CD30, found on some cancer cells. It is already approved for treating Hodgkin lymphoma. The clinical trial tested its effectiveness in people whose PTCL cells expressed CD30. The side effects included nerve damage, nausea, and diarrhea. They were not too severe for most people and are similar to the side effects of CHOP and other chemotherapy regimens.
What was MSK’s role in the clinical testing of this combination?
MSK played a big role in the background research, including helping lead a study several years ago that looked at brentuximab vedotin for the treatment of other T cell lymphomas. Those results gave us the rationale to do this big phase III trial, called ECHELON-2, testing it in people with PTCL. The trial involved more than 400 people. MSK enrolled more patients than any other institution in the new trial, both at Memorial Hospital and at MSK Commack on Long Island. We reported the results of the trial in December at the annual meeting of the American Society of Hematology and in The Lancet soon after. So MSK played a leading role, but it was truly a worldwide effort. More than 140 institutions enrolled patients.
When did you realize this new treatment approach was helping patients?
It was a double-blind study. That means neither the doctors nor patients knew which treatment was being given to a specific person in the trial. In late September 2018, I flew out to Seattle to look at the data when it was finally unblinded. Seattle Genetics, the company that makes brentuximab vedotin and sponsored the trial, was hosting researchers to analyze the data and start writing up the results. I got there late on a Friday night, and it was not until then that I learned that adding brentuximab vedotin not only improved progression-free survival but also overall survival. The improvement in overall survival was the big surprise — it was a dramatic benefit we were not expecting and had never before been shown in a frontline study of T cell lymphoma.
The results were so conclusive and of immediate importance to doctors and patients that it led to one of the fastest ever FDA approvals. It was about six weeks from when the trial data were revealed to approval on November 16. The combination approach using brentuximab vedotin is now available to all newly diagnosed adults with a PTCL subtype called anaplastic large cell lymphoma, which is characterized by CD30 expression. It is also approved for people who have any other CD30-expressing PTCL.
What’s next for this research?
We are taking a closer look at the data to get a better understanding of which people with CD30-positive cancer will do well with the brentuximab vedotin combination and who might need additional therapy.
We don’t have evidence that people whose lymphoma is CD30 negative will benefit from this treatment. But our lymphoma research program is looking at identifying people who can benefit from other targeted therapies. Our T cell lymphoma group is particularly focused on using our increased understanding of the biology of T cell lymphoma to identify more-targeted and hopefully more-effective therapies. This trial result is a good proof of principle for what we’re trying to do, which is develop more individualized and potent therapies for specific lymphoma subtypes.



