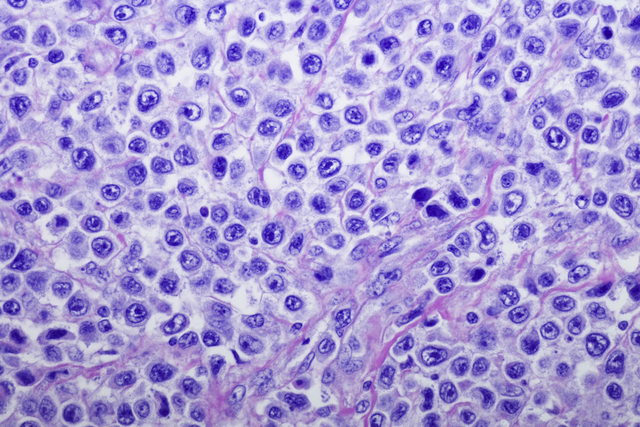
Diffuse large B cell lymphoma is the most common type of non-Hodgkin lymphoma. A combination drug strategy holds potential for slowing or stopping this fast-growing blood cancer.
Diffuse large B cell lymphoma (DLBCL), an aggressive cancer of the white blood cells, is the most common form of non-Hodgkin lymphoma. Researchers looking to slow or reverse this cancer have zeroed in on one particular target, a protein called BCL2. Excessive amounts of BCL2 can help lymphoma cells survive.
In 2016, the US Food and Drug Administration approved a BCL2-targeted drug, venetoclax (Venclexta®), for chronic lymphocytic leukemia. It and similar drugs are being tested in other BCL2-dependent blood cancers. Researchers have had especially high hopes for using BCL2 inhibitors to treat people with different types of lymphoma. But BCL2-targeted drugs have been disappointing in people with DLBCL. In most cases, the tumors resist the treatment.
Now a team led by Anas Younes, Chief of Memorial Sloan Kettering’s Lymphoma Service, has discovered why DLBCL resists BCL2 inhibitors. The researchers have also developed a strategy for overcoming this resistance, and it appears to be effective in cell lines in the lab and mice. The approach involves combining BCL2 inhibitors with a second drug. The pairing will be tested in people with DLBCL within the next year.
The findings are reported in the Proceedings of the National Academy of Sciences.
Blocking Two Disease Pathways
The researchers discovered that in DLBCL tumors, BCL2 has a backup actor — a protein called MCL1. Blocking BCL2 alone is not enough to kill most tumors because MCL1 can pick up the slack. The team showed that in human DLBCL cells and mouse models for the disease, blocking both proteins with a combination of two drugs effectively killed the tumors.
Intriguingly, the team also found an alternative way to make DLBCL cells sensitive to BCL2 inhibitors. They studied a wide range of lymphoma cells treated with BCL2 drugs and looked for the few that actually responded. They identified two types of DLBCL cells that are sensitive to treatment with a BCL2 inhibitor alone. These cells had high levels of a protein called NOXA, a natural inhibitor of MCL1.
The researchers speculated that spurring higher production of NOXA in tumors might be as effective as trying to inhibit MCL1 directly. One way to boost NOXA production is through a class of drugs called HDAC inhibitors. In further studies with cell lines and mouse models, the research team showed that HDAC inhibitors made DLBCL cells vulnerable to the effects of BCL2 inhibitors.
“This suggests that combining BCL2 inhibitors with either MCL1 inhibitors or HDAC inhibitors could also be effective in people with DLBCL,” Dr. Younes says. “We don’t know which approach will work best or which type of inhibitor will be less toxic to people. It’s clearly better to have more than one treatment option.”
Broad Therapeutic Potential
Dr. Younes explains that blocking HDACs may provide added benefits. HDAC inhibitors not only neutralize MCL1, they also tamp down the effects of another protein called MYC, which promotes lymphoma and other cancers. In fact, people whose DLBCL has genetic changes in both of these proteins — known as double-hit lymphoma — have the worst prognosis. So a drug combination targeting HDAC and BCL2 could theoretically offer a better outcome.
Dr. Younes says that the clinical trial will combine a BCL2 inhibitor with an HDAC inhibitor in people whose double-hit DLBCL has returned after initial treatment. He expects the phase I/II trial to begin at MSK sometime in 2019.
“We’re very excited about these findings and the potential of the combination approach,” he says.
This work was supported by NIH Grant P50 CA192937 (MSK Lymphoma SPORE) and by National Cancer Institute Cancer Center Support Grant P30 CA008748, Cycle for Survival, and the Marie-Josée and Henry R. Kravis Center for Molecular Oncology. The study was funded in part by a research grant from Servier, which provided a BCL2 inhibitor used in the experiments. Dr Younes received research funding for clinical trials from both Servier and Novartis.


