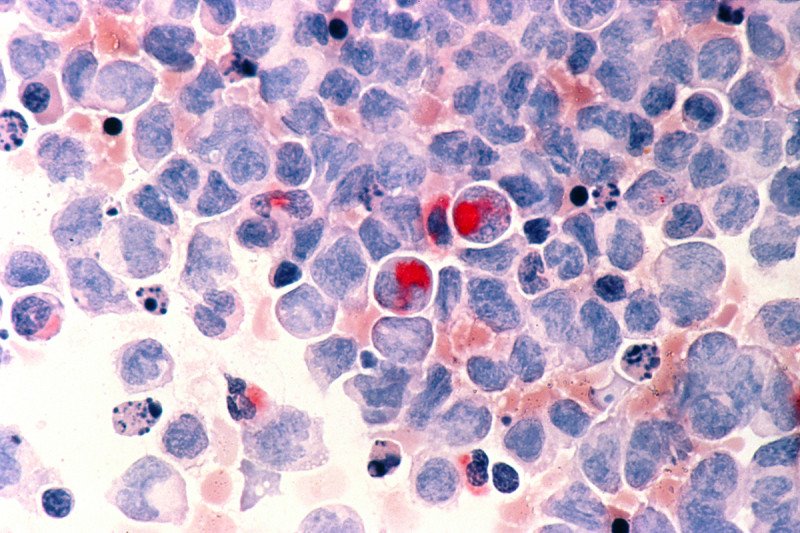
Researchers are learning how acute myeloid leukemia cells develop resistance to chemotherapy.
Doctors have used chemotherapy to treat people with cancer for decades, but there is still much to be learned about how it works — and why it doesn’t always work. In particular, not much is known about the molecular mechanisms that enable some tumors to develop resistance to treatment with chemotherapy drugs.
A new study led by Memorial Sloan Kettering physician-scientist Ross Levine is providing clues about how acute myeloid leukemia (AML), the most common acute leukemia in adults, can become resistant to a common chemotherapy drug. The research has also allowed investigators to develop a more accurate mouse model of the disease, which will help them to gain a greater understanding of how it can be treated with new therapies.
“Despite the fact that we use chemotherapy every day, we understand very little about why it’s not always effective,” says Dr. Levine, who was co-senior author of the study, published recently in the journal Nature Medicine. “We’re finding that cancer cells use different approaches to develop resistance. These novel insights are giving us some paths forward that we can explore with new treatments.”
Focus on a Common Mutation
In the study, the researchers focused on a mutation in the gene DNMT3A, which is present in about one-third of all AML cases. Previous studies have shown that chemotherapy is not very effective against leukemia cells that have this mutation compared with other subtypes that don’t.
“Chemotherapy normally damages cancer cells, but we showed that here, the mutation allows these cells to avoid its effects,” Dr. Levine explains.
The mechanism that allows the mutant cells to evade the damage lies in epigenetics — the chemical modifications of a cell’s genetic material that can modulate gene expression. In this case, the epigenetic mechanism is based on how DNA is packaged inside the cell.
“Normally when chemotherapy damages DNA, cells unreel their genetic material to correct the defects. This unreeling lets the cell know that DNA has been damaged, leading cells to either repair the defect or to undergo programmed cell death,” Dr. Levine says.
Cells with this mutation in DNMT3A can’t do this. “If you can’t unreel the DNA, the leukemia cells can’t recognize the damage. They continue to grow and divide, making the chemotherapy ineffective,” he adds.
Modeling Disease in Mice
Now that the investigators have a better understanding of the mechanism, they can begin to develop new approaches to target it. One way they can do that is through the creation of mouse models that are genetically engineered to carry the DNMT3A mutation.
“Using this animal model, our next step will be to better understand the molecular circuitry that causes the leukemia and why that leads to a progression of the disease in patients,” Dr. Levine says. “More importantly, this will enable us to use a precision oncology approach to develop drugs that are effective against this common subtype of AML.”
A Collaborative Effort
Dr. Levine explains that this work is particularly exciting because it links two initiatives he’s involved with at MSK: the Center for Hematologic Malignancies, which studies whether and how patients respond to treatments for blood cancers, and the Center for Epigenetics Research, which brings together scientists and clinicians with different areas of expertise to study this growing field.
He also credits his postdoctoral fellow, Olga Guryanova, who was the study’s first author, and his collaborators, including co-senior author Siddhartha Mukherjee, a physician-scientist at Columbia University Medical Center and Pulitzer Prize–winning author of The Emperor of All Maladies: A Biography of Cancer.
“This is the kind of research that’s not possible without a lot of collaboration because there are so many different aspects — from collecting patient samples to engineering mouse models to fundamental epigenetics research,” he says.