This information will help you get ready for your procedure to have fiducial (fih-DOO-shul) markers placed in your prostate. It also explains what to expect before, during, and after your procedure. You will have this procedure before you start your radiation therapy.
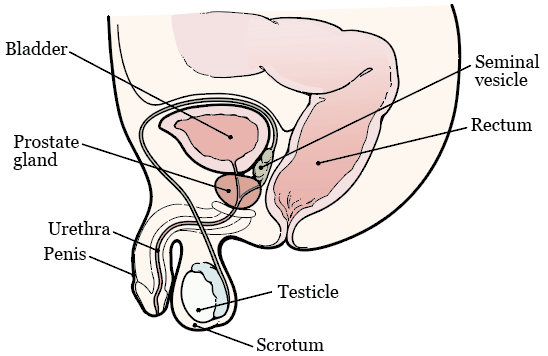
Your prostate is a walnut-sized gland. It’s found below your bladder, right in front of your rectum (see Figure 1). It surrounds your urethra, which is the tube that drains urine (pee) from your bladder. Your prostate adds fluid to your semen (ejaculatory fluid).
About Fiducial Markers
Fiducial markers are tiny metal objects, about the size of a grain of rice. They help your healthcare provider line up the beams of radiation. This makes sure your radiation therapy is delivered the same way each time. The fiducial markers also help your healthcare provider target the tumor and avoid any healthy tissue that’s near it.
The fiducial markers will stay in your prostate after your treatment. Having fiducial markers in your prostate is not harmful to you or your health.
Your appointment to have fiducial markers placed in your prostate is scheduled for
___________________ (date) with
___________________ (healthcare provider).
Before Your Procedure
Tell your healthcare provider if you:
- Take an anticoagulant (blood thinner). Read the “Ask About Your Medications” section for examples.
- Take any steroids medications (such as prednisone).
- Take any dietary supplements (such as vitamins, herbal supplements, or natural or home remedies).
- Have taken any antibiotics in the past 3 months. An antibiotic is a medication to help prevent an infection.
- Have ever had an infection or had to stay in the hospital after a prostate biopsy.
- Have any heart problems.
- Have any implanted devices (such as knee or hip replacements).
- Are allergic to the antibiotic ciprofloxacin (Cipro®) or any other medications.
- Have had a urinary tract infection (UTI) in the last month.
- Have had Achilles tendon injuries or tendonitis (inflammation of your tendons).
- Have trouble hearing.
- Work in a hospital or nursing home.
Get Your Supplies
- 1 saline enema (such as a Fleet® saline enema). You can buy this at your local pharmacy without a prescription.
- Oral antibiotic, if your healthcare provider tells you to. An oral antibiotic is an antibiotic that you swallow. If you’re taking an oral antibiotic, your healthcare provider will send a prescription to your pharmacy. Read the “Antibiotics” section for more information.
Plan How You’re Getting Home
Some people may feel lightheaded (like they might faint) after their procedure. It’s best to have someone take you home after your procedure. They can help you if needed.
Ask about your medications
You may need to stop taking some of your medications before your procedure. Talk with your healthcare provider about which medications are safe for you to stop taking. We’ve included some common examples below.
Blood Thinners
Blood thinners are medications that affect the way your blood clots. If you take blood thinners, ask the healthcare provider performing your procedure what to do. They may recommend you stop taking the medication. This will depend on the type of procedure you’re having and the reason you’re taking blood thinners.
Examples of common blood thinners are listed below. There are others, so be sure your care team knows all the medicine you take. Do not stop taking your blood thinner without talking with a member of your care team.
|
|
Follow your healthcare provider’s instructions for taking aspirin
Aspirin can cause bleeding. If you take aspirin or a medicine that has aspirin, you may need to change your dose or stop taking it 7 days before your procedure. Follow your healthcare provider’s instructions. Do not stop taking aspirin unless they tell you to.
To learn more, read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil (www.mskcc.org/pe/check-med-supplement).
Stop taking nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs, such as ibuprofen (Advil® and Motrin®) and naproxen (Aleve®), can cause bleeding. Stop taking them 2 days before your procedure. If your healthcare provider gives you other instructions, follow those instead.
To learn more, read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil (www.mskcc.org/pe/check-med-supplement).
The Day of Your Procedure
- Give yourself a saline enema the morning of your procedure. Follow the instructions in the package.
- Eat and drink like you usually do. If you do not eat before your procedure, you may feel dizzy or lightheaded after the procedure.
Antibiotics
You will need to take an antibiotic to prevent infection from the procedure. Your healthcare provider will tell you which antibiotic to take. They will send a prescription to your pharmacy before your procedure. You will take one of these antibiotics.
Oral Antibiotics
- Ciprofloxacin (Cipro®) 500 milligrams (mg): You will need to take 2 doses of this antibiotic. For your first dose, take 1 tablet 2 hours before your procedure. You will take your second dose after your procedure. Instructions for taking your second dose are in the “After Your Procedure” section.
- Cefixime (Suprax®) 400 milligrams (mg): Take 1 tablet 2 hours before your procedure.
- Cefuroxime (Ceftin®) 500 milligrams (mg): You will need to take 2 doses of this antibiotic. For your first dose, take 1 tablet 2 hours before your procedure. You will take your second dose after your procedure. Instructions for taking your second dose are in the “After Your Procedure” section.
Intravenous (IV) Antibiotics
Your healthcare provider may decide you need intravenous (IV) antibiotics instead of oral antibiotics. If they do, you will get the IV medication through a vein in your arm. You will get the IV medication 1 hour before your procedure.
During Your Procedure
First, your healthcare provider will gently put a probe (wand) into your rectum. They will put an anesthetic (numbing) lubricating gel on the probe to help it slide in more easily. They may also give you an injection (shot) of a local anesthetic to numb the area around your prostate.
The probe uses ultrasound (sound waves) to make images of your prostate. It also has a thin needle attached to it. Your healthcare provider will use the ultrasound to help them guide the needle. They will use the needle to place 3 fiducial markers into 2 different areas of your prostate. Once your healthcare provider has placed the fiducial markers, they will remove the probe and needle.
This procedure will take about 15 minutes. Before you leave the clinic, your healthcare provider will tell you how to care for yourself at home.
After Your Procedure
Medication Instructions
If you’re taking an oral antibiotic, follow these instructions. This will help prevent an infection in your prostate.
- Ciprofloxacin (Cipro®) 500 mg: For your second and final dose, take 1 tablet 12 hours after your first dose.
- Cefuroxime (Ceftin®) 500 mg: For your second and final dose, take 1 tablet 12 hours after your first dose.
It’s normal to have some soreness after your procedure, but most people do not have pain. If you feel sore, you can take acetaminophen (Tylenol®). If the acetaminophen does not help, call your healthcare provider.
Eating and Drinking
You can go back to your usual diet right away after your procedure. For 3 days after your procedure, try to drink double the amount of liquids that you usually drink. This will help flush out your bladder, prevent infection, and reduce the amount of blood in your urine. It will also make your bowel movements (poop) softer, which helps keep your rectum from getting irritated.
Short-Term Side Effects on Your Bowel Movements, Urine, and Semen
- You may see blood in your bowel movements. You may also have a small amount of bleeding from your rectum. These things can happen when you have a bowel movement. They may happen right after your procedure or for a few days after.
- You may see blood in your urine for 7 to 14 days after your procedure. This bleeding may come and go.
- Your semen may look rust-colored for up to 12 weeks after your procedure. This is because small amounts of blood may be in it.
Physical Activity and Exercise
- Do not take part in any sexual activity for 3 days after your procedure.
- For the next 5 to 7 days after your procedure, do not:
- Play any sports.
- Work out in a gym.
- Ride a bicycle.
- Lift or carry anything heavier than 10 pounds (4.5 kilograms).
When To Call Your Healthcare Provider
Call your healthcare provider right away if you have:
- Heavy bleeding out of your rectum.
- Bleeding out of your rectum that will not stop.
- Blood in your bowel movements.
- Trouble urinating (peeing).
- Bright red blood or large blood clots in your urine.
- A fever of 101 °F (38.3 °C) or higher.
- Chills.
- Dizziness.
- Increasing pain or pain that does not get better after taking over-the-counter pain medication.