Welcome and Overview
This guide is designed to help you and your loved ones understand what to expect throughout your transplant journey. The information in this guide isn’t meant to replace the information that your transplant team will teach you. It’s meant to be a resource that you can refer to throughout the transplant process.
In this guide, we’ll explain some of the challenges you might have over the course of your transplant and recovery. This doesn’t mean you’ll have all of them. You should not compare yourself to other people you know or have heard of who had a stem cell transplant. Everybody is unique.
Stem cell transplants have been done for many decades. They have gotten much better over that time. But a stem cell transplant is still a complex procedure that requires a commitment from you, your family or caregiver, and your transplant team.
Having a transplant is a long process. Getting ready for your transplant is just the first part of your journey. You’ll need to stay within 1 hour of MSK for about 100 days (3 months) after the day of your transplant, even after you’re discharged from the hospital. If you live farther than 1 hour from the hospital, we can help you arrange for a place to stay closer to MSK. Overall recovery time is different from person to person, but you should plan to allow about 1 year for full recovery. All these things will be discussed in more detail in this guide.
At MSK, you’ll have a large transplant team working together to care for you as you go through each phase of your transplant. It’s normal to have many emotional changes during the transplant process. Your transplant team includes many healthcare providers. They include social workers, chaplains, psychiatrists, and members of our Integrative Medicine Department. All these healthcare providers are available to support and help you and your caregiver(s) cope with what you may feel.
The Importance of Communication
Throughout your transplant journey, it’s very important to communicate clearly with your transplant team and caregiver about how you’re feeling. If anything is bothering you, even if it seems small, tell a member of your transplant team. This is true for how you’re feeling both physically and emotionally. It’s very important not to let things build up. If you do, small problems can grow into larger problems. The more information you communicate to your transplant team, the more they can help you. There’s usually something they can do to make you feel more comfortable.
Below are some of the ways you can communicate with your transplant team:
- While you’re an outpatient, call your healthcare provider’s office. Between and Monday through Friday, your healthcare provider’s office coordinator will answer and give your message to the right person. This may be your doctor, nurse, clinical nurse coordinator, or social worker. After , on weekends, and on holidays, MSK’s answering service will answer your call. Ask to talk with the hematology fellow on call.
- While you’re in the hospital, tell a member of your transplant team. Your transplant team will see you at least once a day. You’ll also see your primary nurse throughout the day. Talk with them about any issues during this time.
- Use your MyMSK account. MyMSK is MSK’s patient portal. You can use MyMSK to ask questions about your appointment schedule, request a prescription refill, or request patient education information. Never use MyMSK to communicate any symptoms to your transplant team. You’ll get more information about MyMSK at your initial consult visit. You can also read the resource Communicating With Your Care Team: When to Call or Use MyMSK (www.mskcc.org/pe/communicating_using_mymsk).
About PROMIS
Your transplant team will also use MyMSK to check in about how you’re feeling physically and mentally over time. The set of questions they’ll send is called PROMIS. Your transplant team will send PROMIS questions to your MyMSK account:
- On or near the day you start treatment.
- On the day of your stem cell infusion.
- Every 7 days for the first month after your stem cell infusion.
- Every month for the first year after your stem cell infusion.
- Every 3 months for the second year after your stem cell infusion.
You may report concerning symptoms when you’re filling out the PROMIS questions. You’ll then see a message asking you to call your care team. Or, a member of your transplant team will call you to help. Your answers will also help us know how people generally feel after an allogeneic stem cell transplant so we can improve our care in the future.
How to Use This Guide
There’s a lot of information to read and understand in this guide. Read the entire guide at least once, including the additional resources. You may find it easier to read a few sections at a time rather than trying to read the entire guide at once. We encourage you to refer to this guide as your treatment progresses.
We recommend that you highlight or write notes on anything that you don’t understand or have a question about. There’s no such thing as a silly question, so please ask about anything that’s on your mind.
Stem Cell and Bone Marrow Basics
Hematopoietic (hee-MA-toh-poy-EH-tik) stem cells (usually just called stem cells) are immature cells that grow into all the blood cells in your body. The white blood cells fight infection, red blood cells carry oxygen, and platelets help control bleeding. Your stem cells are always dividing and changing into these different types of blood cells to replace older blood cells. Stem cells also divide to make newer stem cells.
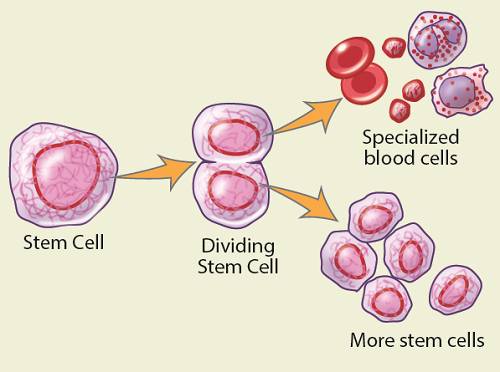
A stem cell transplant means that the stem cells are taken from either the donor’s bone marrow or their bloodstream.
Most of the stem cells in your body are in your bone marrow (the soft tissue in the spaces in the center your bones). Bone marrow is mostly found in the larger bones in your body, such as your hip, breastbone, and pelvis. A few stem cells are also found in your bloodstream.
You might hear your transplant called a stem cell transplant or a bone marrow transplant. A bone marrow transplant is a specific type of stem cell transplant. With a bone marrow transplant, the stem cells are taken from the bone marrow. With a stem cell transplant, the stem cells are taken from either the bone marrow or the bloodstream.
Understanding Your Allogeneic Stem Cell Transplant
When you have an allogeneic stem cell transplant, stem cells are harvested (collected) from a donor. “Allogeneic” means that the stem cells come from someone else. The 3 general sources of stem cells that can be used in an allogeneic stem cell transplant are:
- Peripheral blood stem cells. These are collected from a donor’s bloodstream through a process called apheresis (a-feh-REE-sis). To increase the amount of stem cells in their bloodstream, the donor will get injections (shots) of a medication that causes their body to make more stem cells than usual. The stem cells escape from their bone marrow into their bloodstream, where they can be collected easily while the donor is awake.
- Bone marrow stem cells. These are collected from a donor’s bone marrow through a procedure called bone marrow harvesting. The procedure is done in the operating room while the donor is asleep. The donor usually goes home the same day of the procedure.
- Umbilical cord blood stem cells. These are collected from blood from the umbilical cord and placenta when a baby is born. They’re frozen and stored in a cord blood bank until they’re needed for a transplant.
Your Donor
A test called tissue typing is done to find out who is the best donor for you. For a hematopoietic stem cell transplant, the tissue typing is based on your human leukocyte (LOO-koh-site) antigens (HLA). These are markers on the surface of your white blood cells.
There are many HLA markers, and different people can have different patterns of the markers. HLA markers are inherited (passed from a mother and father to their child). Your close family members (siblings, parents, and children) are most likely to have a pattern of HLA markers that’s like yours.
People who aren’t related to each other can also be a close match. If you don’t have a family member with a matching tissue type, we have a team of search coordinators who will look for an unrelated adult volunteer donor or umbilical cord blood units. The National Marrow Donor Program® has millions of people registered who have been typed for this purpose. Searching for a donor can take weeks or even months. Sometimes, umbilical cord blood can be used if the transplant is urgent, because it’s more readily available. If you’ll need stem cells from someone who isn’t related to you, your doctor will give you more information.
Conditioning
Before your transplant, you’ll get treatment to get your body ready, even if your disease is in remission. This is called conditioning. Conditioning is made up of chemotherapy, radiation therapy, or both. It’s done to:
- Kill any remaining cancer cells in your body.
- Make room for the donor stem cells in your marrow spaces.
- Suppress (weaken) your immune system so you can accept the donor stem cells.
There are 2 types of conditioning before an allogeneic transplant.
- With a myeloablative transplant, you’ll get high doses of chemotherapy with or without radiation. These treatments aim to kill your cancer, but they’ll also kill (myeloablate) all the stem cells in your bone marrow. The donor stem cells will then replace the ones killed by the treatment. This type of treatment is very intense and isn’t right for everyone.
- With a nonmyeloablative transplant, you’ll get lower doses of chemotherapy with or without lower doses of radiation. You’ll also take medications to weaken your immune system. The goal of this approach is to weaken your immune system enough to let the donor stem cells take over and make a new immune system that will fight the cancer.
Your healthcare provider will consider many factors when choosing which type of transplant is best for you. These include your disease, other treatments you’ve had, and your overall health. Your healthcare provider will talk with you about these things in detail.
Transplant Infusion
When it’s time for your transplant, the donor stem cells will be infused (put) into your body through a tunneled catheter. A tunneled catheter is a thin tube put into your upper chest. It’s a type of central venous catheter (CVC). You’ll learn more about tunneled catheters in the section “What to Expect While You’re in the Hospital.”
The stem cells may be infused from a bag, like a blood transfusion, or pushed from a large syringe into your tunneled catheter. This will be done in your hospital room.
Engraftment
Almost right away after the stem cells are infused into your body, they’ll travel through your bloodstream to your bone marrow. They’ll start to divide and create healthy new blood cells. Engraftment is when your body accepts the transplant and your blood cell counts start to recover.
Engraftment usually takes about 10 to 14 days. It can take longer, depending on the source of your stem cells. Platelets and red blood cells usually take a little longer to recover than white blood cells.
While you’re waiting for engraftment, you’ll be given injections of growth factor. This is a medication that will speed up the production of white blood cells in your body. You might also need blood and platelet transfusions.
You’ll have a much higher risk of getting an infection after conditioning until engraftment. You’ll need to take precautions, including avoiding sources of infection, washing your hands regularly, and following a food safe diet. When you’re admitted to the hospital, you’ll be given medications to help protect you from certain infections. You’ll be closely monitored for any signs of infection. We will treat you with antibiotics if we think you might have an infection.
Getting Ready for Your Transplant
Your Initial Consultation Visit
During your initial consultation visit, you’ll meet with your healthcare provider and other members of your transplant team. Your healthcare provider will take a complete medical and surgical history and do a physical exam. They will talk with you about what they think is the best treatment plan for you. They may also discuss this plan with other transplant healthcare providers to make sure everyone agrees on the best plan for your specific situation.
Getting Ready for Your Transplant
Before your transplant, you’ll make practical, physical, and emotional preparations for your transplant. Here’s a list of things that will happen and what you can do to get ready:
- Learn about your transplant. The information your transplant team will go over with you is meant to help you learn, not scare you. Make a note of anything that you don’t understand about your transplant. Note anything in this guide that isn’t clear, and any other questions you have.
- Contact your insurance company. It’s a good idea to contact your insurance company before your transplant to see if there’s a case manager for you.
- Choose a caregiver. Identify a family member or friend to act as your caregiver. Make sure this person understands what this role means. Give your caregiver a copy of this guide and ask them to read it at least once.
- Fill out a Health Care Proxy form. A health care proxy is a legal document that identifies the person who will speak for you if you can’t communicate for yourself. The person you identify is called your health care agent. This person can be different from your caregiver. For more information, talk with your social worker or any other member of your transplant team. You can also read the resource .
- Meet with a social worker. Your social worker will explain the psychological, emotional, and financial support services offered by the social work team.
- Arrange for disability or a leave of absence from work. If you’re working, make arrangements to go on disability or take a leave of absence. You should plan to be away from work for about 6 months, but the exact length of time is different for everyone.
- Plan where you’ll stay. You’ll need to stay somewhere located within 1 hour of MSK for the first 100 days after the day of your transplant. Your social worker can help you arrange this, if needed.
- Make decisions about your fertility. If fertility (the ability to have children naturally) is a concern for you, talk with your transplant team about your options. Ask for an appointment with a fertility specialist. Talk with them about how your treatment may affect your ability to have children in the future. Discuss the steps you can take to preserve your fertility. You can also read the resources below for more information.
- Fertility Preservation Before Cancer Treatment: Options for People Born with Ovaries and a Uterus (www.mskcc.org/pe/fertility_starting_treatment)
- Building Your Family After Cancer Treatment: For People Born With Testicles (www.mskcc.org/pe/building_family_born_testicles)
- Sperm Banking (www.mskcc.org/pe/sperm_banking)
- Arrange for childcare and pet care, if needed. If you have concerns about talking with your children about your transplant, your social worker can help guide you.
- Make decisions about your hair. The chemotherapy that kills cancer cells also kills the cells that make your hair. Most people lose their hair during their transplant. Think about if you’d like to cut your hair. If you decide to wear a wig, visit a wig store as soon as you can. That way, you can find one that closely matches your natural hair, if you want to.
- Have your pretransplant evaluation. You’ll have a series of medical tests. Your clinical nurse coordinator will review which tests are needed. Your doctor’s office coordinator will work with you to try to schedule these tests at a time that’s convenient for you.
- Meet with a clinical dietitian nutritionist, if needed. If you have specific nutritional needs, you’ll meet with a clinical dietitian nutritionist to review special dietary requirements and safe food handling. If you want to meet with a clinical dietitian nutritionist, ask your nurse for a referral.
- Meet with a pharmacist. The pharmacist will go over all the medications you’ll take before and after your transplant.
Your Transplant Team
A team of healthcare providers will care for you throughout your treatment. You’ll meet many of them as you progress through your transplant journey. You might not meet some members, such as your doctor’s office coordinator, laboratory staff, or our service coordinator. But they’re all working to help you. Here is a list of your team members and their roles.
- An attending doctor will be in charge of your care throughout your treatment. Even though one specific doctor will be your primary outpatient doctor, different doctors may care you for while you’re in the hospital.
- A fellow is a doctor who has finished general training and is getting more training in cancer care.
- An advanced practice provider (APP) is a healthcare provider who works with your doctor to provide you with care. They can give medical treatments and prescribe medications. Sometimes, you may see them instead of your doctor. APPs include nurse practitioners (NPs), physician assistants (PAs), and certified registered nurse anesthetists (CRNAs).
- A clinical nurse coordinator is a nurse who will communicate and work with you, your caregiver, and your team of doctors. They will organize and schedule testing, procedures, and consultations with other professionals you need before your transplant. Your clinical nurse coordinator will teach you about your specific treatment plan.
- Nursing staff will work with you when you’re seen at outpatient visits and while you’re in the hospital. They’re registered nurses (RNs) specially trained in the care of stem cell transplant patients.
- Each outpatient nurse works with 1 or 2 attending doctors. They will meet you when you have your initial consultation visit. Your outpatient nurse will see you at many of your outpatient visits after discharge. They will follow you along your transplant journey.
- When you’re admitted, you’ll have a team of primary nurses that will care for you during your hospital stay. The inpatient nurses work 12-hour shifts. They will try to be consist about who will be working with you.
- A nursing assistant or patient care technician (PCT) provides basic care and support under the direction and supervision of a registered nurse.
- A hospitalist is a doctor who sees people only while they’re in the hospital. At MSK, there’s a hospitalist on duty all night.
- A clinical pharmacist who is an expert in the care of people having stem cell transplants will review your medications with you and your caregiver. They will teach you how to take them properly, and tell you about any side effects they might cause.
- A social worker will help you, your family, and your friends manage the stress that comes with the transplant process. Social workers understand the issues faced by people having transplants. They are available to listen, offer counseling, and refer you or your loved ones to other resources and services.
- A transplant service coordinator will work with you and your insurance company to determine your transplant benefits. This person is familiar with the insurance issues faced by people having transplants. Each insurance company has its own policies and requirements. When your insurance company needs authorization, your transplant service coordinator will help with that process.
- Office coordinators give administrative support to your attending doctors and their nurses. You might talk with them when you give us information, schedule an appointment, or have questions for your transplant team. Office coordinators are sometimes called physician office assistants (POAs).
- Care coordinators work in the outpatient areas and monitor the flow of patients in and out of the clinic. They make sure patients either schedule or complete all of the tests, scans, and treatments the care team orders. Care coordinators also manage patients’ medical records and coordinate their future appointments. Care coordinators are sometimes called session assistants (SAs).
- An unrelated donor search coordinator works with staff at the National Marrow Donor Program to find a donor for people who don’t have a donor in their family. They’ll give updates to your doctor about the search results often.
- A clinical research coordinator works with your transplant team. They will talk with you and explain some of the research studies, also called clinical trials, that you may be able to join at MSK. These studies don’t include anything related to your particular treatment. They mostly concern collecting samples or data. Clinical research coordinators are sometimes called research study assistants (RSAs).
- Patient representatives are the connection between patients and families, and the hospital staff. They’re here to protect your rights and help explain hospital policies and procedures. Patient representatives can help you with any concerns about your care. They can help you communicate with members of your transplant team.
- A clinical dietitian nutritionist is a food and nutrition expert who will assess your nutritional status and talk with you and your caregiver about your diet. They will give you advice about changing your diet to help manage your symptoms and side effects.
- A physical therapist (PT), occupational therapist (OT), or both will see you while you’re in the hospital. They’ll work with you to help you keep up your strength and stamina during your recovery.
- A room service associate will explain how the room service works, including the hours it’s available and how to use it. They’ll make sure you get the right menus and deliver your meals.
- A case manager will see you while you’re in the hospital and give your health insurance company the updates it needs. They help you arrange home care, as needed.
Your Caregiver
An important step in getting ready for your transplant is choosing your caregiver. Your caregiver will be an important part of your transplant team. This person is usually a family member or a close friend.
Your caregiver will be responsible for some of the medical, practical, and emotional support you need during your transplant. This person needs to be available 24 hours a day, 7 days a week once you’re discharged. Some of your caregiver’s responsibilities will include:
- Medical support
- Noticing any changes in your condition.
- Telling your transplant team about any new symptoms you have.
- Telling your transplant team about any changes in your condition.
- Calling for medical help in an emergency.
- Practical support
- Dealing with financial and insurance issues.
- Keeping family members and friends up to date about your condition.
- Managing the number of visitors you have.
- Keeping you away from anyone who’s sick.
- Grocery shopping and preparing meals.
- Laundry and cleaning.
- Emotional support
- Paying close attention to your moods and feelings.
- Communicating with you and listening to you.
- Understanding your needs and decisions.
You may not have just 1 person who can act as your caregiver. It’s OK to have different caregivers scheduled during different times. It’s best to limit the number of caregivers to 2 or 3 people, if you can.
It’s important for your caregiver to stay positive, calm, and flexible while giving you with the support and encouragement you need. It’s also important for you to understand the caregiver role is challenging. At times, your caregiver may feel overwhelmed by the responsibilities.
Take time now to think about who you want to be your caregiver. It should be somebody you trust and who can take the time to care for you. Your caregiver should be someone who can offer you the practical and emotional support you need.
If your caregiver gets sick or shows any signs of a cold or flu (such as a cough, fever, or sore throat) 1 week before or at any time during your transplant, tell your transplant team right away.
Resources for caregivers
Caregivers can have physical, emotional, spiritual, and financial distress. Resources and support are available to help manage the many responsibilities that come with caring for a person having a transplant. For support resources and information, contact your transplant social worker. You may also find the resource helpful.
At MSK, our Caregivers Clinic provides support specifically for caregivers who are having a hard time coping with the demands of being a caregiver. For more information, call Dr. Allison Applebaum at 646-888-0200 or go to www.mskcc.org/cancer-care/doctor/allison-applebaum.
Coping with Separation from Your Children
Whether you’re inpatient or outpatient, being apart from your children will be hard for you and your family. We strongly recommend that you talk with your social worker about your concerns and develop a plan to maintain strong ties to your children during your transplant.
Below are some things that others have done to remain in contact with their children during their transplant.
- Talk with your children regularly using programs or apps like Skype, Google Hangouts, or FaceTime. Set up a time that you talk to them each day, such as when they get home from school and before they go to bed. Get into a routine of using the computer to see and talk to them.
- Paint or create other crafts to send home. Ask a member of your transplant team to arrange for volunteers from the Patient Recreation Center to bring you supplies.
- Use your cell phone or a tape recorder to record yourself reading your children’s favorite stories. Upload these recordings to the web, give them to your caregiver, or e-mail them to your children. They can read along with these stories while listening to your voice.
- Keep copies of your children’s favorite stories with you in your hospital room. At night, you can use Skype to read along with them before they go to sleep.
- Decorate your hospital room with your children’s artwork and pictures of your family.
- Give your children a special coloring book or journal for times when they miss you or when feelings are difficult. Your caregiver can bring the colorings to you. You can talk with your child about them over Skype or on the phone.
We know that nothing will replace physical contact between you and your children, but we strongly encourage you to use all of the technology that’s available to maintain a strong bond with them while you’re away.
For more help maintaining your relationship with your children, contact your social worker.
Your Pretransplant Evaluation
Before you become a transplant candidate, your overall physical condition will be evaluated. You’ll need to make several trips to MSK to have tests. We often call this the “work-up” or “restaging” period. During the work-up, you’ll need to have some, but not always all, of the following tests.
- Chest x-ray. This is done to make sure your lungs are clear and there’s no sign of infection or other problems.
- Blood tests. These are done to check several things, including your kidney function, liver function, blood counts, and past exposure to certain viruses.
- Urine test. This is done to see if there’s anything abnormal in your urine (pee).
- Electrocardiogram (EKG) and echocardiogram (echo). These are done to give your transplant team information about your heart.
- Pulmonary function tests (PFTs). These are breathing tests that measure how well your lungs work.
- Computed tomography (CT) scan. This is a radiology test that gives more detailed images of soft tissue and bone than a standard x-ray. Sometimes, CT scans use contrast dye that you drink or have injected into your veins. It’s very important to tell your doctor if you know you have an allergy to contrast dye, seafood, or iodine. If you have a mild allergy, you can still have contrast dye, but you’ll need medications before getting the dye to prevent a reaction.
- Positron emission tomography (PET) scan. This is a radiology test that’s used to look at certain types of cancer, as well as your organs and how they work in your body.
- Dental exam. You must have a full dental exam before your transplant. Any cavities, loose fillings, or gum disease should be taken care of before your transplant. This can be done by your own dentist or by a dentist here at MSK. If you see your own dentist, ask for a letter saying that you have no dental problems. If there are issues, ask your dentist to contact your healthcare provider’ office to discuss them. Your dental exam can be done up to 3 months before you’re admitted to the hospital for your transplant.
- Bone marrow aspiration and biopsy. A bone marrow aspirate is a small sample of bone marrow, usually taken from the back of your hip. Your hip will be numbed, a needle will be put into the bone marrow, and a small amount of bone marrow liquid will be taken out. A bone marrow biopsy might be done at the same time. This biopsy involves collecting a tiny piece of bone for examination. This is done to check how well your bone marrow is making cells and to look for any sign of cancer in the marrow.
- Lumbar puncture (spinal tap). This is done to check for abnormal cells in your cerebrospinal fluid (CSF). This is the fluid that surrounds your brain and spinal cord. A small needle will be put through your back and a small amount of CSF will be collected. A lumbar puncture is only done for certain types of leukemia and lymphoma. Sometimes, chemotherapy is injected into your CSF to keep the cancer from spreading there or to treat cancer if it’s already there.
- Skeletal survey. This is done to look for bone damage caused by cancer. It’s usually only done for people who have multiple myeloma. It involves taking x-rays of the major bones in your body. It can take a few hours.
- Consultation with a radiation oncologist. If you’re having radiation therapy as part of your conditioning, you’ll meet with your radiation oncologist to go over your treatment plan. You might also have a CT scan, PET scan, or both during this visit. They’ll be used to plan your treatment. You’ll also have a treatment planning session called a simulation. During this session, several imaging scans are taken, along with measurements of your chest. These are used to make lead shields. Your lungs are very sensitive to radiation and the shields will be used to protect them during some of the treatments.
These tests are usually done in the 30 days before your transplant (Day −30 onwards), but sometimes the pretransplant evaluation can take longer. Your clinical nurse coordinator will work with you and your caregiver to schedule the tests. The results of the tests will be used to plan your treatment and make sure it’s safe to start your treatment.
Your healthcare provider will explain any other tests that you might need.
Donor Screening
Around the time you’re having your pretransplant evaluation, the donor will be going through the screening process. If the donor is related to you, they’ll be screened at MSK. If the donor is unrelated, they’ll be screened at the local donor center. Donor screening is done to make sure the donor is healthy enough to donate their stem cells.
Stem Cell Harvesting
For an allogeneic transplant, the donor’s stem cells are harvested (collected) from their body, then given to the person receiving the transplant.
Peripheral Blood Stem Cell (PBSC) Harvesting
PBSC harvesting is the procedure used to collect stem cells from the donor’s blood. Before PBSC harvesting, the donor will have mobilization. This is the process of increasing the number of stem cells made by their bone marrow and released into their bloodstream.
After mobilization, the donor’s blood will be collected and separated into its major components (red blood cells, white blood cells, platelets, and plasma). The stem cells will be removed from the other white blood cells and the rest of the blood will be given back to the donor. If you’d like to know more about the PBSC harvesting process, you can read the resource Allogeneic Donor Peripheral Blood Stem Cell Harvesting (www.mskcc.org/pe/allogeneic_pbsc_harvesting).
In general, the donor’s stem cells are collected 1 to 2 days before the transplant. Sometimes, their stem cells are collected at an earlier time and frozen until needed.
Bone Marrow Harvesting
In certain cases, stem cells may be collected from the donor’s bone marrow rather than peripheral blood. This is called bone marrow harvesting. With bone marrow harvesting, mobilization isn’t needed.
Bone marrow harvesting is done in the operating room while the donor is under general anesthesia (asleep). If you’d like to know more about the bone marrow harvesting process, you can read the resource About Bone Marrow Harvesting (www.mskcc.org/pe/bone_marrow_harvesting).
Your Preadmission Appointment
Once your pretransplant evaluation is finished and you have the date of your transplant, you’ll have your preadmission appointment. This appointment is usually 1 to 2 weeks before you’re admitted to the hospital. At this appointment:
- Your healthcare provider will review your treatment plan with you.
- Your healthcare provider will go over the consent forms and you’ll sign consent for your transplant (if you haven’t already).
- You’ll meet with your clinical nurse coordinator. They’ll give you a calendar outlining your treatment plan, review information, and answer your questions.
- You’ll meet with your clinical pharmacist again to review the medications you’ll take during and after your transplant.
- You may be asked to sign a consent form for transfusion (if you haven’t already). This is because you may need blood or platelet transfusions when your blood counts are low after your transplant. For more information about blood transfusions, read the resource About Your Blood Transfusion (www.mskcc.org/pe/blood_transfusion).
Between your preadmission appointment and when you’re admitted to the hospital, it’s very important to call your transplant doctor’s office if you have any of the following:
- Signs of a cold, such as:
- A runny nose
- Congestion
- A cough
- A fever of 100.4 °F (38.0 °C) or higher
- Nausea (feeling like you’re going to throw up)
- Vomiting (throwing up)
- Diarrhea (loose or watery bowel movements)
- A toothache
- An open wound
- Any other new problem, even if it seems small
Your healthcare provider will decide if your admission for transplant should be delayed. It could be very dangerous to start your chemotherapy while you have an infection, even if it’s just a cold. This is because your immune system won’t be able to fight the infection.
Your Hospital Admission
On your admission day, bring a list of all the prescription and nonprescription medications you’re taking, along with the dose you take and how often you take them. The list should include patches, creams, vitamins, nutritional supplements, herbal products, and over-the-counter medications.
You can also bring the following items with you, if you want to:
- Pajamas, sweat pants, or shorts
- Button down or zipper shirts
- Slippers
- Sneakers, socks with traction, or both
- Hat or scarf
- Blanket and pillow from home (brightly colored to distinguish it from hospital linens)
- Photos, posters, or other reminders of home
- Cell phone and charger
- Baby wipes
- Puzzles, books, or magazines
- Notebook and pens and pencils
- A little bit of money
- Radio, iPod, or CD player
- Laptop or tablet (such as an iPad)
Don’t bring the following items with you:
- Your medications (neither prescription nor over-the-counter)
- Things that will clutter up your room
- Flowers or plants
What to Expect in the Hospital
Having Your Tunneled Catheter Placed
You’ll need a tunneled catheter during your transplant. A tunneled catheter is a type of central venous catheter (CVC). It’s a tube that’s put into a large vein in your upper chest (see Figure 2). Outside your body, the catheter divides into 2 or 3 smaller tubes called lumens (see Figure 3).
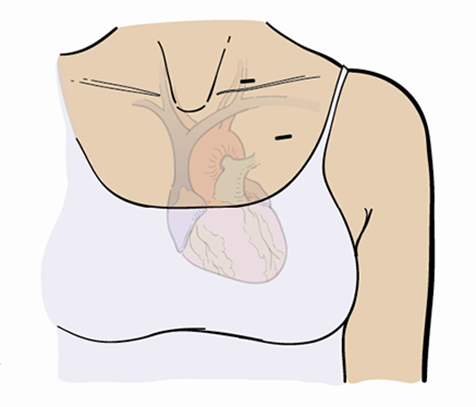
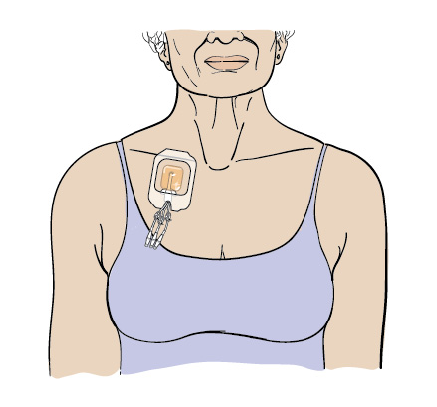
A tunneled catheter lets your transplant team infuse your stem cells, draw your blood, and give you fluids, electrolytes, blood transfusions, chemotherapy, and other medications without having to keep sticking you with a needle. Having a tunneled catheter will make your treatment much more comfortable.
Most people have their tunneled catheter placed on the day they’re admitted to the hospital. Sometimes, it may need to be placed a few days before hospital admission. For more information, read the resource About Your Tunneled Catheter (www.mskcc.org/pe/about_tunneled_catheter).
The procedure to place your tunneled catheter will be done in the Interventional Radiology department at Memorial Hospital (MSK’s main hospital). Your clinical nurse coordinator will talk with you about the details of having your tunneled catheter placed.
After Your Tunneled Catheter is Placed
After your tunneled catheter has been put in, you’ll be monitored until you’re fully awake.
- If your tunneled catheter is being placed on the day you’re being admitted to the hospital, you’ll be taken to the inpatient stem cell transplant unit once you’re fully awake. The inpatient nursing staff will care for your tunneled catheter while you’re in the hospital.
- If your tunneled catheter is put in a few days before you’re admitted to the hospital, you’ll be discharged once you’re fully awake. You must have a caregiver with you if you’re going home after your tunneled catheter is placed. Your nurse will change the dressing, if needed.
Keep your tunneled catheter secure at all times to avoid pulling it. You can tape the lumens of your tunneled catheter to your skin, tuck them into a bra if you wear one, or secure them to your clothing. Ask your nurse about the best way to secure your tunneled catheter. You can find more information about caring for your tunneled catheter in the resource About Your Tunneled Catheter (www.mskcc.org/pe/about_tunneled_catheter).
Your tunneled catheter is usually taken out when you’re discharged from the hospital.
While You’re in the Hospital
There are 2 transplant units in Memorial Hospital. The nurses on each unit are specially trained to care for people having transplants, and all the same guidelines are followed on both floors. You may need to change your room or floor while you’re in the hospital. We try to avoid this as much as possible.
When you’re admitted to the hospital, your inpatient transplant team will take a complete medical history, review your current medications, and do a physical exam. Your inpatient transplant team is made up of an attending doctor and a combination of a fellow, APP, primary nurse, and pharmacy specialist.
Your primary nursing team will care for you during your hospital stay. Nurses usually work 12-hour shifts starting at either or When nursing shifts change, your nurse will share the information about what happened with you and your care during that shift with the nurse taking over.
What to Expect
- You’ll be in protective isolation to lower your risk of getting an infection. Anyone who goes into your room must clean their hands and wear a mask and gloves. For more information, read the resource Hand Hygiene and Preventing Infection (www.mskcc.org/pe/hand_hygiene).
- You’ll be in a private room that has a bathroom for your use only. Your room will have Wi-Fi and a TV with cable channels.
- You’ll be connected to an IV pole with electronic pumps during most of your hospital stay.
- Your vital signs will be taken every 4 hours, even during the night.
- Your urine will be measured daily during your hospital stay. It’s important that we know how much urine you’re making.
Testing and Evaluations
Before every day, a member of your transplant team will weigh you and take a sample of your blood. Your blood will be checked to see how your white blood cells, red blood cells, and platelets are recovering. Other blood tests will be done as needed to check your kidney and liver, monitor for infections, check the level of chemotherapy or other medications in your blood, and to help evaluate your overall condition.
The day you’re admitted to the hospital, every Monday, and right before you’re discharged, your nurse will take a nasal swab for testing. This is to see if you have any bacteria that may cause an infection. If you do, your transplant team will give you information about additional isolation precautions needed.
If you’re at risk of falling, someone will be available to help you go to the bathroom. Your treatment team will tell you more about how to prevent falls. You can also read the resource Call! Don't Fall! (www.mskcc.org/pe/call_dont_fall).
Exercise
Even though you’ll feel tired after your chemotherapy and transplant, you should still try to stay active and get out of bed every day. It’s important to be safe, so ask for help when you get up.
We encourage you to walk around the unit. You must wear a mask and gloves while you’re walking around the unit. Your nurse will tell you if you also need to wear an isolation gown. Don’t leave the floor for walking or exercise.
A physical therapist will evaluate you early during your hospitalization and prescribe an exercise program that’s right for you.
Communication
Each room has a call bell system that’s monitored 24 hours a day, 7 days a week. If you need something, please use your call bell and say exactly what you need so we can send the right member of your transplant team to help you.
Diet
Your transplant team will plan your diet. You’ll be given a menu and instructions on how to order your meals. Room service will deliver your meals to you.
In general, everyone having a transplant is placed on a food safe diet. Your clinical dietitian nutritionist will discuss this with you. For more information, read the resource Eating Well After Your Stem Cell Transplant (www.mskcc.org/pe/eating_well_sct).
If you keep kosher, have diabetes, or follow other specialty diets, tell your clinical dietitian nutritionist so that we can prepare your meals properly. Your clinical dietitian nutritionist is also available to help you plan your meals.
Showering
You’ll be expected to shower daily. Your patient care technician will be in your room when you’re showering to help you and to make sure you’re safe.
Mouth Care
It’s important to take good care of your mouth. This will help to reduce infections and mouth sores. Your nurse will go over this with you.
The 5 Phases of Transplant
There are 5 phases of transplant. They are:
- Conditioning
- Transplant day to engraftment
- Engraftment to day of discharge
- Early convalescence
- Late convalescence
These phases are described in the table below. They’re also described in more detail in the following pages.
The phases and time frames aren’t exact, and there’s some usually some overlap from one phase to the next. Everyone’s transplant timeline is unique.
| Description | Time Period | |
|---|---|---|
| Phase 1 Conditioning |
|
|
| Phase 2 Transplant day to engraftment |
|
|
| Phase 3 Engraftment to day of discharge |
|
|
| Phase 4 Early convalescence |
|
|
| Phase 5 Late convalescence |
|
|
Phase 1: Conditioning
Conditioning is another name for the therapy given to get you ready for your transplant. Conditioning is usually a combination of 2 or more chemotherapy medications or chemotherapy and radiation therapy. The particular conditioning you’ll get is based on a number of factors and is discussed with you at your outpatient visits before admission.
Conditioning starts on a negative-numbered day (such as Day -7). Depending on your treatment plan, the number of days of conditioning will vary. Your stem cell transplant always takes place on Day 0. Every day after your transplant is referred to as a positive-numbered day (such as Day +1, Day +2).
| Day -10 to Day -1 | Day 0 | Day +1 |
|---|---|---|
| Conditioning (chemotherapy and possible radiation therapy) | Stem cell infusion (transplant) | Start of supportive care |
Before you get your chemotherapy, a number of safety checks will be done to make sure everything is correct. Once all the safety checks have been completed, your nurse will give you IV fluids (to keep you hydrated), antinausea medication, and the chemotherapy medication through your tunneled catheter (see Figure 4).

Radiation Therapy
The radiation therapy given before a transplant is usually total body irradiation (TBI). With TBI, small doses of radiation will be given to your whole body. If your transplant doctor recommends radiation as part of your conditioning, you’ll have a consultation appointment with a radiation oncologist before you’re admitted to the hospital. This doctor will explain the process and take some measurements of your body to be sure the radiation is given safely and effectively. They’re also responsible for prescribing the appropriate amount of radiation.
These doses are given 1 to 3 times a day and over 1 to 4 days. Each treatment will take 10 to 30 minutes. Having radiation therapy is like having an x-ray. The treatment doesn’t hurt.
You may also need a boost (additional radiation treatment) to other parts of your body. The treatment depends on the disease you have. Your transplant doctor and radiation oncologist will explain the details of your treatment plan.
If you’re male and have leukemia or lymphoma, you may have a boost to your testes. This is done to destroy cancer cells that may be hidden there.
Things to remember
- Don’t wear any jewelry during your treatments. The metal may change the radiation dose to that area.
- Stop using any creams, lotions, deodorants, or oils (even lip balm, such as ChapStick®) 2 days before you start radiation therapy. Don’t use them at all while you’re getting radiation. You can use Aquaphor®, but don’t apply it for 4 hours before your treatment.
- Family members can go with you when you have your treatments. They must wait outside the treatment room, but they can see you on a video screen and talk to you.
- You and your clothes won’t become radioactive during or after the treatments. You can’t pass the radiation to other people.
- Your nurse will tell you more about how the radiation is given and what you’ll do during the treatments.
Side Effects of Conditioning
Conditioning should kill some or all of the cancerous cells in your body. It will also get your bone marrow and immune system ready to get your transplant. But, the side effects of conditioning treatments aren’t to be taken lightly. They may include the loss of your ability to fight infections, infertility, hair loss, fatigue, nausea and vomiting, diarrhea, mouth sores, or mouth tenderness.
Your transplant team will help you and your caregiver understand and get ready for these side effects. Before you start treatment, make a list of questions you would like to ask about these side effects. Talk through these questions with your caregiver and transplant team.
Low white blood cell count (neutropenia)
Your treatment will damage your ability to fight infections and heal. It’s important to understand why this happens, how to watch for danger signs, and how to avoid infections and injuries.
One side effect of treatment is called neutropenia. Neutropenia is a condition in which you have a lower than normal number of neutrophils (a type of white blood cell) in your bloodstream. Neutrophils play a crucial role in your immune system—they’re one of the first types of cells that travel to the site of an infection. Once they reach the site of an infection, they ingest and fight potentially harmful germs.
Because your treatment will kill your stem cells, you’ll temporarily lose your ability to make new neutrophils. Since your neutrophils aren’t being replaced, the number of neutrophils in your bloodstream will drop to a very low level, leaving you at high risk of infection. Your transplant team will watch for any signs of infection. You may be given injections (shots) of a medication called filgrastim (Neupogen®). This medication stimulates the growth of neutrophils to help you recover faster.
Showering and bathing
While you’re neutropenic (have neutropenia), it’s very important to keep yourself clean.
Shower or bathe every day using a 4% chlorhexidine gluconate (CHG) solution antiseptic skin cleanser, such as Hibiclens®. 4% CHG solution is a fast-acting antiseptic that kills germs that live on your skin. It can work for up to 24 hours after you use it. Showering with it will lower your risk of infection.
To shower with 4% CHG solution:
- Use your normal shampoo to wash your hair. Rinse your head well.
- Use your normal soap to wash your face and genital area. Rinse your body well with arm water.
- Open the 4% CHG solution bottle. Pour some into your hand or a clean washcloth.
- Move away from the shower stream. Rub the 4% CHG solution gently over your body from your neck to your feet. Don’t put it on your face or genital area.
- Move back into the shower stream to rinse off the 4% CHG solution. Use warm water.
- Dry yourself off with a clean towel.
- Don’t put on any lotion, cream, deodorant, makeup, powder, or perfume.
When you use 4% CHG solution:
- Don’t use it on your head, face, eyes, ears, mouth, genital area, or on deep wounds. If you have a wound and aren’t sure if you should use 4% CHG solution on it, ask your doctor or nurse.
- Don’t use regular soap, lotion, cream, powder, or deodorant after washing with 4% CHG solution.
- If you have an irritation or allergic reaction when using 4% CHG solution, stop using it and call your doctor.
Caring for Your Mouth
While you’re neutropenic, you’ll need to change the way you brush your teeth and care for your mouth. This will help you avoid infection and bleeding. Follow these guidelines to take good care of your mouth:
- You’ll be given a mouthwash to rinse your mouth before meals, after meals, and at bedtime. The number of rinses may be increased to every 2 hours, depending on how your mouth feels. Only use the mouthwash that your nurse gives you. Most store-bought mouthwashes contain alcohol, which can irritate and dry your mouth and throat.
- Use an ultra soft toothbrush.
- You can use toothpaste that you buy in the store.
- Don’t use dental floss.
- Avoid licking your lips. Licking your lips makes them more chapped and dry.
- Apply a lip balm (such as Burt’s Bees®, ChapStick, or A&D® ointment) after you clean or rinse your mouth and every 2 to 4 hours as needed. This will help keep your lips moist.
- Your doctor may prescribe an oral antifungal antibiotic to keep you from getting an infection in your mouth. Use it as instructed.
- If your mouth becomes sensitive, avoid hot, spicy, acidic, or coarse foods. You may prefer soft or liquid food served cold or at room temperature.
- If you have a lot of pain from mouth sores, your healthcare provider will give you pain medication.
Anemia (low red blood cell count)
Your red blood cells carry oxygen from your lungs to the tissues in all parts of your body. When you’re anemic (have anemia), your blood can’t carry oxygen as well. Some of the side effects of anemia include:
- Fatigue (feeling more tired than usual)
- Weakness
- Fast heartbeat
- Shortness of breath
- Headache
- Pale skin
If you have anemia, your doctor may prescribe a blood transfusion.
Low platelet count (thrombocytopenia)
In addition to losing your ability to make neutrophils and other types of white blood cells, you’ll also lose your ability to make platelets. Platelets clump together to help stop bleeding. After your treatment, the number of platelets in your bloodstream will drop. This is called thrombocytopenia.
You’ll need to take special care to avoid cuts and strenuous activities that may cause bleeding. You also need to take special care of your gums and mouth because it’s common for bleeding to happen there.
You’ll need to take these special precautions if your platelets become very low:
- Avoid sharp objects, such as razors, scissors, and nail clippers. Only shave using an electric razor or shaver. Don’t use a razor that has a blade.
- Follow the guidelines in the “Caring for Your Mouth” section.
- If you’re straining to have bowel movements (poop), ask someone from your transplant team for a stool softener or laxative.
Tell your doctor if you have any signs of bleeding. Examples are:
- Easy bruising
- Faint, tiny, pin-point red dots on your torso, arms, or legs
- Vaginal spotting or heavy menstrual bleeding
- Broken blood vessels in the whites of your eyes
- Blood in your urine
- A headache that doesn’t get better, blurred vision, or dizziness
- Coughing up blood, vomiting blood, or a nosebleed that doesn’t stop after a few minutes with applied pressure or ice
- Black bowel movements (poop) or blood on your bowel movements
Nausea and vomiting
Nausea and vomiting are common side effects of treatment. Chemotherapy acts on a part of your brain that may trigger nausea and vomiting. Nausea and vomiting can also be caused by stress or just the thought of having chemotherapy. The amount of nausea and vomiting you have depends on the type of chemotherapy you get. You may have nausea during your conditioning, or it may be delayed for several hours or days.
You’ll be given medication to prevent and control nausea before your conditioning. These medications work differently for each person. If the medication you’re taking isn’t helping, tell your transplant team or doctor. You may need to try a different medication or take more than one kind of antinausea medication to feel better. Your transplant team will work with you to prevent and treat nausea and vomiting.
Diarrhea
Diarrhea is frequent, loose, watery bowel movements. It can also cause stomach cramps, gas, and pain in your abdomen (belly) or rectal area. Diarrhea can be caused by cancer treatments, medications, infection, stress, or other medical conditions. If you’re having diarrhea, you can become dehydrated due to loss of fluids and electrolytes.
Your nursing staff will keep track fluid losses that you may have from diarrhea. It’s important that you always use the collection container in the toilet to collect your bowel movements so they can be measured.
Constipation
Constipation is having hard, dry bowel movements or having fewer bowel movements than usual. It happens when materials move too slowly through your large intestine. The normal length of time between bowel movements is different for everyone. If you’re having fewer bowel movements than usual or if you haven’t had a bowel movement for more than 2 days, you may be constipated.
There are many causes of constipation, including not drinking enough liquids or not eating enough fiber, a decrease in your activity, not moving around or walking enough, and side effects of chemotherapy, antinausea medications, and pain medications.
Medications are available to treat constipation. Tell your nurse or medical team if you haven’t had a bowel movement for more than 2 days.
Mouth sores (mucositis)
Some treatments affect the cells that line your mouth and digestive tract. This is called mucositis. Mucositis can cause redness, swelling, tenderness, and sores on the lining of your mouth, tongue, and lips. You may have some mouth and throat discomfort that can make it hard to eat or swallow. Tell your nurse if you’re having any of these symptoms so they can be treated.
If you’re getting radiation therapy, you may also have discomfort in your salivary glands. Your salivary glands are found on both sides of your neck and under your chin. They may become tender and swollen and you may make less saliva. The swelling will decrease a few days after your conditioning. The decrease in saliva is usually temporary and gets better after several months.
Hair loss
The chemotherapy that kills cancer cells also kills the cells that make your hair. Most people lose their hair during their transplant.
Losing your hair can be an unpleasant and upsetting experience. Many people choose to cut their hair short before their transplant to take control of this process and to lessen the shock of losing their hair. Talk this through with your caregiver, friends, and family.
Before your transplant is also a good time to think about whether you would like to wear a wig. Modern wigs can look very natural and wearing one may make you feel more comfortable. A list of wig stores in New York is included in the resource Hair Loss and Your Cancer Treatment (www.mskcc.org/pe/hair_loss_cancer_treatment).
You can get a wig while you still have your hair or bring a clipping of your hair if you’d like your wig to match your natural hair color. Ask your doctor for a prescription for the wig, as some insurance companies will reimburse some of the cost of a wig.
Skin changes
Conditioning can cause skin changes such as increased dryness, flaking, discoloration, and darkening. When you bathe, use a body soap that’s labeled for “sensitive skin.” Discuss the use of products with your nurse. Use alcohol-free lotions, creams, or oils to help relieve the dryness.
Your skin may also be very sensitive to the sun and may burn very easily. Avoid bright sunlight. When you’re outside, wear a sunscreen with an SPF of at least 30 and protective clothing, such as long-sleeved shirts, long pants, and a hat. Skin is the most common site for cancer, and sun protection reduces the risk of skin cancers.
Your nurse will tell you how to manage skin reactions during your treatment. For more information, read the resource Skin Care Guidelines While You Are Receiving Radiation Therapy (www.mskcc.org/pe/skin_care_radiation_therapy).
Transplant Day
After you finish your conditioning regimen, you will get your stem cell infusion—your transplant.
On Day 0, your donor’s stem cells will be infused into your body. These stem cells will help you be able to make new blood cells and fight infections again.
You’ll be given medications about 30 minutes before your transplant to help reduce any side effects that you may have during the infusion. You’ll be closely monitored and your vital signs will be checked often during and after the infusion.
Your stem cell infusion
If the stem cells are from a donor that isn’t related to you, they’re brought to MSK right away. Here, they’re processed for an unmodified or T cell-depleted stem cell transplant.
Unmodified stem cell transplant
In an unmodified stem cell transplant, the T cells (type of white blood cell that plays an important role in your new immune system) aren’t removed from the stem cells before they’re given to you. They’re infused much like a blood transfusion over a few hours into your tunneled catheter. Red cells or plasma may need to be removed before you get the stem cells if you and your donor aren’t the same blood type.
T cell-depleted stem cell transplant
In a T cell-depleted stem cell transplant, the T cells are removed from the stem cells before they’re given to you. If you’re going to have a T cell-depleted stem cell transplant, you’ll get it after the T cells are removed in the laboratory. This takes 12 to 24 hours, so you’ll get it the day after your donor has given the stem cells. The stem cells will be injected directly into your tunneled catheter from a large syringe. There usually aren’t any side effects from the infusion of T cell-depleted stem cells.
Umbilical cord blood stem cell transplant
On the day of your transplant, the umbilical cord blood will be thawed in our laboratory and brought to your room in a bag. If you’re also getting partially matched T cell-depleted stem cells (haploidentical) from a family member, these will be given either on the same day as you get the cord blood, or on the following day.
The cord blood will be given to you through your tunneled catheter. Sometimes, people have nausea or get high blood pressure during an umbilical cord blood infusion. These issues will be treated as they happen.
Your doctor and nurse will discuss any questions or concerns you may have about the type of transplant you’re going to get.
Side effects
You may have some side effects during and after your infusion. This is more common if the stem cells are collected ahead of time and stored frozen. Side effects can include nausea, vomiting, a tickle in your throat, or a cough. Other side effects that can happen include low blood pressure, chills, and fever. It’s important that you communicate with your transplant team during your transplant. If you do have side effects, your transplant team will treat them.
If the stem cells you got were frozen and preserved, you may notice a strong, garlic-like taste in your mouth during and after your transplant. Your urine, sweat, and skin may also have a garlic-like smell. You may not notice the smell, but those around you’ll. This smell is caused by the preservative used to store the stem cells. It will gradually go away over 1 to 2 days. Your nurse will have lemons to use as a safe, natural air freshener during the infusion.
Additionally, if the stem cells you got were frozen and preserved, your urine may look discolored, ranging from pink-tinged to bloody. This can last for 24 hours after your transplant. This is your body’s way of getting rid of extra red blood cells that may be with the stem cells but aren’t needed.
Phase 2: Transplant Day to Engraftment
Once you’ve had your transplant, you’ll enter a period of watching and waiting for your donor stem cells to start making healthy new blood cells. This process is called engraftment. As engraftment happens, the number of white blood cells, red blood cells, and platelets in your blood will start to increase.
Some complications are possible after your transplant. Infection, bleeding, and anemia are some of the major complications that can happen while you’re waiting for your blood counts to return to normal. In most cases, there are steps that you and your transplant team can take to prevent, manage, and treat these complications.
Here’s a list of things that will happen during this phase:
- You will have testing. You’ll have blood tests and other tests as needed to monitor your progress. You’ll have blood drawn every day.
- You may continue to have side effects from the conditioning. You’ll be given medication to help manage the side effects and make you more comfortable.
- You will follow a food safe diet. Because you’re neutropenic, you’ll follow a diet that contains a low number of potentially harmful microbes.
- You may get transfusions. You may need to get a blood transfusion to boost the numbers of red blood cells and platelets in your bloodstream.
- Your blood counts will start to recover. Over time, as the stem cells engraft and start to make new blood cells, your blood counts will get higher.
- You will stay physically active. You’ll try to remain physically active after your transplant by limiting the amount of time you spend in bed and walking a little each day. Follow the recommendations that your physical therapist gives you.
Risk of Infection
You’ll be at risk for bacterial, fungal, and viral infections for several months after your transplant. They’re a major risk in the early recovery period until your new bone marrow grows and makes white blood cells to fight infection. You’ll still be at risk for some infections while your immune system recovers during the first 2 years after your transplant.
Fever is one important sign of infection. If you develop a fever, you’ll have a chest x-ray and urine and blood tests. You’ll be given IV antibiotics to help your body fight the infection. Nearly all people develop a fever during the first 2 weeks after their transplant. Most infections are treated successfully with antibiotics.
Your doctors and nurses will try to keep you from getting infections. You’ll likely be given medications that are used to treat infections. This can help prevent infections in people who have had a transplant. You’ll get antiviral medications to help keep some viral infections you may have had in the past (such as cold sores, shingles, or genital herpes) from coming back after your transplant. You’ll also get antifungal medication to prevent fungal infection.
People whose immune systems aren’t working well can get infections that wouldn’t happen in healthy people. These are called opportunistic infections. You may need medication to help protect you from these infections. You’ll be at risk for them until your white blood cell count and immune system return to normal.
Bleeding
Your platelet count will be low. Since platelets form blood clots, you’ll be at risk for bleeding. The mucous membranes of your nose, mouth, skin, and gastrointestinal (GI) tract are most commonly affected. You’ll have platelet transfusions if your count falls below 10,000 or if you have any bleeding.
Anemia
When your red blood cell count is low, you might have weakness and fatigue. Your nurse will help you with your daily activities if you need help. You’ll be given red blood cell transfusions as needed. These and all other blood products will be irradiated (exposed to radiation) to prevent harmful side effects.
Phase 3: Engraftment to Day of Discharge
Possible Early Complications
Time frames of transplant aren’t exact. Some of the side effects or complications reviewed here can happen in more than one phase of your transplant journey.
Organ complications
You may have complications in your kidneys, liver, lungs, or heart. Organ complications aren’t common, but they can be serious. You’re at higher risk if you already have a medical condition in any of these organs. This is why we carefully check your organ function before your transplant.
Kidneys
Your kidneys filter your blood and make urine to carry waste products out of your body. The chemotherapy and radiation therapy you get before your transplant can affect how well your kidneys work. This may be temporary, but it means that waste products may stay in your blood until your kidney function gets better. It also means that your kidneys will have more trouble getting rid of some of the medications you take.
Your nurses will keep track of the amount of fluids you get. This includes what you drink and what you get through your IV line. They’ll also write down how much urine you make. This will help your doctors to know if you’re starting to have problems with your kidneys. You’ll also have blood tests every day to tell your doctors how your kidneys are working. If needed, your doctors will adjust the doses of some of the medications you’re getting to decrease the risk of injuring your kidneys more.
Liver
In some people, small blood vessels in the liver are injured. This is called sinusoidal obstruction syndrome or veno-occlusive disease. If this happens, it can cause your liver to become enlarged and may damage your liver cells. Fluid may fill your abdomen. This usually starts within the first 3 weeks after a transplant. Everyone having a transplant gets a medication during their transplant process to help reduce the risk of developing sinusoidal obstruction syndrome or veno-occlusive disease.
If you have any side effects to your liver, your doctor will discuss the treatment options with you in more detail.
Lungs
Infections that affect the lungs (such as pneumonia) may cause breathing problems after a transplant. These problems most commonly develop in the first few weeks after a transplant and can be serious. Your transplant team will watch you closely for any sign of pneumonia. Tell them if you notice any change in your breathing. Don’t ignore a cough or shortness of breath. The treatment for pneumonia depends on what caused it.
To help prevent problems with your lungs, exercise them. This may help to keep them clear. Your nurse will show you how to do deep breathing exercises. You can also use an incentive spirometer, which is an instrument to help you practice deep breathing. Even getting out of bed and doing breathing exercises helps.
Heart
Your heart pumps blood throughout your body. Certain chemotherapy medications may have side effects that damage your heart. Your doctors will watch your heart function carefully while you’re in the hospital.
Graft versus host disease
Graft versus host disease (GVHD) happens when the donor’s immune cells (T cells) start to attack and damage your body’s organs. There’s a chance that GVHD will develop when the new stem cells start to engraft. A close match of HLA or tissue type between you and your donor helps lower this risk but doesn’t make it go away.
Risk factors for GVHD include your age and the gender of your donor. Anyone whose donor isn’t an identical twin gets some type of prevention for GVHD. This prevention includes either removing the T cells from the transplant (T cell depleted) or giving medications to prevent those T cells from causing GVHD. There are good and bad things about each method, and there are reasons that you would get one or the other. Your doctor will discuss these with you before your transplant.
There are two kinds of GVHD: acute GVHD and chronic GVHD.
Acute GVHD usually develops within the first 100 days after a transplant, but it can happen later. Symptoms of acute GVHD include:
- A skin rash that appears on parts of your body or your entire body
- Jaundice (yellow skin and eye color) and an enlarged liver
- Abnormal liver blood tests
- Loss of appetite
- Nausea and vomiting
- Mild to severe diarrhea
Chronic GVHD usually develops after 100 days but rarely before the first 3 months after transplant. It usually lasts longer than acute GVHD. Symptoms of chronic GVHD include:
- A dark skin rash or dry or thickened skin
- Loss of appetite
- Weight loss
- Diarrhea
- Dry mouth
- Tightness and discomfort in your mouth
- Dry eyes
- Hair loss
- Decreased energy
The symptoms of GVHD may be mild to severe. You may develop only acute GVHD, only chronic GVHD, or both acute and chronic GVHD. If you develop both, you may or may not have symptoms between the time that you develop acute and chronic GVHD.
GVHD may slow the growth of the bone marrow and recovery of the blood counts. This means it will take longer for your immune system to work properly. Because of this, you can be at an increased risk of infections. GVHD may affect one or more parts of your body.
If you have evidence of GVHD, your doctor will discuss the treatment plan with you.
Getting Ready for Discharge
Once your blood counts have recovered and any side effects or complications you had have resolved, your inpatient team will start working with you and your caregiver to get you ready for discharge. On average, people can be discharged about 3 weeks from their day of transplant. It may be a few days before that or it may be longer than 3 weeks, depending on your stem cell source and your exact treatment plan.
To be discharged from the hospital, you must:
- Have no fever
- Have blood counts that are in a safe range (neutrophil count higher than 1,000)
- Be eating and tolerating some solid food
- Be drinking 1½ to 2 liters of liquids a day
- Be tolerating your oral medications
- Have a caregiver to help you
Most of the time, your tunneled catheter will be removed right before you’re discharged.
Your transplant team will work with you before you’re discharged to make plans for your follow-up care. You’ll be seen in the outpatient clinic within 1 week of your discharge.
Medical alert jewelry
Before you leave the hospital, you will need to order a medical alert bracelet or necklace. Your transplant team will help you. Examples of medical alert jewelry companies include MedicAlert® (www.medicalert.org) and ROAD iD (www.roadid.com).
Your bracelet or necklace should be engraved with the statements “Allogeneic stem cell transplant” and “Irradiated cellular blood components and CMV-safe blood components only.” This will let paramedics or hospital staff know what to do if you’re in an accident and can’t tell them yourself.
Phase 4: Early Convalescence
This phase of your recovery extends over a long period of time—from discharge to 1 year after your transplant or longer. It’s important to remember that, even though your blood counts are coming back up to the normal range, your immune system is still very immature. You’ll still need to take medications and follow precautions to keep yourself healthy and avoid infection.
You may start to notice some complications, especially those that affect your organs. This can happen even if they weren’t a problem earlier in your course.
The time frames given here are general guidelines. Your transplant team may give you a more exact time frame.
Leaving the Hospital
Even though you may be very happy and feel ready to leave the hospital, you might also feel nervous. It’s normal to have some worries and concerns as you get closer to leaving the hospital. After you leave, you and your family will need to manage your care. Feeling confident and comfortable doing this takes time. During your follow-up visits, your social worker can help you get the services you need and give you emotional support.
When you leave the hospital, it will take time to get used to living at home again. You may find that the things you need to do to keep from getting sick add some stress to your life. Feeling a sense of balance and comfort again will come with time. Try to stay as calm and confident as you can.
Your recovery after transplant will be gradual. You probably won’t feel the way you did before your illness for a while. You may feel tired and weak, have a smaller appetite, and notice changes in the way things taste and smell. It will also take time for you to get your strength back and go back to doing the activities you enjoyed before your illness and transplant.
Preventing Infection
It usually takes 12 to 18 months for your immune system to recover from your transplant. We often tell people that the first year after transplant is like your first year of life as a newborn baby. During that time, you’re at risk for infection. Your transplant team will check your blood cell counts to see how well your immune system is working. This will help them advise you about any changes to the guidelines you must follow.
Be aware of the symptoms of infection listed below. Call your doctor’s office right away if you have:
- A fever of 100.4 °F (38.0 °C) or higher.
- Don’t take acetaminophen (Tylenol®) unless your healthcare provider tells you to.
- You don’t have to take your temperature every day. But, check it regularly if you don’t feel well.
- Flushed (red) skin, sweating, or shaking chills.
- Coughing, sneezing, runny nose, shortness of breath, or chest discomfort.
- Redness, swelling, or pain in your throat, eyes, ears, skin, joints, or abdomen.
- Blurred vision or other changes in your ability to see clearly.
- Nausea, vomiting, or diarrhea.
- Frequent urination, a burning feeling when you urinate, or both.
- Irritation in your rectum, including burning and pain.
- A rash.
- Small blisters (similar to cold sores) around your mouth or on any other part of your body.
- Trouble flushing your tunneled catheter, if you still have one.
You can catch viruses more easily until your immune system is back to normal. One of these is the virus that causes chickenpox and shingles. If you’re exposed to chickenpox or shingles, call your transplant doctor or nurse right away. You’ll need to be assessed.
Viruses that you’ve had in the past (such as chickenpox) can also reactivate. This often starts as pain in the skin with pimples or fluid-filled blisters. If you develop blisters, they can be tiny or as large as a pencil eraser. The blisters may be painful, itch, or burn. If you have any of these symptoms, call your doctor or nurse right away so you can be treated.
Once your immune system has recovered, you’ll start getting your childhood vaccines. This usually starts about 1 year after your transplant, but your transplant team will decide when the timing is right for you.
There are certain precautions you can take to decrease your chance of getting an infection. Below, we provide some guidelines for you to follow.
Personal hygiene
While you’re recovering from your transplant, it’s very important to keep yourself clean. Doing this can help prevent infection. Follow the guidelines below.
- Shower or bathe every day.
- Use a mild soap, such as Dove® or Caress®. Don’t use Ivory® or a deodorant soap. They can dry out your skin.
- Be sure to wash your underarms and groin.
- Use a washcloth and towel that are only for your personal use.
- If your skin is dry, avoid using very hot water. Apply baby oil or a skin moisturizer, such as Eucerin® or CeraVe®. Put it on after you bathe, while your skin is still damp. Gently pat your skin dry with your towel. Don’t use lotions containing alcohol. They’ll make your skin drier.
- Hair usually starts to grow back about 3 months after your transplant. It’s possible that your hair will grow back with a different texture. Although it’s rare, hair loss can happen months or years after your transplant.
- Limit your time in direct sunlight.
- Your skin will be more sensitive and may burn more easily after your transplant. The medications you’re taking may add to this. Whenever you’re in the sun, protect your skin with a sunscreen that has an SPF of at least 30. Reapply it often. If you’ll be in direct sunlight for 20 minutes or longer, cover your skin with cotton clothing and a protective hat.
- Being in the sun for too long may also reactivate cold sores (herpes simplex virus) or cause GVHD of the skin.
- You can wear contact lenses, but make sure they’re cleaned well before you put them in. Don’t reuse cleaning solution. Be sure to throw away cleaning solutions when they expire. If your eyes are dry, use moisturizing drops.
- You can wear makeup. Buy all new products after your transplant.
- New nails will grow and replace your old nails. This will happen gradually 3 to 4 months after your transplant. Don’t get a manicure or pedicure in a nail salon while your immune system is still recovering. You can give yourself a manicure or pedicure at home with your own equipment.
- If you still have a tunneled catheter, don’t let it soak in water while you bathe. Read the resource About Your Tunneled Catheter (www.mskcc.org/pe/about_tunneled_catheter) for more information.
- Don’t get body piercings or tattoos after your transplant. These increase your risk of hepatitis and other infections. Discuss any concerns you may have with your transplant doctor.
Mouth care
Keep following the instructions in the “Caring for Your Mouth” section until your transplant team tells you that can start using an ultra soft toothbrush. You can brush your teeth with an ultra soft toothbrush if:
- Your absolute neutrophil count (ANC) is higher than 500 (sometimes called 0.5).
- Your platelet count is 20,000 (sometimes called 20) or higher.
Ask your doctor or dentist when you can floss and brush your teeth with a regular toothbrush.
If you wear dentures, keep them clean to prevent an infection. Soak them every day in any type of denture cleaner. Use the directions on the product. Then, rinse them well with tap water. Your dentures may need refitting after your transplant.
If any of your medications are mouth rinses, take out your dentures before rinsing or swishing the medication. This will help the medications work better and will keep your mouth from becoming reinfected. Tell your doctor or nurse if you have pain or discomfort in your mouth.
You may have mouth dryness for 3 to 4 months or longer after your transplant. Don’t use store-bought, alcohol-based mouthwashes or hydrogen peroxide. They’ll dry and irritate your mouth. Instead, use a mild saltwater rinse. Make it by mixing ½ teaspoon of salt and ½ teaspoon of baking soda in an 8-ounce glass of water. Your dentist may prescribe other rinses. Sucking on sugarless candy or lozenges may also help.
Your salivary glands may not be as good at washing bacteria from your mouth after your transplant. This increases your risk of cavities. Use toothpaste with fluoride. You can also use a mouthwash with fluoride once your mouth has fully recovered and is no longer too dry. Follow the instructions on the mouthwash bottle.
Caring for your tunneled catheter
It’s just as important to keep your tunneled catheter clean after you go home as it was while you were in the hospital. If you go home with a tunneled catheter, your nurse will teach you how to care for it at home. You’ll have a chance to practice with your nurse watching. Read the resource About Your Tunneled Catheter (www.mskcc.org/pe/about_tunneled_catheter) for more information.
Your home environment
Keep your home as free of dirt and dust as possible. But, you shouldn’t go to extremes. Don’t repaint your walls or put down new carpets. In fact, you shouldn’t be around any renovations or construction until your transplant team tells you it’s okay. This includes those in process and those done within the past 3 months.
Stay out of musty areas where mold might grow, such as a damp basement. You can use an air filtration system in your home, but you don’t need to.
Don’t use a humidifier. Bacteria and mold grow easily in it. A pan of water placed near a heat source may help in the winter. Change the water every day.
In general, try not to do any chores like dusting or vacuuming for the first 3 months after your transplant. Depending on your energy level, it’s fine for you to cook, wash dishes, or iron. Keep your bathroom very clean, especially the tub and toilet. Use a disinfectant regularly. It’s best for someone else to do this.
Wash your eating utensils, towels, and linens carefully. They don’t need to be washed separately from the rest of your household.
- Thoroughly wash all forks, spoons, and knives with hot water and dishwashing detergent or use a dishwasher.
- Wash towels twice a week and bed linens once a week. Use only your own towels and washcloths, not those of your family members.
You can have plants in your home. But, for the first few months after your transplant:
- Don’t touch the soil from household plants unless you wear gloves and a mask.
- Don’t touch the water in a vase of flowers. Someone else should change the water in the vases daily.
Pets and animals
Animals can carry diseases. They may put you at greater risk for infection while your immune system is recovering. You can have a pet in your home and touch it, but it’s best that you don’t have close physical contact. For example, don’t hold the animal in your lap. Don’t touch the animal’s saliva or feces. Be sure to protect yourself from bites or scratches.
Don’t handle or care for birds, lizards, snakes, turtles, hamsters, or other rodents while you’re recovering. If you have an aquarium and you have to clean it yourself, protect yourself by wearing gloves.
If you have a cat or dog at home, follow the additional guidelines below until your doctor gives you other instructions.
- Be sure that your pet is up-to-date with immunizations and any booster shots.
- Have your pet’s veterinarian check their stool for parasites every year.
- If you have a cat, get it tested for feline leukemia and toxoplasmosis every year.
- Have your pet treated for fleas. If your pet walks through wooded areas, have it screened for ticks every day during tick season (May to November). Talk with your pet’s veterinarian about using a flea and tick collar.
- Don’t clean cat litter boxes or clean up after your dog. Have someone else do these things for you.
- Keep your pets indoors or on your own property whenever you can. This is to help keep them from getting diseases from other animals.
- Don’t let pets in your bed.
If you plan to get a pet after your transplant, it’s best that you choose a healthy dog or cat that’s more than 1 year old. Have it spayed or neutered. Outside of your home, avoid close contact with animals in a farm or a petting zoo.
Family and visitors
You can have close physical contact with people in your immediate family. But, don’t have close contact with someone who has a cold or any signs of being sick. Wear a mask if you must be in the same room with someone who’s sick. Your family members and close friends should get a yearly flu shot.
You can have visitors, but limit them to small groups. Don’t visit with anyone who has:
- A cold.
- Chickenpox or recently been exposed to chickenpox.
- Recently been exposed to herpes, shingles, or any other type of virus or infection.
- Recently got a vaccine with a live virus (such as varicella or rotavirus). There are very few of these, but if someone in your household needs one, their doctor should be told that you’re immune suppressed and live in the same household.
Call your doctor right away if you or a family member is exposed to chickenpox, shingles, measles, or German measles (rubella).
Outside your home
Take regular walks outside, but avoid dirty areas and construction sites. Walking is an excellent way to regain your strength and endurance. But, during the first few months after your transplant, avoid the following places when they’re crowded.
- Supermarkets
- Shopping malls
- Movie theaters
- Schools
- Restaurants
- Public transportation
- Places of worship (such as churches or synagogues)
You can go to these places at off-peak hours when there are fewer people.
Avoid taking public transportation (such as a train or bus) for at least 3 months after your transplant. We understand you may need to take a taxi, car service, or other transportation (such as Access-a-Ride) to return for follow-up visits. We recommended that you wear a mask when traveling by this means.
You can swim in the ocean after you regain your strength and are more active. Pay attention to alerts from the local health department. You can also swim in a private pool that isn’t crowded. Make sure the pool is chlorinated.
Don’t swim in lakes, rivers, or crowded pools until your immune system has recovered. Don’t swim if your tunneled catheter is still in place.
Bleeding
Platelets are blood cells that help form clots and control bleeding. When your platelet count is low, you’re at risk for bleeding. Many people are discharged with a low platelet count. It can take weeks or months for your body to make enough platelets so your count returns to normal. You may need to have platelet transfusions.
Signs of a low platelet count include skin changes, bleeding, or both. Skin changes may include a lot of bruising or petechiae (peh-TEE-kee-ee). These are tiny, purplish-red spots on the skin that don’t disappear when you press them. You may see them on your lower legs or inside ankles. If you see many petechiae, call your doctor. Other symptoms of a low-platelet count may include bleeding from your gums or nose.
If you leave the hospital with any of these symptoms and they increase in amount or frequency, call your doctor. If you haven’t had any of these symptoms and suddenly develop them, call your doctor. It may mean that there’s a change in your platelet count.
If you have an injury that causes bleeding, don’t panic. Stay calm and follow the guidelines below for the type of injury.
- Open wounds: If you cut yourself, put a clean, dry gauze pad, towel, or cloth over the cut. Press firmly. Keep pressing to apply pressure until the bleeding stops. If the bleeding doesn’t stop, elevate the wound. For example, raise your arm or prop up your feet. Apply ice to the wound and call your doctor.
- Nosebleeds: If you have a nosebleed, sit up and lean forward slightly. Don’t tilt your head back. Squeeze the bridge of your nose firmly between your thumb and forefinger for at least 10 minutes without letting go. If the bleeding doesn’t stop, keep squeezing your nose. Apply a small bag of ice to the bridge of your nose until the bleeding stops. If the bleeding continues longer than 30 minutes, call your doctor.
- Accidents: If you’re in an accident, you may need blood or blood products. They should be irradiated to 3,000 rads. This is to keep transfused blood from causing GVHD.
- Wear your medical alert jewelry at all times. It gives the doctor who will be treating you this information. Read the “Medical alert jewelry” section for information about what to write on your medical alert jewelry.
- If you’re admitted to another hospital, have the doctor call MSK right away for guidelines on blood products.
If your platelet count is below 50,000 (50), follow the guidelines below.
- Use an electric razor when shaving.
- Use a soft-bristle toothbrush or an oral irrigator (such as a WaterPic®) to prevent gum bleeding. Don’t use dental floss.
- Don’t take aspirin, products that have aspirin, or aspirin-like medications, such as such as ibuprofen (Advil®) or naproxen (Aleve®). For more information, read the section “Common Medications to Avoid.”
- Avoid blowing your nose forcefully.
- If you’re constipated, call your doctor. You may need more fiber in your diet or a stool softener.
- Avoid activities or sports that can cause injury. If you have any questions or concerns about this, talk with your doctor.
Resuming Your Activities
Daily activities
The time it takes to recover after a transplant varies. Most people find that it takes about 3 months, while others may need more or less time.
The time after your transplant is a time of cell recovery and growth. The cells in your mouth, stomach, intestine, hair, and muscles will all regrow. This requires calories and energy. You may feel more tired than you expected. Remember, this fatigue and weakness are normal. Each week, you should get more of your strength back.
Around the 3rd month after your transplant, your hair will start growing more quickly. You may feel well enough to start going back to your usual level of activity. From this point on, you’ll probably feel better and better. For most people, however, the first 2 to 3 months to 1 year after transplant remain a time of recovery.
Exercise
Most people find it takes time to regain their strength. It may be helpful to follow a regular exercise plan. When you start to exercise, start with easy exercises. Your physical therapist can help you decide what type of exercise is right for you. As you feel ready, ask your doctor how to increase your exercise.
Don’t play contact sports or ski until your platelet count is over 100,000.
Hobbies
Some hobbies, such as woodworking, painting, and model building, use products that can be toxic. Always work in a room with plenty of fresh air. Keep the windows open. Use nontoxic paints and glue. If you have questions or concerns about resuming any of your hobbies, ask your doctor.
Returning to school or work
The earliest you can go back to school or work is about 4 months from the time of your transplant. This time frame can vary from person to person and depends many things. Some people may feel ready to return right away, while others feel worried after being away for so long. It may help to start slowly. For example, start with a schedule of half days or 3 days a week. Most people tell us that thinking about returning is almost harder than actually doing it.
Making the transition back to your usual lifestyle can be hard. Some people have talked about feelings related to changes in their appearance, such as hair loss. Others have trouble concentrating or maintaining their attention span. Many can’t keep up their former pace. Your transplant team is here to talk with you about going back to school or work. You can talk to a social worker, nurse, psychiatrist, or your doctor. We can work with you to find ways to make your transition easier.
Traveling
For the first 100 days after the day of your transplant, avoid traveling more than about 1 hour away from MSK.
If you plan to travel by plane, talk with your transplant team. You must have a high enough platelet count to safely travel by plane.
If you plan to travel out of the country during the first 2 years after your transplant, talk with your transplant team. They may recommend that you see an expert in travel medicine to reduce your risk of infection while abroad, depending on your destination.
Sexual Health
Before you leave the hospital, ask your doctor about resuming sexual activity. It’s important for you and your partner to have answers to your questions. If new questions come up, you can discuss them during your follow-up visits.
Protecting yourself during sexual activity
Until your doctor tells you that your blood counts and immune system have recovered, follow these precautions:
- Avoid sex that involves penetration or contact with mucous membranes while your blood counts are low (a platelet count less than 50,000). This includes vaginal, oral, and anal sex or inserting fingers, vibrators, or other sex toys into your vagina or anus.
- Use latex condoms every time you have vaginal, oral, or anal sex.
- Use a barrier device (condoms or dental dams) any time your partner’s vaginal secretions or semen could enter your mouth.
- Avoid any sexual activity that could expose your mouth to feces.
- Avoid sex that involves contact with mucous membranes if you or your partner have a genital infection or think you might have one.
Hugging, cuddling, gentle touching, and kissing skin are other ways you can be intimate with your partner during this time.
For more information about being sexually active during and after treatment, read the resources below.
- Sex and Your Cancer Treatment (www.mskcc.org/pe/sex_cancer_treatment)
- Sexual Health and Intimacy (www.mskcc.org/pe/sexual_health_intimacy)
The American Cancer Society also publishes resources on sexuality after cancer treatment. They’re available for free from your local American Cancer Society (ACS) or on the ACS website at the links below.
- Sex and the Man With Cancer
www.cancer.org/treatment/treatments-and-side-effects/physical-side-effe… - Sex and the Woman With Cancer:
www.cancer.org/treatment/treatments-and-side-effects/physical-side-effe…
Information for women
After your transplant, you may have:
- Fewer menstrual periods
- No menstrual periods
- Vaginal dryness and discomfort
Talk with your BMT doctor before using the products below.
Vaginal moisturizers are nonhormonal, over-the-counter products that help relieve vaginal dryness and discomfort. They’re available in most drug stores or on the Internet. Examples are vitamin E liquid capsules, Replens®, Hyalo GYN®, and K-Y® Brand LIQUIBEADS™.
Vaginal lubricants usually come in a liquid or gel form. They’re used to supplement a woman’s own lubrication and minimize dryness and pain during sexual activity. You can use these lubricants to make sexual activities more comfortable and pleasurable. Examples are Astroglide®, K-Y® Jelly, and Pjur® Woman Bodyglide (a silicone-based lubricant). For more information, read the resource Improving Your Vulvovaginal Health (www.mskcc.org/pe/improving_vulvovaginal_health).
Depending on your treatment, the function of your ovaries may change. This can result in decreased estrogen levels. Your doctor may recommend that you take estrogen supplements after your transplant.
If you need any help or support with these issues, your doctor can refer you to a specialist in our Female Sexual Medicine and Women’s Health Program. You can also contact the program by calling 646-888-5076.
Information for men
Some men have decreased sexual desire after their transplant. This could have an impact on your relationship. However, as you regain your strength and increase your activities, this too will change.
Some men also have erectile dysfunction (ED) after their transplant. ED can be treated with medication, such as sildenafil citrate (Viagra®) or tadalafil (Cialis®). There are many other ways to treat ED. Your doctor can refer you to a specialist in our Male Sexual and Reproductive Medicine Program. You can also contact the program by calling 646-888-6024.
Drinking Alcohol and Using Tobacco
After your transplant, your organs need time to recover. Alcohol can harm your liver and recovering bone marrow. This harm can be worse if you’re taking medications that can affect your liver. Don’t drink alcohol until your doctor tells you it’s safe.
Never smoke:
- Cigarettes
- Cigars
- Marijuana
- Other tobacco products
Doing so can lead to a serious lung infection. It can also increase your risk of a second cancer. MSK has specialists who can help you quit smoking. For more information about our Tobacco Treatment Program, call 212-610-0507 or go to www.mskcc.org/cancer-care/counseling-support/tobacco-treatment.
Follow-up Care
Your follow-up visits will be scheduled before you’re discharged. In general, you’ll be seen at least 1 to 2 times a week for the first 3 months after your transplant. After that, your appointments will be spaced further apart as long as you’re doing well.
Before your visits, make a list of any medications that need to be refilled. If you’re going to run out of any medications before your follow-up visit, tell your doctor before your appointment. You’ll be given prescriptions during your visit to be filled either at MSK or your local pharmacy.
If you’re taking immunosuppressive medications, don’t take the morning dose on the days that you have a follow-up visit, unless your doctor gives you other instructions. Bring the dose to your appointment. During your appointment, you will have blood drawn to see how much of the drug is in your blood. Then, a staff member will tell you to take the medication.
When you come to the clinic for your follow-up visits, always wear a surgical mask. Bring a list of all the medications you’re taking and the dosages of each one. Some people find it helpful to bring a list of questions that have come up since the last visit.
You’ll have blood tests to check your blood counts, electrolyte levels, and liver and kidney function. Bone marrow aspirations will be done every few months. They’re usually done 1, 3, 6, 12, and 24 months after transplant. If needed, your bone marrow may be checked more often or for a longer time after your transplant. Bone marrow tests tell us about the health and growth of your marrow.
If you had a transplant for acute leukemia, you may need to have lumbar punctures (spinal taps). This is especially true for people who have had, or are at high risk for having, leukemia in their spinal fluid. A lumbar puncture lets your doctor give you more chemotherapy in your spinal fluid after your transplant. It can also be given through an Ommaya reservoir, if you have one.
You may need to have IV treatments such as antibiotics and blood transfusions. If you do, your doctor or nurse will tell you how long and how often you’ll need them. These appointments will usually be scheduled at the same time as your follow-up visits.
At some point after your transplant, you might be referred to our BMT Survivorship clinic. There, you’ll see a survivorship NP. A survivorship NP is part of your transplant team. They work closely with your doctors and nurses to help with your recovery. This NP will also communicate directly with your primary care provider so information about your transplant is included in your overall healthcare.
Dental care
After you have recovered from your transplant, go to your local dentist for routine checks. If you need extensive dental work, ask your transplant doctor what you should do. They’ll tell you when it’s safe to resume all dental care with your dentist.
Tell your doctor or dentist if you have:
- Taken the medications pamidronate (Aredia®) or zoledronic acid (Zometa®)
- Jaw tightness
- Toothaches
- Discoloration at your gum line
- Receding gums
Common Medications to Avoid
Don’t take aspirin, any medications containing aspirin, or nonsteroidal anti-inflammatory drugs (NSAIDs) until your doctor gives you other instructions. For a list of these medications, read the resource How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil (www.mskcc.org/pe/check-med-supplement).
Check the label of any over-the-counter medications that you’re thinking of taking to make sure they don’t contain ingredients you should avoid. If you aren’t sure if a medication is safe to take, ask your transplant team.
Don’t take any herbal supplements or home remedies without talking to your transplant team first.
Phase 5: Late Convalescence
Possible Long-Term Complications
In the section “Possible Early Complications,” we discussed issues that may come up with your kidneys, liver, heart, and lungs. Other organ systems, such as your endocrine system, may also be impacted.
Your endocrine system makes hormones. It may not return to normal after your transplant. You’ll have blood work and exams to check your hormone levels. Some people develop hypothyroidism (an underactive thyroid) after radiation therapy or just as a part of aging. If you develop it, you’ll need to take medication to supplement what your thyroid can’t make itself.
You’ll be followed in our survivorship clinic after your transplant and will be monitored closely for any late side effects you may have. Some of the testing you had as part of your pretransplant evaluation will be repeated, including an EKG, echocardiogram, and pulmonary function tests. We’ll monitor you for any thyroid dysfunction, evidence of a hormonal deficiency, and any sign of osteoporosis (bone loss).
Health issues such as thyroid dysfunction or bone loss can develop in any person, even if they haven’t had a transplant, but we want to monitor you closely and keep you well.
Other Possible (Uncommon) Complications
Graft failure or rejection
Transplanted stem cells sometimes don’t grow successfully inside the body. This is called graft failure. Graft rejection means that your immune system has rejected your new stem cells. You’ll get treatments before your transplant to prevent this from happening.
The risk of graft rejection lasts about 2 to 4 weeks after a transplant. Occasionally, graft failure can happen at a later time after a transplant. If this happens, one option may be to get more stem cells from your donor, if they’re available. This is called a “boost.” Your doctor will discuss treatment options with you if this happens.
Relapse
Many people are worried that their cancer will come back. Your risk is higher if you had your transplant when you were in an advanced stage of disease or you weren’t in remission. Your doctor will follow you closely to watch for any sign of relapse.
Continued Follow-up Care
Immunizations
After your transplant, you’ll lose the protection from the vaccines you got as a child. Everyone who has a stem cell transplant gets childhood vaccines once their immune system has recovered. This usually happens about 1 year after the transplant.
Once it’s safe for you to get vaccines, your transplant team will plan them. The vaccines can be given at MSK or your NP can give your primary care provider a list of the recommended vaccines. Please note that it’s sometimes hard for primary care providers to get the vaccines, so you may need to get them at MSK. You’ll get only “killed” vaccines first, and if you respond to those, you’ll then get “partially killed” vaccines, such as for measles and shingles.
Eye exams
You may develop cataracts if you got radiation therapy or high-dose steroids. See an eye doctor if you develop any of the following symptoms:
- Cloudy, blurry, foggy, or filmy vision
- Changes in the way you see color
- Problems driving at night, such as glare from oncoming headlights
- Problems with glare during the day
- Double vision
You might only need a change in your eyeglass or contact lens prescription. Be sure to tell your optician or eye doctor what treatment you had.
Try to wait until at least 3 months after your transplant before getting a new eyeglass or contact lens prescription. Your vision can change during the recovery process.
Educational Resources
This section contains the educational resources we referred to throughout this guide. You can find them online, or you can ask a member of your transplant team. You can also search for more educational materials on the Patient and Caregiver Education website, www.mskcc.org/pe.
- About Your Tunneled Catheter (www.mskcc.org/pe/about_tunneled_catheter)
- Allogeneic Donor Peripheral Blood Stem Cell Harvesting (www.mskcc.org/pe/allogeneic_pbsc_harvesting)
- About Bone Marrow Harvesting (www.mskcc.org/pe/bone_marrow_harvesting)
- Building Your Family After Cancer Treatment: For People Born With Testicles (www.mskcc.org/pe/building_family_born_testicles)
- Call! Don't Fall! (www.mskcc.org/pe/call_dont_fall)
- How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil (www.mskcc.org/pe/check-med-supplement)
- Communicating With Your Care Team: When to Call or Use MyMSK (www.mskcc.org/pe/communicating_using_mymsk)
- Fertility Preservation Before Cancer Treatment: Options for People Born with Ovaries and a Uterus (www.mskcc.org/pe/fertility_starting_treatment)
- About Your Blood Transfusion (www.mskcc.org/pe/blood_transfusion)
- Hair Loss and Your Cancer Treatment (www.mskcc.org/pe/hair_loss_cancer_treatment)
- Hand Hygiene and Preventing Infection (www.mskcc.org/pe/hand_hygiene)
- Improving Your Vulvovaginal Health (www.mskcc.org/pe/improving_vulvovaginal_health)
- Eating Well After Your Stem Cell Transplant (www.mskcc.org/pe/eating_well_sct)
- Sex and Your Cancer Treatment (www.mskcc.org/pe/sex_cancer_treatment)
- Sexual Health and Intimacy (www.mskcc.org/pe/sexual_health_intimacy)
- Skin Care Guidelines While You Are Receiving Radiation Therapy (www.mskcc.org/pe/skin_care_radiation_therapy)
- Sperm Banking (www.mskcc.org/pe/sperm_banking)