This information will help you get ready for your HDR brachytherapy (BRAY-kee-THAYR-uh-pee) with interstitial (IN-ter-STIH-shul) implants for treatment of gynecological cancers at MSK.
Read this resource at least once before your brachytherapy procedure. Use it as a reference in the days leading up to your treatment. Bring it with you every time you come to MSK, including for your treatments. You and your healthcare team will refer to it throughout your care.
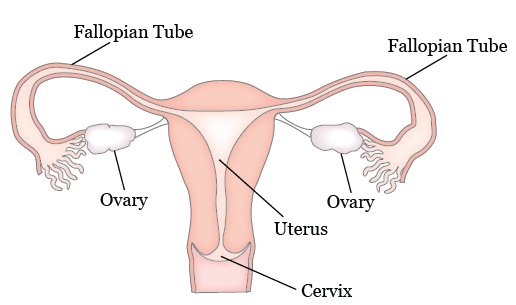
About your gynecological system
Your gynecological system includes your ovaries, fallopian tubes, uterus, cervix, and vagina. Your uterus is located in your lower abdomen (belly) between your bladder and rectum. The lower narrow end of the uterus is called the cervix (see Figure 1). Your ovaries and fallopian tubes are attached to your uterus.
About HDR brachytherapy
Brachytherapy is a type of radiation therapy. Radiation therapy kills cancer cells by making it hard for them to multiply. During brachytherapy, a radiation source is placed directly into or next to a tumor.
With HDR brachytherapy, your healthcare provider will place an applicator, also known as interstitial implantation device. The applicator will be placed in and around your vagina, cervix, or uterus. One end of the applicator will be implanted near the tumor during a surgery. The other end will be outside your body. There will be catheters (thin, flexible tubes) coming out of the applicator outside your body.
The radioactive source, which is Iridium-192, is stored in a separate unit. The outside end of the applicator will be connected to the radiation source through thin cables. Radiation will be guided through the applicator towards the tumor. After each treatment, the cables will be disconnected.
Most people get HDR after getting another type of radiation therapy called external beam radiation therapy. The HDR treatments begin about a week after the external beam radiation therapy is completed.
You’ll be admitted to the hospital for 2 days for your HDR treatment.
Your role on your radiation therapy team
You’ll have a team of healthcare providers working together to provide the right care for you. You’re part of the team, and your role includes:
- Arriving on time for your procedure.
- Asking questions and talking about your concerns.
- Telling someone on your radiation therapy team when you have side effects or pain.
- Caring for yourself at home.
- Quitting smoking, if you smoke. If you want to quit, call our Tobacco Treatment Program at 212-610-0507.
- Drinking liquids as instructed.
- Eating the foods suggested by your radiation therapy team.
- Maintaining your weight.
Getting ready for your procedure
You and your care team will work together to get ready for your procedure. Help us keep you safe by telling us if any of these things apply to you, even if you’re not sure.
I take an anticoagulant (blood thinner), such as:
These are examples of medicines. There are others.
Be sure your healthcare provider knows all the medicines you’re taking.- Aspirin
- Heparin
- Warfarin (Jantoven®, Coumadin®)
- Clopidogrel (Plavix®)
- Enoxaparin (Lovenox®)
- Dabigatran (Pradaxa®)
- Apixaban (Eliquis®)
- Rivaroxaban (Xarelto®)
- I take an SGLT2 inhibitor, such as:
- Canagliflozin (Invokana®)
- Dapagliflozin (Farxiga®)
- Empagliflozin (Jardiance®)
- Ertugliflozin (Steglatro®)
- I take prescription medicine(s), including patches and creams. A prescription medicine is one you can only get with a prescription from your healthcare provider.
- I take over-the-counter medicine(s), including patches and creams. An over-the-counter medicine is one you can buy without a prescription.
- I take dietary supplements, such as herbs, vitamins, minerals, or natural or home remedies.
- I have a pacemaker, automatic implantable cardioverter-defibrillator (AICD), or other heart device.
- I have sleep apnea.
- I have had a problem with anesthesia (A-nes-THEE-zhuh) in the past. Anesthesia is medicine to you sleep during a surgery or procedure.
- I’m allergic to certain medicines or materials, including latex.
- I’m not willing to receive a blood transfusion.
- I drink alcohol.
- I smoke or use an electronic smoking device, such as a vape pen or e-cigarette.
- I use recreational drugs, such as marijuana.
Presurgical testing (PST)
You’ll have a PST appointment before your procedure. You’ll get a reminder from your healthcare provider’s office with the appointment date, time, and location.
You can eat and take your usual medicine(s) the day of your PST appointment.
It’s helpful to bring these things to your appointment:
- A list of all the medicines you’re taking, including prescription and over-the-counter medicines, patches, and creams.
- Results of any medical tests done outside of MSK in the past year, if you have them. Examples include results from a cardiac stress test, echocardiogram, or carotid doppler study.
- The names and telephone numbers of your healthcare providers.
You’ll meet with an advance practice provider (APP) during your PST appointment. They work closely with MSK’s anesthesiology (A-nes-THEE-zee-AH-loh-jee) staff. These are doctors with special training in using anesthesia during a procedure.
Your APP will review your medical and surgical history with you. You may have tests to plan your care, such as:
- An electrocardiogram (EKG) to check your heart rhythm.
- A chest X-ray.
- Blood tests.
Your APP may recommend you see other healthcare providers. They’ll also talk with you about which medicine(s) to take the morning of your procedure.
About drinking alcohol
It’s important to talk with your healthcare providers about how much alcohol you drink. This will help us plan your care.
If you drink alcohol regularly, you may be at risk for problems during and after your procedure. These include bleeding, infections, heart problems, and a longer hospital stay.
If you drink alcohol regularly and stop suddenly, it can cause seizures, delirium, and death. If we know you’re at risk for these problems, we can prescribe medications to help prevent them.
Here are things you can do before your procedure to keep from having problems.
- Be honest with your healthcare providers about how much alcohol you drink.
- Try to stop drinking alcohol once your procedure is planned. Tell your healthcare provider right away if you:
- Get a headache.
- Feel nauseous (like you’re going to throw up).
- Feel more anxious (nervous or worried) than usual.
- Cannot sleep.
- Tell your healthcare provider if you cannot stop drinking.
- Ask your healthcare provider questions about drinking and procedures. All your medical information will be kept private, as always.
About smoking
If you smoke, you can have breathing problems when you have a procedure. Stopping for even a few days before your procedure can help.
Your healthcare provider will refer you to our Tobacco Treatment Program if you smoke. You can also reach the program by calling 212-610-0507.
About sleep apnea
Sleep apnea is a common breathing problem. If you have sleep apnea, you stop breathing for short lengths of time while you’re asleep. The most common type is obstructive sleep apnea (OSA). With OSA, your airway becomes fully blocked during sleep.
OSA can cause serious problems during and after a procedure. Tell us if you have or think you might have sleep apnea. If you use a breathing device, such as a CPAP machine, bring it on the day of your procedure.
7 days before your procedure
Follow your healthcare provider’s instructions for taking aspirin
Aspirin can cause bleeding. If you take aspirin or a medicine that has aspirin, you may need to change your dose or stop taking it 7 days before your procedure. Follow your healthcare provider’s instructions. Do not stop taking aspirin unless they tell you to.
To learn more, read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil (www.mskcc.org/pe/check-med-supplement).
Stop taking vitamin E, multivitamins, herbal remedies, and other dietary supplements
Vitamin E, multivitamins, herbal remedies, and other dietary supplements can cause bleeding. Stop taking them 7 days before your procedure. If your healthcare provider gives you other instructions, follow those instead.
To learn more, read Herbal Remedies and Cancer Treatment (www.mskcc.org/pe/herbal_remedies).
Ask about your diabetes medications, if needed
You’ll need to stop eating and drinking the night before and morning of your procedure. If you take insulin or another medication for diabetes, you may need to change the dose. Ask the healthcare provider who prescribes your diabetes medication what you should do the morning of your procedure.
2 days before your procedure
Stop taking nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs, such as ibuprofen (Advil® and Motrin®) and naproxen (Aleve®), can cause bleeding. Stop taking them 2 days before your procedure. If your healthcare provider gives you other instructions, follow those instead.
To learn more, read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil (www.mskcc.org/pe/check-med-supplement).
1 day before your procedure
Note the time of your procedure
A staff member will call you after the day before your procedure. If your procedure is scheduled for a Monday, they’ll call you on the Friday before. If you do not get a call by , call 212-639-5014.
The staff member will tell you what time to arrive for your procedure. They’ll also remind you where to go.
If you have any changes in your health or you need to cancel your procedure for any reason, call your radiation oncologist.
The night before your procedure
- Take the medications your healthcare provider told you to take the night before your procedure. Take them with a small sip of water.
- Shower using soap and water the night before or the morning of your procedure.
Instructions for eating and drinking: 8 hours before your arrival time
|
The day of your procedure
Instructions for drinking: 2 hours before your arrival time
| Stop drinking 2 hours before your arrival time. This includes water. |
Things to remember
- Take the medications your healthcare provider told you to take the morning of your procedure. Take them with a small sip of water.
- If you take any medication(s) for diabetes, remember that you might need to take a different dose than usual. Follow your healthcare provider’s instructions.
- Don’t put on any lotion, cream, deodorant, makeup, powder, perfume, or cologne.
- Don’t wear any metal objects. Remove all jewelry, including body piercings. The equipment used during your procedure can cause burns if it touches metal.
- Leave valuable items (such as credit cards, jewelry, and your checkbook) at home.
- If you wear contact lenses, wear your glasses instead. If you don’t have glasses, bring a case for your contacts.
What to bring
- A pair of loose-fitting pants, such as sweatpants.
- Reading material, electronic devices, cell phone, and charger. You’ll be lying in bed most of the time you’re in the hospital, so having ways to pass the time will be helpful.
- Your breathing device for sleep apnea (such as your CPAP device), if you have one.
Where to park
MSK’s parking garage is on East 66th Street between York and 1st avenues. If you have questions about prices, call 212-639-2338.
To get to the garage, turn onto East 66th Street from York Avenue. The garage is about a quarter of a block in from York Avenue. It’s on the right (north) side of the street. There’s a tunnel you can walk through that connects the garage to the hospital.
There are other parking garages on:
- East 69th Street between 1st and 2nd avenues.
- East 67th Street between York and 1st avenues.
- East 65th Street between 1st and 2nd avenues.
Once you’re in the hospital
When you get to the hospital, take the B elevator to the 6th floor. Check in at the desk in the Presurgical Center waiting room.
Many staff members will ask you to say and spell your name and birth date. This is for your safety. People with the same or a similar name may be having a procedure on the same day.
When it’s time to change for your procedure, you’ll get a hospital gown, robe, and nonskid socks to wear.
Meet with a nurse
You’ll meet with a nurse before your procedure. Tell them the dose of any medications you took after midnight (12 a.m.) and the time you took them. Make sure to include prescription and over-the-counter medications, patches, and creams.
Your nurse may place an intravenous (IV) line in one of your veins, usually in your arm or hand. If your nurse does not place the IV, your anesthesiologist will do it in the procedure room.
Meet with an anesthesiologist
You will also meet with an anesthesiologist (A-nes-THEE-zee-AH-loh-jist). An anesthesiologist is a doctor with special training in anesthesia. They will give you anesthesia during your procedure. They will also:
- Review your medical history with you.
- Ask if you’ve had any problems with anesthesia in the past. This includes nausea (feeling like you’re going to throw up) or pain.
- Talk with you about your comfort and safety during your procedure.
- Talk with you about the kind of anesthesia you’ll get.
- Answer questions you have about anesthesia.
During your procedure
When it’s time for your procedure, you’ll either walk into the operating room or be taken in on a stretcher. A member of the operating room team will help you onto the operating bed. Compression boots will be placed on your lower legs. These gently inflate and deflate to help blood flow in your legs.
Once you’re comfortable, your anesthesiologist will give you anesthesia through your IV line and you’ll fall asleep. You’ll also get fluids through your IV line during and after your procedure.
After you’re fully asleep, a breathing tube will be placed through your mouth and into your windpipe to help you breathe. A urinary (Foley) catheter will also be placed to drain urine (pee) from your bladder.
Your healthcare provider will place the applicator with small, needle-like catheters through your skin and into your vagina, cervix, or uterus. The exact location depends on where your HDR treatment will be delivered. Your healthcare provider will decide how many catheters are needed based on the size of the area being treated. The catheters will be held in place by a template (small piece of plastic with holes in it).
When all the catheters are inserted, you’ll have a magnetic resonance imaging (MRI) scan to make sure they’re in the right place. This scan will also help your healthcare provider finish the treatment planning process.
HDR brachytherapy treatment
After your treatment plan is confirmed, you’ll probably have your first treatment while you’re still in the operating room under anesthesia. For your treatment, tubes will be connected to the catheters in your body to deliver the radiation. The tubes are connected to a machine that stores the radioactive source. Once everything is ready, the radiation will be delivered through the tubes and catheters.
After the radiation is delivered, the tubes will be disconnected from the catheters and the treatment will end.
After your procedure
What to expect
When you wake up after your procedure, you’ll be in the Post-Anesthesia Care Unit (PACU). A nurse will be keeping track of your temperature, pulse, blood pressure, and oxygen levels. You’ll get oxygen through a tube resting below your nose. You’ll have a Foley catheter in your bladder to keep track of how much urine you’re making. You’ll also have compression boots on your lower legs to help your blood flow.
You may have some pain after your procedure. Your healthcare providers will ask you about your pain often. You’ll have a pain pump called a patient-controlled analgesia (PCA) device. PCA uses a computerized pump to deliver pain medication into your IV or epidural space (in your spine). For more information, read Patient-Controlled Analgesia (PCA) (www.mskcc.org/pe/pca). If your pain isn’t relieved, tell one of your healthcare providers.
There isn’t anything radioactive in your needles between your treatments. After your stay in the PACU, you’ll be taken to your hospital room.
While you’re in the hospital
While the catheters are in place, you’ll need to lie still on your back in bed. You must stay in bed until the catheters are removed.
While you’re in bed, you’ll be able to raise the head of your bed a little bit, about 20 degrees. You won’t be able to move your hips or legs, but you can wiggle your toes. You’ll have compression boots on your legs to help prevent blood clots and improve blood flow. You’ll be able to move your arms and upper body.
You’ll be asked to do deep breathing exercises using your incentive spirometer. This helps your lungs expand, which prevents pneumonia. For more information, read the resource How To Use Your Incentive Spirometer (www.mskcc.org/pe/incentive_spirometer).
You’ll follow a low-residue diet while you’re in the hospital. A low-residue diet has low amounts of fiber, which will help you have fewer bowel movements. You’ll also get medication to keep you from having a bowel movement. You may want to avoid eating foods that cause gas or make you feel bloated. You’ll eat all your meals in bed.
If you need any help, use your call bell to let a nurse know. The call bell is by the side of your bed.
We understand that lying still and flat in bed for several days can be challenging. You’ll be able to use your phone and other electronic devices, as well as read.
Getting additional HDR treatments
You’ll receive 4 to 5 HDR treatments while you’re in the hospital. For each of your treatments, your bed will be moved from your room to the treatment area in the Department of Radiation Oncology.
For your treatments, your radiation therapists will attach tubes to the catheters in your body. The tubes look like long plastic straws. One end is connected to a machine that stores the radioactive sources, and the other is attached to the catheters in your body.
Once everything is ready, your radiation therapist will leave the room while you receive the HDR treatment. The room has a video camera, microphone, and speaker so your radiation therapists can see, hear, and talk to you at all times.
During the HDR treatment, the radiation source will move through the tubes into the catheters. You won’t feel any pain or discomfort while the source is in place. You won’t see or feel the radiation. You may hear a clicking sound from the HDR machine.
Your treatment will take about 10 to 20 minutes.
After your treatment is done, the radiation source is moved back into the machine. Your radiation therapist will come back and disconnect the tubes from the catheters.
The rest of your treatments will be done the same way each time. You’ll have them twice a day. Each treatment is given about 4 to 6 hours apart.
After your last treatment
After your last treatment, you’ll get medication to make you relaxed and sleepy. The applicator, template, and catheters will be removed once the medication takes effect. You’ll then be brought back to your hospital room.
After the applicators, catheters, and template are removed, you may feel some cramping in your uterus and pressure in your vaginal area. These symptoms go away over a couple of hours. Ask your nurse for pain medication if you’re uncomfortable.
You may be discharged home that same day or early the next morning.
Dilator therapy
After HDR brachytherapy, your vagina may become dry, less elastic, narrower, and shorter. Together, these things are called vaginal stenosis. Before you go home, you’ll get instructions about how to use a vaginal dilator to help with these side effects.
Vaginal dilator therapy is a form of rehabilitation therapy you can use throughout your life. It will:
- Allow your healthcare provider to perform a more thorough pelvic exam.
- Make it more comfortable for you to be examined.
- Prevent your vagina from becoming too narrow.
- Keep your vagina more elastic.
- Allow you to have vaginal sex with less discomfort.
Your nurse will give you a vaginal dilator kit and explain how and when to use it. For more information, read the resource How to Use a Vaginal Dilator (www.mskcc.org/pe/vaginal_dilator).
At home
After your treatment is finished, you aren’t radioactive and don’t need to follow any radiation precautions.
You may have cramping for a day after your last treatment. Once at home, you can take ibuprofen (Advil® or Motrin®) or acetaminophen (Tylenol®) as needed. Don’t take Vitamin E, aspirin, or products that contain aspirin for at least 1 week after your procedure.
You can resume your regular diet.
You can shower after you’re discharged from the hospital.
You can begin driving once you’re home, as long as you’re not taking any prescription pain medications that make you sleepy.
For 6 weeks after your treatment:
- Don’t take a bath or swim in a pool.
- Don’t lift anything heavier than 10 pounds (4.5 kilograms).
- Don’t put anything inside your vagina (such as tampons and douches) or have vaginal intercourse.
Side effects
You may have side effects after your treatment. These side effects may last for 4 to 6 weeks.
If you need more help or support, contact the Female Sexual Medicine and Women’s Health Program at 646-888-5076.
Vaginal bleeding
You may have vaginal bleeding that looks like menstrual flow. This may last for up to 1 week.
Use sanitary pads for vaginal bleeding. Don’t use tampons.
Vaginal dryness
You may have vaginal dryness. This may last for the rest of your life.
Here is some information about vaginal moisturizers and when to start using them.
Hydrating moisturizers
- HYALO GYN®
- This moisturizer can be applied both inside of your vagina and on your vulva.
- You can buy HYALO GYN online at www.hyalogyn.com
- Replens™ Long-Lasting Vaginal Moisturizer
- This vaginal moisturizer can be inserted into your vagina with a disposable applicator or applied to your vulva.
- You can buy Replens Long-Lasting Vaginal Moisturizer at your local pharmacy.
Soothing (natural oil) types
- Carlson® Key–E® Suppositories
- These are suppositories (solid medications that dissolve) that you insert into your vagina with a disposable applicator. They work best if you use them at bedtime.
- You can buy Carlson Key-E suppositories online at www.carlsonlabs.com
- Natural oils, such as vitamin E or coconut oil
Vaginal or anal irritation
Your vaginal or anal area may become irritated. Avoid rubbing the area, because it can lead to more irritation.
Use a warm wet cloth to cleanse the area,
Since you won’t be able to take baths for 6 weeks, you can buy a plastic sitz bath at your pharmacy. It fits over your toilet and lets you take sitz baths.
You can also buy a peri-bottle, which is a small plastic bottle with a squirt tip. You can use to wash your vaginal or anal areas with warm water.
When to call your healthcare provider
Call your healthcare provider if you have:
- New or worsening chills.
- A fever of 100.4 °F (38 °C) or higher.
- Vaginal bleeding that’s more than light spotting.
- Cloudy or foul smelling urine.
- Blood in your urine.
- More than 3 watery bowel movements a day that aren’t helped by medication.
- No bowel movement in 3 days.
- Bleeding from your rectum.
- Nausea or vomiting and are not able to keep food or liquids down.
- Abdominal or pelvic pain that doesn’t go away after you take your pain medication.
- New or worsening redness around a wound.
- New or increased drainage from a wound.
- New or worsening shortness of breath or difficulty breathing.
- A heartbeat that is faster than usual.
- New or worsening cough.
- New or worsening pain.
- New or worsening leg pain, or cramping.
- New or worsening swelling in one or both legs, calves, ankles or feet.
Contact information
If you have questions or concerns, talk with a member of your radiation therapy team. You can reach them Monday through Friday from to
After , during the weekend, and on holidays, call 212-639-2000. Ask for the radiation oncologist on call.
If you have questions or concerns, talk with a member of your radiation therapy team. You can reach them Monday through Friday from to at these numbers.
Radiation oncologist: _____________________
Phone number: _________________________
Radiation nurse: ________________________
Phone number: _________________________
After , during the weekend, and on holidays, call 212-639-2000. Ask for the radiation oncologist on call.