This information will help you get ready for image-guided radiation therapy (IGRT). It will help you know what to expect before, during, and after your treatment. You will also learn about side effects and how to care for yourself during your treatment.
Read through this resource before you start radiation therapy. Use it as a reference in the days leading up to your treatments so that you can prepare as much as possible. Bring this resource to your simulation appointment and all future appointments with your radiation oncologist. You and your healthcare team will refer to it throughout your treatment.
About IGRT
Radiation therapy uses high-energy beams to treat cancer. It works by damaging the cancer cells and making it hard for them to reproduce. Your body is then naturally able to get rid of these damaged cancer cells. Radiation therapy also affects normal cells. However, your normal cells are able to repair themselves in a way that cancer cells can’t.
IGRT can treat tumors with even more accuracy than traditional radiation therapy. IGRT involves taking many images of the tumor during treatment. This ensures that we’re aiming the beam of radiation to the correct area. You won’t see or feel the radiation.
You may have IGRT if:
- Your radiation therapy will be given in 1 to 5 treatments instead of multiple treatments.
- Your treatment needs to be very precise, for safety reasons.
- You need treatment in a part of your body where there’s movement. It may be:
- A tumor in your lung or liver that moves when you breathe.
- A tumor in your abdomen (belly) or pelvis that moves due to fullness or movement of your digestive tract.
- A tumor in your spine or surrounding areas.
Radiation therapy takes time to work. It takes days or weeks of treatment before cancer cells start to die. They will keep dying for weeks or months after radiation therapy ends.
Your role on your radiation therapy team
Your radiation therapy care team will work together to care for you. You’re a part of that team, and your role includes:
- Getting to your appointments on time.
- Asking questions and talking about your concerns.
- Telling us when you have side effects.
- Telling us if you’re in pain.
- Caring for yourself at home by:
- Quitting smoking if you smoke. MSK has specialists who can help. To learn more about our Tobacco Treatment Program, call 212-610-0507. You can also ask your nurse about the program.
- Caring for your skin based on our instructions.
- Drinking liquids based on our instructions.
- Eating or avoiding the foods and drinks we suggest.
- Staying around the same weight.
Simulation
Before you begin your radiation therapy, you will have a treatment planning procedure called a simulation.
The simulation is done to make sure that:
- Your treatment site is mapped out.
- You get the correct dose of radiation.
- The radiation dose to nearby tissues is as small as possible.
During your simulation, you will have x-rays done and your skin may be marked with little tattoo dots. These marks help your team make sure you’re in the right position for your radiation therapy.
Your simulation will take 2 to 4 hours but can be longer depending on the treatment your doctor has planned for you.
Getting ready for your simulation
- During your simulation, you will be lying in one position for a long time. If you think you will be uncomfortable lying still, you can take acetaminophen (Tylenol®) or your usual pain medication before your simulation.
- If you think you may get anxious during your procedure, ask your doctor if medication may be helpful.
- Wear comfortable clothes that are easy to take off because you may need to change into a hospital gown. Don’t wear jewelry, powders, or lotions.
You may need to have other procedures before your simulation to help with treatment planning. If you need to have one of the procedures below, we will schedule them for you.
Some people will need to have other procedures done before the simulation to help in treatment planning. If you need to have any of the procedures below, we will schedule them for you.
- Placement of markers: Several gold markers will be implanted into the area to be treated. These markers are the size of a grain of rice and can be seen on x-rays and a computed tomography (CT) scan. Marker placement will be done a number of days before your simulation. You will be told where to go to have it done. Someone from Interventional Radiology will contact you the day before to give you instructions and to confirm the time of your arrival.
- Myelogram: A contrast dye will be injected into your spinal canal. This helps us see your spinal cord and surrounding tissues more clearly. This is done several hours before your simulation.
- A staff member from Radiology will call you the day before your procedure. He or she will tell you what time you should arrive at the hospital for your procedure. If your procedure is scheduled on a Monday, you will be called on the Friday before. If you don’t receive a call by the business day before your procedure, please call 212-639-7298.
- You will need to go to the Center for Image-Guided Interventions (CIGI) at 1275 York Avenue between East 67th and East 68th Streets. Take the M elevators to the 2nd floor.
- Your myelogram will be done before your simulation. After you have recovered, you will be brought back to the Department of Radiation Oncology on a stretcher for your simulation.
Take devices off your skin
You may wear certain devices on your skin. Before your simulation or treatment, some device makers recommend you take off your:
- Continuous glucose monitor (CGM)
- Insulin pump
If you use one of these, ask your radiation oncologist if you need to take it off. If you do, make sure to bring an extra device to put on after your simulation or treatment.
You may not be sure how to manage your glucose while your device is off. If so, before your appointment, talk with the healthcare provider who manages your diabetes care.
Day of your simulation
What to expect
A member of your radiation therapy team will check you in. You will be asked to state and spell your full name and date of birth many times. This is for your safety and part of our standard identification process. People with the same or similar names may be having care on the same day as you.
You will be greeted by your radiation therapist. He or she will take a photograph of your face. This picture will be used to identify you throughout your treatment.
Your radiation therapist will then explain the simulation to you. If you have not already signed a consent form, your radiation oncologist will review everything with you, and ask for your signature.
During your simulation
For your simulation, you may need to get undressed and change into a gown. You should keep your shoes on. If you wear a head covering, such as a wig, turban, or cap, you may have to remove it. Your radiation therapists will help you lie down on a table and make every effort to ensure your comfort and privacy.
Although the table will have a sheet on it, it is hard and has no cushion. If you have not taken pain medication and think you may need it, tell your radiation therapists before your simulation begins. Also, the room is usually cool. If you feel uncomfortable at any time, let your radiation therapists know.
Throughout your simulation, you will feel the table move into different positions. The lights in the room will be turned on and off and you will see red laser lights on each wall. Your radiation therapists use these laser lights as a guide when they position you on the table. Do not look directly into the red beam because it may damage your eyes.
Although your radiation therapists will walk in and out of the room during your simulation, there will always be someone who can see and hear you. You will hear your radiation therapists speaking to each other as they work, and they will explain to you what they are doing. Do not move once your simulation begins because it may change your position. However, if you are uncomfortable or need assistance, tell your radiation therapists.
To help pass the time, your radiation therapists can play music for you. You may bring a CD of your own from home, if you wish.
Positioning and molds
Depending on the area of your body that is area being treated, frames, molds, or masks may be made. These will help you stay in the correct position and will be used with each treatment. It takes about 30 minutes to make these.
Upper spine: You will lie on your back within a frame, with your hands holding the handles at your sides (see Figure 1). The frame lines up your shoulders and hips to keep you in proper alignment. A mask will be made for you that will extend to your shoulders.
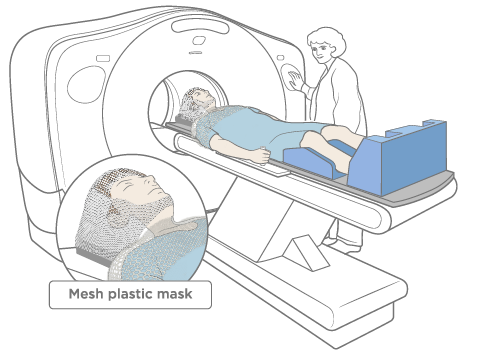
Figure 1. Upper spine mold Lower spine: You will lie on your back with a paddle on both sides of your hips (see Figure 2).
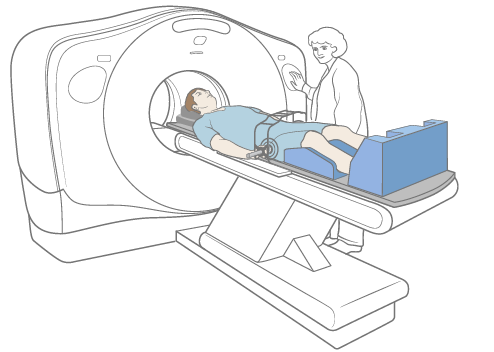
Figure 2. Lower spine mold Abdominal compression: You will lie on your back. You will be asked to put on a harness-like jacket (see Figure 3). The lower portion will lie across your lower abdomen (belly) and air will be slowly added into it, creating pressure. This is to reduce the movement of your liver while we are taking x-ray images.
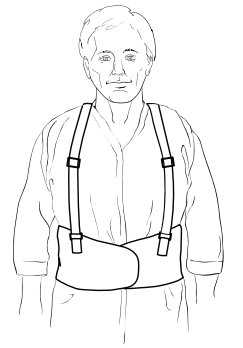
Figure 3. Abdominal compression - Face mask: Your radiation therapist will place a warm, wet sheet of plastic mesh over your face and will shape it to fit around your head. You will be able to hear and breathe without difficulty while the mask is on. As the mask cools, it will harden.
Body mold: You will probably be lying on your back throughout your simulation. A mold may be made of your upper body to help you maintain the same position each time you receive your treatment. Your therapists will pour a warm fluid into a large plastic bag that will be sealed and placed on the table. You will lie on top of the bag, on your back, with your arms raised above your head (see Figure 4). The fluid will feel warm at first, but it will cool as it hardens. While it is cooling, your radiation therapist will tape the bag to your skin so that it will take the shape of your upper body and arms. This procedure takes about 15 minutes. During your simulation, and each day of your treatment, you will lie in this mold to help ensure you are in the correct position.
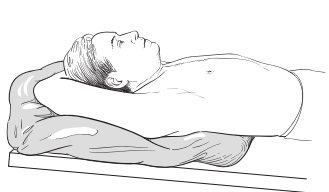
Figure 4. A body mold
X-ray images
While you are lying in your position, you will get x-rays of the area to be treated. These may be done on an x-ray machine called a simulator or on a computed tomography (CT) scan machine. These scans are used only to map your treatment. They are not used for diagnosis or to find tumors. If you need other imaging, your nurse will explain this to you.
It will take about 45 minutes to get your x-rays. During the scan, you will hear the machine turn on and off. Even if the noise seems loud, your radiation therapists will be able to hear you if you speak with them.
Skin markings (tattoos)
Your radiation therapists will draw on your skin in the area being treated with a felt marker. You may need permanent skin markings called tattoos. Your radiation therapists will use a sterile needle and a drop of ink to make the tattoo. The sensation of getting one feels like a pinprick. The tattoo marks are no bigger than the head of a pin. The felt marking can be washed off after your simulation. The tattoos are permanent and will not wash off. If you’re concerned about receiving tattoos as part of your radiation treatment, talk with your doctor.
After the tattoos are made, your therapists will take several photographs of you in your simulation position. The photographs and tattoo marks will be used to position you correctly on the table each day of your treatment.
Additional imaging
We may need to use other imaging tests along with the CT scan to help us plan your treatment. These are done the same day as your simulation, right after the procedure. We will schedule these for you and bring you to the area where they will be done. If you think you will feel anxious during these procedures, ask your doctor about medication that may help you relax.
- Magnetic resonance imaging (MRI): This procedure will be done in the Department of Radiation Oncology while you are in the body mold we made during your simulation. It helps us see your spine more clearly.
- Positron emission tomography (PET) scan: This procedure will be done while you are in the body mold we made during your simulation. It helps us see the difference between normal and abnormal tissues. This will be done in either the Department of Radiation Oncology or the Molecular Imaging and Therapy Service (MITS). The MITS is sometimes called the Nuclear Medicine service.
After your simulation
At the end of your simulation, you may be given an appointment card with the date and time for your first treatment. If your appointment cannot be made then, we will call you to tell you the date and time.
Scheduling your treatment
IGRT may be given in several different schedules. Your schedule is based on what your radiation oncologist recommends. It can be:
- A single treatment, usually given on the same day as your setup or beam films.
- Three to 5 treatments, usually given every other day
- Daily treatment, given Monday through Friday, for about _____ weeks.
You must come in every day that you are scheduled for your treatment. Your treatment may not be as effective if you skip or miss appointments. If you need additional time due to unforeseen circumstances, your radiation oncologist will tell you. If you for some reason you can’t come in for treatment, you must call your radiation oncologist’s office to let your team know. If you need to change your schedule for any reason, speak with your radiation therapist.
Planning your treatment
During the time between your simulation and first treatment, your radiation oncologist will work with a team to plan your treatment. They will use your simulation x-rays, CT scan, and any other imaging tests that were done to plan the angles and shapes of your radiation beams. They will also determine the dose of radiation that your body will receive. These details are carefully planned and checked. This process takes about 7 business days.
Vitamins and dietary supplements during radiation therapy
It’s OK to take a multivitamin during your radiation therapy. Do not take more than the recommended daily allowance (RDA) of any vitamin or mineral.
Do not take any other dietary supplements without talking with a member of your care team. Vitamins, minerals, and herbal or botanical (plant-based) supplements are examples of dietary supplements.
Set-up procedure
Before your first treatment, you will be scheduled for a set-up procedure. This generally takes about 1 hour. If pain medication was helpful during simulation, you may want to take it before this procedure.
When you come for your set-up procedure, you will be shown to the dressing room and asked to change into a gown. Your therapists will bring you to the room where you will receive your treatment each day. They will position you on the treatment table. You will lie exactly as you were lying day of your simulation.
Special x-rays called beam films will be taken to make sure that your position and the area being treated are correct. The beam films will be repeated throughout your treatment. They are not used to see how your tumor responds to the treatment.
Depending on your treatment plan, you may start treatment on the same day as your set-up procedure.
During your treatment
After you check in at the reception desk, have a seat in the waiting room. When your radiation therapists are ready for you, they will tell you to change into a gown. If you are taking any pain medication, you should take it at this time.
Your radiation therapists will bring you into the treatment room and help you lie in your mold on the table (see Figures 5 and 6). You will be positioned exactly how you were lying during your set-up procedure.
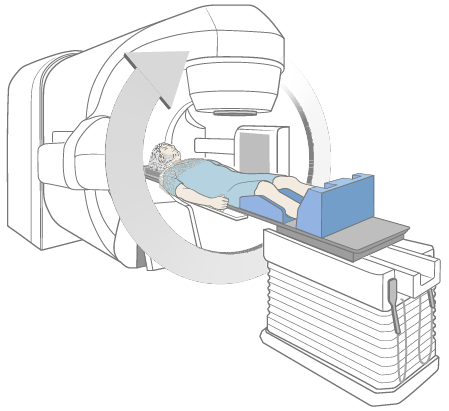
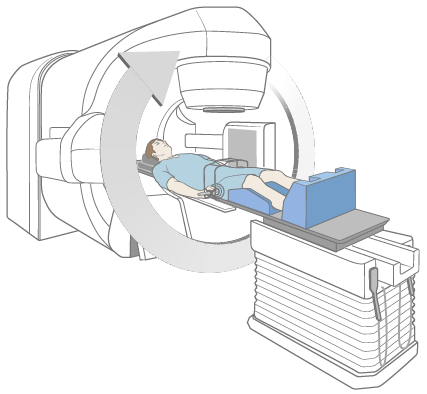
Once you are positioned correctly, your radiation therapists will leave the room, close the door, and start your treatment. You will not see or feel the radiation, but you may hear the machine as it moves around you and is turned on and off. You will be in the treatment room for about 2 hours, depending on your treatment plan. Most of this time will be spent putting you into the correct position. If you are getting more than 1 treatment, the next one may last 30 minutes to 2 hours, depending on your treatment plan.
Although you will be alone during the treatment, your radiation therapists will see you on a monitor and hear you through an intercom at all times. They will make sure that you are comfortable during the treatment. Breathe normally during the treatment, but do not move. However, if you are uncomfortable or need help, speak to your radiation therapists. They can turn off the machine and come in to see you at any time, if necessary.
Neither you nor your clothes will become radioactive during or after treatment. It is safe for you to be around other people.
Weekly visits during your treatment
Your radiation oncologist and nurse will see you each week to evaluate your response to treatment. This visit will be before or after your treatments each _______________. You should plan on being in the department about 1 extra hour on those days.
During these visits, you should ask questions and discuss any concerns you have. If you need to speak with your radiation oncologist or nurse anytime in between these weekly visits, ask the support staff or therapists to contact them when you come in for treatment.
If you are receiving 1 or 3 treatments, your radiation oncologist and nurse will see you at least once during your treatment.
Side effects
Some people develop side effects from radiation therapy. The type and how severe they are depend on many factors. These include the dose of radiation, the number of treatments, and your overall health. Side effects may be worse if you are also getting chemotherapy. Below are the most common side effects of radiation therapy. You may have all, some, or none of these. Depending on the area being treated, there may be other side effects that your doctor and nurse will discuss with you.
Many patients ask about vitamins. You may take a daily multivitamin if you wish. Do not take more than the recommended daily amount of any vitamin. Do not take any supplements unless your radiation oncologist approves them. This includes both nutritional and herbal supplements.
Swelling around the treatment area
IGRT may cause swelling around the area that is being treated. You may need to take a steroid called dexamethasone (Decadron®) to prevent it. Whether you need it depends on the area we are treating and the amount of radiation you will be getting. If you need the steroid, you will be told how to take it before and after your treatment. Be sure to take it exactly as you are told.
If you develop any symptoms after your treatment, such as increased pain or difficulty moving, call your doctor or nurse immediately. The dose may need to be adjusted or you may need additional medication.
Skin and hair reactions
During radiation therapy, your skin and hair in the area being treated may change. This is normal. After 2 to 3 weeks, your skin may become pink or tanned. It may even become bright red or very dark later on.
Your skin may feel dry and itchy, and may look flaky during treatment. Sometimes, the skin in sensitive areas may blister, open, and peel. If this happens, tell your doctor or nurse.
You may also notice a rash, especially in any area where you have had previous sun exposure. Although this may be a side effect of treatment, a rash could also be a sign of infection. If you develop a rash at any time during your treatment, tell your doctor or nurse.
Your nurse may apply special dressings or creams and teach you how to care for your skin. Your doctor may stop your treatment until your skin heals. This skin reaction sometimes becomes more severe during the week after treatment is done. If this happens, call your doctor or nurse. Your skin will gradually heal after your treatment is completed, but this often takes 3 to 4 weeks.
You may lose some or all of the hair in the area being treated. Your hair will usually grow back 3 to 6 months after your treatment is completed.
Below are guidelines to help you care for your skin during treatment. Follow these guidelines until your skin gets better. These guidelines refer only to the skin in the area being treated with radiation.
Keep your skin clean
- Bathe or shower daily using warm water and a mild unscented soap, such as Neutrogena®, Dove®, baby soap, Basis®, or Cetaphil®. Rinse your skin well and pat it dry with a soft towel.
- When washing, be gentle with your skin in the area being treated. Do not use a washcloth, a scrubbing cloth, or brush.
- If you received tattoo marks before your treatment, they are permanent and won’t wash off. You may get other markings during treatment such as an outline of your treatment area with a purple felt-tipped marker. You can remove these markings with mineral oil when your therapists say it’s okay.
- Do not use alcohol or alcohol pads on your skin in the area being treated.
Moisturize your skin often
- Start using a moisturizer when you begin treatment. This can help to minimize any skin reaction. You can use over-the-counter moisturizers. When choosing a moisturizer pick one that does not have any fragrances or lanolin. There are a number of products that are good to use, and your nurse may suggest one of these to you. Use only one at a time unless your nurse tells you to use more.
- If you are using a moisturizer, apply it 2 times a day.
Avoid irritating your skin in the area being treated
- Wear loose-fitting cotton clothing in the area being treated. Do not wear tight clothing that will rub against your skin.
- Use only the moisturizers, creams, or lotions that are recommended by your doctor or nurse.
- Don’t use makeup, perfumes, powders, or aftershave in the area being treated.
- Don’t use deodorant if your skin is open, cracked, or irritated. You can use deodorant on intact skin in the area being treated. Stop using it if your skin becomes irritated.
- If your skin is itchy, do not scratch it. Apply moisturizer. Ask your nurse for recommendations on how to relieve the itching.
- Don’t shave in the area that is being treated. If you must shave, use only an electric razor. Stop if your skin becomes irritated.
- Don’t put tape on your treated skin.
- Don’t let your treated skin come into contact with extreme hot or cold temperatures. This includes hot tubs, water bottles, heating pads, and ice packs.
- If you have no skin reactions during your treatment, you can swim in a chlorinated pool. However, be sure to rinse off the chlorine right after getting out of the pool.
- Avoid tanning or burning your skin during treatment and for the rest of your life. If you are going to be in the sun, use a PABA-free sunblock with an SPF of 30 or higher. Also, wear loose-fitting clothing that covers you as much as possible.
Fatigue
Fatigue is feeling tired or weak, not wanting to do things, not being able to concentrate, or feeling slowed down. You may develop fatigue after 2 to 3 weeks of treatment, and it can range from mild to severe. Fatigue may last 6 weeks to 12 months after your treatment ends.
There are a lot of reasons why you may develop fatigue during treatment, including:
- The effects of radiation on your body.
- Traveling to and from treatment.
- Not having enough restful sleep at night.
- Not eating enough protein and calories.
- Having pain or other symptoms.
- Feeling anxious or depressed.
- Certain medications.
You may find that your fatigue is worse at certain times of the day. Below are suggestions to help you manage your fatigue.
Ways to manage fatigue
- If you are working and are feeling well, continue to do so. However, working less may help increase your energy.
- Plan your daily activities. Pick those things that are necessary and most important to you and do them when you have the most energy. For example, you may go to work but not do housework, or watch your children’s sports event but not go out to dinner.
- Plan time to rest or take short naps (10 to 15 minutes) during the day, especially when you feel more tired. If you do nap, try to sleep for less than 1 hour at a time.
- Try to sleep at least 8 hours every night. This may be more sleep than you needed before you started radiation therapy. You may also find it helpful to go to sleep earlier at night and get up later in the morning. One way to sleep better at night is to be active during the day. For example, if you are able to exercise, you could go for a walk, do yoga, or ride a bike. Another way to sleep better at night is to relax before going to bed. You might read a book, work on a jigsaw puzzle, listen to music, or do calming hobbies.
- Ask family and friends to help you with things like shopping, cooking, and cleaning. Check with your insurance company to see if they cover home care services.
- Some people have more energy when they exercise. Ask your doctor if you can do light exercise, such as walking, stretching, or yoga.
- Eat foods that are high in protein and calories. Ask your nurse for the resource Eating Well During Your Cancer Treatment (www.mskcc.org/pe/eating-cancer-treatment).
- Other symptoms, such as pain, nausea, diarrhea, difficulty sleeping, or feeling depressed or anxious, can increase your fatigue. Ask your doctor or nurse for help with any other symptoms you may have.
Other side effects
Some people may experience other side effects. Your radiation oncologist or nurse will discuss these with you.
Sexual health
You might have concerns about how cancer and your treatment can affect your sexuality. You aren’t radioactive. You can’t pass radiation to anyone else, so it’s safe to be in close contact with other people.
You can be sexually active during radiation treatment, unless your radiation oncologist gives you other instructions. However, if you or your partner are able to have children, you must use birth control (contraception) to prevent pregnancy during your treatment.
The American Cancer Society has resources about sexual health issues during cancer treatment. The one for men is called Sex and the Man with Cancer. The one for women is called Sex and the Woman with Cancer. You can search for them at www.cancer.org or call 800-227-2345 for a copy.
MSK also has sexual health programs to help you address the impact of your disease and treatment on your sexual health. You can meet with a specialist before, during, or after your treatment.
- Female Sexual Medicine & Women’s Health Program: For more information or to make an appointment, call 646-888-5076.
- Male Sexual & Reproductive Medicine Program: For more information or to make an appointment, call 646-888-6024.
Emotional health
|
|
|
You might also worry about telling your employer you have cancer or about paying your medical bills. You may worry about how your family relationships may change, or that the cancer will come back. You may worry about how cancer treatment will affect your body, or if you will still be sexually attractive.
It’s normal and OK to worry about all these things. All these kinds of feelings are normal when you or someone you love has a serious illness. We’re here to support you.
Ways to cope with your feelings
Talk with others. When people try to protect each other by hiding their feelings, they can feel very alone. Talking can help the people around you know what you’re thinking. It might help to talk about your feelings with someone you trust. For example, you can talk with your spouse or partner, close friend, or family member. You can also talk with a chaplain (spiritual advisor), nurse, social worker, or psychologist.
Join a support group. Meeting other people with cancer will give you a chance to talk about your feelings and learn from others. You can learn how other people cope with their cancer and treatment and be reminded you’re not alone.
We know that all cancer diagnoses and people with cancer are not the same. We offer support groups for people who share similar diagnoses or identities. For example, you can join a support group for people with breast cancer or for LGBTQ+ people with cancer. Visit www.msk.org/vp to learn about MSK’s support groups. You can also talk with your radiation oncologist, nurse, or social worker.
Try relaxation and meditation. These kinds of activities can help you feel relaxed and calm. You might try thinking of yourself in a favorite place. While you do, breathe slowly. Pay attention to each breath or listen to soothing music or sounds. For some people, praying is another way of meditation. Visit www.msk.org/meditations to find guided meditations lead by our Integrative Medicine and Wellness providers.
Exercise. Many people find that light movement, such as walking, biking, yoga, or water aerobics, helps them feel better. Talk with your healthcare provider about types of exercise you can do.
We all have our own way of dealing with tough situations. Often, we do what worked for us in the past. But sometimes that’s not enough. We encourage you to talk with your doctor, nurse, or social worker about your concerns.
After your treatment
Please be sure to keep your follow-up appointments with your radiation oncologist. He or she will evaluate your response to treatment. You may have blood tests, x-rays, and scans during these visits. Before coming, write down your questions and concerns. Bring this and a list of all your medications with you. You can also call your doctor or nurse at any time after your treatment is completed, or in between follow-up visits, if you have any questions or concerns.
Contact information
If you have questions or concerns, contact a member of your radiation therapy team. You can reach them Monday through Friday from to at these numbers.
Radiation oncologist: _____________________
Phone number: _________________________
Radiation nurse: ________________________
Phone number: _________________________
Outside those hours, you can leave a message or talk with another MSK provider. There is always a doctor or nurse on call. If you’re not sure how to reach your healthcare provider, call 212-639-2000.
Resources
MSK support services
Counseling Center
www.msk.org/counseling
646-888-0200
Many people find that counseling helps them. Our counseling center offers counseling for individuals, couples, families, and groups. We can also prescribe medications to help if you feel anxious or depressed. To make an appointment, ask your healthcare provider for a referral or call the number above.
Female Sexual Medicine & Women’s Health Program
646-888-5076
Cancer and cancer treatments can affect your sexual health, fertility, or both. Our Female Sexual Medicine & Women’s Health Program can help with sexual health problems, such as premature menopause or fertility issues. We can help before, during, or after your treatment. Call for more information or to make an appointment.
Integrative Medicine Service
www.msk.org/integrativemedicine
Our Integrative Medicine Service offers many services to complement (go along with) traditional medical care, including music therapy, mind/body therapies, dance and movement therapy, yoga, and touch therapy. To schedule an appointment for these services, call 646-449-1010.
You can also schedule a consultation with a healthcare provider in the Integrative Medicine Service. They will work with you to come up with a plan for creating a healthy lifestyle and managing side effects. To make an appointment, call 646-608-8550.
Male Sexual and Reproductive Medicine Program
646-888-6024
Cancer and cancer treatments can affect your sexual health, fertility, or both. Our Male Sexual and Reproductive Medicine Program can help with sexual health problems, such as erectile dysfunction (ED). We can help before, during, or after your treatment. Call for more information or to make an appointment.
Nutrition Services
www.msk.org/nutrition
212-639-7312
Our Nutrition Service offers nutritional counseling with one of our clinical dietitian-nutritionists. Your clinical dietitian-nutritionist will talk with you about your eating habits. They can also give advice on what to eat during and after treatment. To make an appointment, ask a member of your care team for a referral or call the number above.
Resources for Life After Cancer (RLAC) Program
646-888-8106
At MSK, care does not end after your treatment. The RLAC Program is for patients and their families who have finished treatment.
This program has many services. We offer seminars, workshops, support groups, and counseling on life after treatment. We can also help with insurance and employment issues.
Tobacco Treatment Program
www.msk.org/tobacco
212-610-0507
MSK has specialists who can help you quit smoking. For more information about our Tobacco Treatment Program, call 212-610-0507. You can also ask your nurse about the program.
External resources
American Cancer Society (ACS)
www.cancer.org
800-ACS-2345 (800-227-2345)
Offers a variety of information and services, including Hope Lodge, a free place for patients and caregivers to stay during cancer treatment.
American Society for Therapeutic Radiology and Oncology
www.rtanswers.org
800-962-7876
A group of radiation oncology professionals that specializes in treating patients with radiation therapy. Provides detailed information on treating cancer with radiation and contact information for radiation oncologists in your area.
CancerCare
www.cancercare.org
800-813-HOPE (800-813-4673)
275 7th Ave. (between West 25th & 26th streets)
New York, NY 10001
Provides counseling, support groups, educational workshops, publications, and financial assistance.
Cancer Support Community
www.cancersupportcommunity.org
Provides support and education to people affected by cancer.
National Cancer Institute (NCI) Cancer Information Service
www.cancer.gov
800-4-CANCER (800-422-6237)
Provides education and support to people with cancer and their families. Publications are available online and in print.
Questions to ask your radiation oncologist
Before your appointment, it’s helpful to write down questions you want to ask. Examples are listed below. Write down the answers during your appointment so you can review them later.
What kind of radiation therapy will I get?
How many radiation treatments will I get?
What side effects should I expect during my radiation therapy?
Will these side effects go away after I finish my radiation therapy?
What kind of late side effects should I expect after my radiation therapy?