This information explains what intraperitoneal (IP) chemotherapy is and how to get ready for it.
What is intraperitoneal chemotherapy?
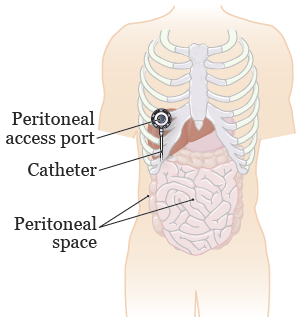
Your peritoneal (payr-ih-toh-NEE-ul) space is the area between the muscles and organs in your abdomen (belly) (see Figure 1). There is a little fluid between the peritoneal lining and your organs. If your cancer spreads to your abdomen or peritoneal space, IP chemotherapy can help target the cancer cells there.
During IP chemotherapy, the medicine will just target the cancer in your peritoneal space. This treatment uses a higher dose of chemotherapy medication to do this. Your healthcare provider will teach you about the medicine that will be used for your IP chemotherapy.
You may get your IP chemotherapy as an inpatient or an outpatient. Inpatient is when you stay in the hospital. Outpatient is when you don’t stay in the hospital but come in for treatments.
Depending on the type of cancer you have and the medication you need, your healthcare provider will let you know:
- Where you will get your IP chemotherapy.
- How many treatments you will have.
- How long your therapy will last.
Some people may need to switch between having intravenous (through a vein) therapy and IP chemotherapy given at different times.
How is intraperitoneal chemotherapy given?
During your IP chemotherapy, you will lie down in a bed. You can get up to go to the bathroom. You may get fluids or medication intravenously (IV, through a vein).
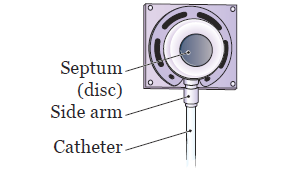
Your healthcare provider will put a needle through your skin and into the self-sealing disc on your access port. This will feel like a small pinprick. They will tape the needle in place and cover it with a small bandage.
The access port will have a catheter (thin, flexible tube) connected to it. The catheter will be placed into your peritoneal space (see Figure 1). Your IP chemotherapy medication will be mixed with fluids, such as normal saline. The fluid and medication mixture will be in a bag that’s attached to the needle. It will be injected directly into your peritoneal space through your access port.
This mixture will flow into your peritoneal space. You may need to have more fluid placed into your IV after your treatment. This is to make sure the medication fills your entire peritoneal space.
What is an access port and why do I need it?
Before you start IP chemotherapy, your healthcare provider will place an access port under your skin near your rib cage. This will be done during a procedure before your treatment starts. The access port lets your care team put medication into your bloodstream.
The port has a raised chamber. On top of the chamber is a self-sealing rubber septum (disc). The chamber also has a side arm to attach the catheter to (see Figure 2). You may see or feel the port under your skin. This is normal.
How do I get ready for intraperitoneal chemotherapy?
- Eat a light dinner the night before and a light breakfast on the morning of your treatment. You may get nauseous during your treatment if your stomach is full.
- Dress comfortably the morning of your treatment. Wear loose-fitting shirts and pants with an elastic band or a draw string. You may feel bloated after treatment so you will feel more comfortable if you can loosen your pants.
- If you want to, you can bring a music player so you can listen to music during treatment. There will be a TV in the room where you will get your treatment. Someone can also stay with you during your treatment.
- You can bring food and drinks with you into the treatment room. Most people do not have an appetite during treatment, but you can eat during your treatment if you’d like to.
Arrange for someone to take you home
You must have a responsible care partner take you home after your procedure. A responsible care partner is someone who can help you get home safely. They should be able to contact your care team if they have any concerns. Make sure to plan this before the day of your procedure.
If you don’t have a responsible care partner to take you home, call one of the agencies below. They’ll send someone to go home with you. There’s a charge for this service, and you’ll need to provide transportation. It’s OK to use a taxi or car service, but you still need a responsible care partner with you.
| Agencies in New York | Agencies in New Jersey |
| VNS Health: 888-735-8913 | Caring People: 877-227-4649 |
| Caring People: 877-227-4649 |
What can I expect after my intraperitoneal chemotherapy treatment session?
After the fluid flows fully into your peritoneal space, your healthcare provider will take out the needle. They will put a bandage on the area. This bandage can be taken off about 30 minutes after your treatment session ends.
If you’re inpatient and cannot get out of bed, we will ask you to move from side to side in bed. You must do this every 15 minutes for 1 hour (4 times total). This will help the solution move throughout your peritoneal space. Then your IP chemotherapy will be over, and you can get out of bed. Your body will absorb the solution over the next few days.
If you’re an outpatient, make sure you move around for the next hour after your treatment is over. Try to walk around if you can. This lets the medication reach all parts of your peritoneal space. You should also rest, drink fluids, and eat small meals after your treatment.
The time the treatment takes can be different for everyone. It’s usually no more than 1.5 to 2 hours. Some treatments may last as long as 6 hours if you need extra IV fluid. Ask your healthcare provider how long your treatment may take.
What are the side effects of intraperitoneal chemotherapy?
The side effects of IP chemotherapy are different for everyone. This section lists the most common side effects and how you can manage them. The side effects can be caused by the amount of fluid that’s injected into your peritoneal space. They can be caused by the medication itself. You may have none, some, or all of these side effects.
Abdominal pressure or bloating
- After your treatment is over, try to walk around. This will help with the pressure or bloating. Wear comfortable clothes, such as pants with an elastic band, for your treatments. Wear these clothes for a few days after your treatments.
Full bladder or the need to urinate (pee) often
- Try to empty your bladder just before you start your treatments. You can also use the bathroom during your treatments.
Faster breathing
- Raise your head on a pillow during your treatment. When your treatment is over, you can walk around or sit upright in a chair.
Nausea (feeling like you might throw up) and vomiting (throwing up)
- Your healthcare provider may give you medication to help with nausea before or during your IP chemotherapy. They may also prescribe this medication for you to take at home if you need it.
Loss of appetite (not feeling hungry)
- Try to eat smaller meals more often. For example, try eating 6 half-size meals instead of 3 main meals each day. This will allow you to eat the same amount of food overall, but in smaller portions that will be easier to digest (break down).
- Drink liquid nutritional supplements such as Ensure®.
- Keep snacks around to eat when you’re feeling hungry.
How can I care for my access port at home?
Since the access port is under your skin, you do not need to cover or bandage it. You can bathe and shower as you usually do. You can follow your normal diet.
Having a port and catheter should not limit your activities. Ask your healthcare provider about going back to your normal activities.
Check the skin around your port every day. Call your healthcare provider if there are any problems or changes.
When to call your healthcare provider
Call your healthcare provider if you have any of the following:
- Severe or constant stomach pain.
- A fever of 100.4° F (38° C) or higher.
- Redness, swelling, or tenderness in the area around your port site.
- Leaking or drainage from your port site.
- Nausea or vomiting that lasts more than 24 hours (1 day).
- Diarrhea (loose, watery bowel movements) that lasts more than 24 hours.
- Constipation (not able to have a bowel movement) that lasts more than 24 hours.
- If you cannot eat or drink for more than 24 hours.
- Any unexpected or unexplained problems.