This information will help you get ready for radiation therapy to your lymph nodes at MSK. It explains what to expect. It also explains how to care for yourself before, during, and after your radiation therapy.
This information is general. Your radiation therapy team will design a treatment and care plan just for you. Because of that, some parts of your treatment may be different than what’s described here. Your radiation therapy team will talk with you about what to expect.
About radiation therapy
Radiation therapy uses high-energy radiation to treat cancer. It works by damaging the cancer cells, making it hard for them to multiply. Your body can then naturally get rid of the damaged cancer cells. Radiation therapy also affects normal cells, but they can fix themselves in a way cancer cells can’t.
Radiation therapy takes time to work. It takes days or weeks of treatment before cancer cells start to die. They keep dying for weeks or months after radiation therapy ends.
You might have radiation therapy on its own. Or, you might have it before, during, or after chemotherapy (chemo) or surgery. Your radiation therapy care team will talk with you about what to expect.
About external beam radiation therapy
You’ll have a type of radiation therapy called external beam radiation therapy. During your treatments, a machine will aim beams of radiation directly at the tumor. The beams will pass through your body and destroy cancer cells in their path. You will not see or feel the radiation.
About radiation therapy to your lymph nodes
Many people have radiation therapy to their lymph nodes as part of their treatment for lymphoma.
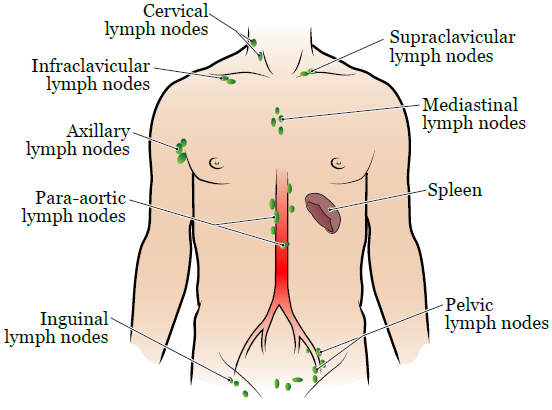
There are many groups of lymph nodes in your body (see Figure 1). You’ll get radiation therapy just to the group or groups with cancer cells.
Some people also get radiation therapy to their spleen. Your spleen is an organ in your abdomen (belly).
Your radiation oncologist or nurse will check off the areas that will be targeted during your radiation therapy.
Your radiation oncologist or nurse will tell you which of the following areas will be targeted during your radiation therapy.
- The lymph nodes in your neck (cervical lymph nodes).
- The lymph nodes above your collar bone (supraclavicular lymph nodes).
- The lymph nodes below your collar bone (infraclavicular lymph nodes).
- The lymph nodes in the middle of your chest (mediastinal lymph nodes).
- The lymph nodes in your armpit (axillary lymph nodes).
- The lymph nodes in your abdomen (para-aortic lymph nodes).
- Your spleen.
- The lymph nodes in your pelvis (pelvic lymph nodes).
- The lymph nodes in your groin (inguinal lymph nodes).
Your role on your radiation therapy team
Your radiation therapy care team will work together to care for you. You’re a part of that team, and your role includes:
- Getting to your appointments on time.
- Asking questions and talking about your concerns.
- Telling us when you have side effects.
- Telling us if you’re in pain.
- Caring for yourself at home by:
- Quitting smoking if you smoke. MSK has specialists who can help. To learn more about our Tobacco Treatment Program, call 212-610-0507. You can also ask your nurse about the program.
- Caring for your skin based on our instructions.
- Drinking liquids based on our instructions.
- Eating or avoiding the foods and drinks we suggest.
- Staying around the same weight.
What happens before radiation therapy to your lymph nodes
Simulation appointment
You’ll have a treatment planning procedure called a simulation before your first radiation treatment. During your simulation, your radiation therapists will take imaging scans. They may also mark your skin with little tattoo dots. The imaging scans and tattoos help to:
- Map your treatment site.
- Make sure you get the right dose (amount) of radiation.
- Limit the amount of radiation that gets to your nearby healthy tissues.
Your simulation appointment will take about 2 hours. It may be shorter or longer based on your treatment plan.
Positron emission tomography-computed tomography (PET-CT) scan
Some people have a PET-CT scan during their simulation. If you are, your nurse will give you detailed instructions for getting ready for the scan.
Sometimes, PET-CT scans use intravenous (IV) contrast. IV contrast is a dye that’s put into your bloodstream to make the images clearer. Some people are allergic to IV contrast. If you are, tell your nurse. They will tell you what to do.
If you’re having a PET-CT scan, do not eat or drink anything except water for 6 hours before your appointment time. This includes gum, hard candy, cough drops, and mints. If you have anything except water, we may need to reschedule your PET-CT scan.
Medicines to take
You’ll be lying still in one position for a long time during your simulation. If you think you’ll be uncomfortable, take an over-the-counter pain medicine or your usual pain medicine 1 hour before your simulation.
If you think you may get anxious during your simulation, talk with your healthcare provider ahead of time. They may suggest medicines to help.
What to eat and drink
Your healthcare provider will tell you if you need to follow special instructions for eating or drinking before your simulation. If you don’t need to follow special instructions, you can eat and drink like usual.
What to wear
Wear comfortable clothes that are easy to take off. You will need to change into a hospital gown. Do not wear jewelry, powder, lotion, or cream, unless a member of your care team says it’s OK.
Take devices off your skin
You may wear certain devices on your skin. Before your simulation or treatment, some device makers recommend you take off your:
- Continuous glucose monitor (CGM)
- Insulin pump
If you use one of these, ask your radiation oncologist if you need to take it off. If you do, make sure to bring an extra device to put on after your simulation or treatment.
You may not be sure how to manage your glucose while your device is off. If so, before your appointment, talk with the healthcare provider who manages your diabetes care.
What to bring
If your dentist made a mouth guard for you, bring it to your simulation.
Leave any valuable items you don’t need at home. Examples include extra credit cards, extra cash, and jewelry.
What to expect when you arrive
A member of your radiation therapy team will check you in when you arrive. They’ll give you an identification (ID) wristband with your name and date of birth. During your appointment, many staff members will check your ID wristband and ask you to say and spell your name and date of birth. This is for your safety. People with the same or a similar name may be getting care on the same day.
Your radiation therapists will review what to expect during the simulation. If you haven’t already signed a consent form, they will go over the form with you. They will answer any questions you have and ask for your signature.
You’ll change into a hospital gown when it’s time for your simulation. Keep your shoes on. If you wear a head covering (such as a wig, turban, or cap), you may need to take it off.
What to expect during your simulation
Your radiation therapists will help you onto the simulation table. The table will have a sheet on it, but it’s hard and does not have a cushion. If you have not taken pain medicine and think you may need it, tell your radiation therapists before your simulation starts.
Your radiation therapists will help you get into position for your simulation. Your position will depend on which group or groups of lymph nodes are being treated.
Your simulation will take about 2 hours but can be shorter or longer depending on your specific treatment plan. Your radiation therapists can play music for you to help pass the time.
Do not move once your simulation starts. It’s important that you stay in the same position. Tell your radiation therapists if you feel uncomfortable or need help.
Imaging scans and positioning
Your radiation therapists will use computed tomography (CT) scans or PET-CT scans to check and adjust your position throughout your simulation. These scans are only to plan your treatments. They are not for diagnosis or to find tumors.
- If you’re having a PET-CT scan, your nurse may place an IV line in one of your veins. You’ll get contrast through the IV line before the scan. The contrast helps your care team get clear images of the treatment area.
- If you’re having a CT scan, you may need to hold your breath during the scan. Your radiation therapists will tell you how and when to hold your breath.
You’ll feel the simulation table move into and out of the scanner and hear the scanner turn on and off. You will see red or green laser lights on the walls. Your radiation therapists use the lasers to help position you on the table.
Even if it seems loud, your radiation therapists will be able to hear you if you need to speak with them. They will walk in and out of the room during the scans, but the room has a microphone, speaker, and camera. Someone will always be able to see and hear you.
Immobilization device
Your radiation therapists may make you an immobilization device. It will help you stay in the same exact position for all your treatments. It may be attached to the simulation or treatment table, depending on your position.
If you have an immobilization device, you’ll use it during your simulation and all your treatments.
Skin markings and tattoos
Your radiation therapists will use a felt marker to draw on your skin in the treatment area. They may also make permanent skin markings called tattoos once they’re sure you’re in the right position. They’ll make the tattoos using a clean needle and a drop of ink. Each one will feel like a pinprick. The tattoos will not be bigger than the head of a pin.
Your radiation therapists will take several photos of you in your simulation position after they make the markings. Your care team will use the photos and markings to position you correctly on the treatment table each time.
You can wash off the felt markings after your simulation. The tattoos are permanent and will not wash off. Talk with your radiation oncologist if you’re concerned about having tattoos as part of your radiation therapy.
What to expect after your simulation
We will schedule your set-up procedure and first treatment at the end of your simulation appointment.
Scheduling your treatments
Most people have treatments every weekday. You will have treatments for about _______ weeks.
Most people have treatments every weekday. Your care team will tell you how many weeks your radiation therapy will last.
Call your radiation oncologist’s office to tell your care team if you can’t come in for treatment for any reason. Talk with your radiation therapist or scheduler if you need to change your schedule for any reason.
Checking your treatment schedule
You can see your treatment schedule in your patient portal, MSK MyChart. If you do not have a MSK MyChart account, you can sign up at mskmychart.mskcc.org. You can also ask a member of your care team to send you an invitation.
It’s very helpful to use MSK MyChart to keep track of your appointment times. We will call you if we need to reschedule any of your treatment appointments.
Treatment planning
Between your simulation and first treatment, your radiation oncologist will work with a team to plan your treatments. They will use your simulation scans to plan the angles and shapes of your radiation beams. They will also determine the dose of radiation that you will receive. They carefully plan and check all the details of your treatments. This takes 7 to 10 business days.
What happens during radiation therapy to your lymph nodes
You’ll be in the same position for your radiation treatments as you were for your simulation. You may want to take pain or anxiety medicine before your radiation treatments if it was helpful for your simulation. Take it about 1 hour before your appointment.
Wear comfortable clothes that are easy to take off. You will need to change into a hospital gown.
Your treatment appointments
Each day you have treatment, check in at the reception desk and have a seat in the waiting room. Your radiation therapists will ask you to change into a hospital gown when they’re ready for you. Keep your shoes on.
Your radiation therapists will bring you into the treatment room and help you lie on the treatment table (see Figure 2). They will position you exactly how you were lying during your simulation.

Set-up procedure and first treatment
When you come for your first treatment appointment, you’ll have imaging scans before your treatment starts. These scans are called the set-up procedure. It usually takes about 40 minutes.
Radiation treatments
You will have special imaging scans (x-rays or CT scans) during each of your treatment appointments. These are to make sure your position and the treatment area are correct. They are not to check how your tumor is responding to the radiation therapy.
Your radiation therapists will do their best to make sure you’re comfortable in your treatment position. Once everything is ready, they’ll leave the room and start your treatment.
Do not move during your treatment. Your radiation therapists may give you instructions for breathing during your treatment, but most people can breathe normally.
You will not see or feel the radiation. You may hear the machine as it moves around you and is turned on and off.
You will be alone in the room during your treatment, but your radiation therapists will see you on a monitor and hear you through an intercom the whole time. Tell them if you’re uncomfortable or need help.
You will be in the treatment room for about 30 minutes, depending on your treatment plan. You’ll spend most of this time getting into your treatment position. The actual treatment only takes a few minutes.
You will not be radioactive during or after your radiation treatments. It is safe for you to be around other people and pets.
Status check visits
Your radiation oncologist or a radiation nurse will check in with you every week during your radiation therapy. They’ll talk with you about any concerns, ask about any side effects you’re having, and answer your questions. This status check visit may be a telemedicine visit or a visit before or after your treatment.
Call your radiation oncologist’s office if you need to speak with your radiation oncologist or radiation nurse outside your status check visit. You can also ask another member of your radiation care team to contact them when you come in for treatment.
Vitamins and dietary supplements during radiation therapy
It’s OK to take a multivitamin during your radiation therapy. Do not take more than the recommended daily allowance (RDA) of any vitamin or mineral.
Do not take any other dietary supplements without talking with a member of your care team. Vitamins, minerals, and herbal or botanical (plant-based) supplements are examples of dietary supplements.
Side effects of radiation therapy to your lymph nodes
You may have side effects from your radiation therapy. This section has information about the most common side effects. You may have all, some, or none of them.
Your nurse will talk with you about the side effects you’re most likely to have. The ones you have and how strong they are depends on many things, such as:
- The dose of radiation you’re getting.
- The number of radiation treatments you’re getting,
- If you’re getting chemo and radiation therapy at the same time.
- Your overall health.
You may start to notice side effects about 2 weeks after your first treatment. They may get worse as you go through your radiation therapy. They will slowly get better over several weeks after you finish radiation therapy. Some side effects may take longer to go away.
You and your radiation therapy care team will work together to prevent and manage side effects. Follow the guidelines in this section to help manage your side effects during and after treatment.
Skin and hair reactions
Your skin and hair in the treatment area may change during your radiation therapy. This is normal.
- Your skin may become pink or tanned after 2 to 3 weeks. It may become bright red or very dark later on, based on your skin tone.
- Your skin may feel dry and itchy and look flaky. Sensitive areas may blister, open, and peel. Tell a member of your care team if this happens.
- You may get a rash, especially in areas where your skin has been in the sun. Tell a member of your care team if you get a rash. They can be a sign of an infection.
- You may lose some or all of your hair in the treatment area. Hair most often grows back 3 to 6 months after you finish radiation therapy.
Your radiation nurse may put special dressings or creams on your skin. They will also teach you how to care for your skin on your own. If your skin reactions are very bad, your radiation oncologist may stop your treatments until your skin heals.
Skin reactions sometimes get worse during the week after your last treatment. Call your radiation oncologist or nurse if this happens. Your skin will heal over time once you finish radiation therapy, but it often takes 3 to 4 weeks.
These guidelines can help you care for your skin during your radiation therapy. Follow them until your skin gets better. These guidelines are only for your skin in the radiation treatment area. You can care for the rest of your skin as usual.
Keep your skin clean
- Bathe or shower every day.
- Use warm water and a mild unscented soap, such as Neutrogena®, Dove®, baby soap, Basis®, or Cetaphil®.
- Be gentle with your skin when you wash it. Do not use a washcloth, loofah, or brush.
- Rinse your skin well.
- Pat your skin dry with a soft, clean towel.
- Your radiation therapists may outline your treatment area with a purple felt-tipped marker. You can remove these markings with mineral oil when your radiation therapists say it’s OK.
- Do not use alcohol or alcohol pads on your skin.
Keep your skin moisturized
- Moisturize your skin 2 times every day.
- Use a moisturizer without fragrances or lanolin. Lanolin is an oil made by animals that have wool, such as sheep. It can make your skin more sensitive.
- There are many over-the-counter (not prescription) moisturizers that are good to use. Your radiation nurse may suggest one. Ask them if you’re not sure which one to use.
- Only use 1 moisturizer at a time unless your radiation nurse tells you to use more.
Avoid irritating your skin
- Wear loose-fitting cotton clothing. Do not wear tight clothing that will rub against your skin.
- Only use the moisturizers, creams, or lotions your radiation oncologist or nurse suggests.
- Do not use makeup, perfume, cologne, powder, or aftershave.
- Do not use deodorant if your skin is broken, cracked, or irritated. You can use deodorant on intact (not broken) skin. Stop using it if your skin becomes irritated.
- Do not scratch your skin if it’s itchy. Put on moisturizer. Ask your radiation nurse about ways to ease the itching.
- Avoid shaving your skin. If you must shave, use an electric razor. Stop if your skin becomes irritated.
- Do not put anything sticky (such as Band-Aids® or medical tape) on your skin.
- Do not expose your skin to very hot or cold temperatures. For example, do not use hot tubs, hot or cold water bottles, heating pads, or ice packs.
- Only swim in a pool if you do not have any skin reactions. Rinse off right after you get out.
- Avoid tanning or burning your skin. Use a sunblock with an SPF of 30 or higher if you’re going to be in the sun. Wear loose-fitting clothing over as much of your skin as you can.
Fatigue
Fatigue is feeling very tired or weak. When you feel fatigued, you may not want to do things. You may have trouble focusing, feel slowed down, or have less energy than usual. Fatigue can range from mild (not bad) to severe (very bad). It may be worse at certain times of day.
You may start to feel fatigued after 2 to 3 weeks of treatments. You may still feel fatigued for a few weeks to several months after finishing radiation therapy. Fatigue usually gets better over time.
There are lots of reasons you may feel fatigued during your radiation therapy. They include:
- The radiation’s effects on your body.
- Traveling to and from your treatment appointments.
- Not getting enough restful sleep at night.
- Not getting enough protein and calories.
- Having pain or other symptoms.
- Feeling anxious (nervous) or depressed (unhappy).
- Side effects of some medicines.
Ways to manage fatigue
- If you’re working and are feeling well, it’s OK to keep working. But working less may help you have more energy.
- Plan your daily activities. Pick the things you need or really want to do. Do them when you have the most energy. For example, you may choose to go to work but not do housework. You may choose to watch your child’s after-school event but not go out to dinner.
- Plan time to rest or take short (10- to 15-minute) naps during the day, especially when you feel more tired.
- Try to sleep at least 8 hours every night. This may be more sleep than you needed before you started radiation therapy. You may find it helpful to:
- Go to sleep earlier and get up later.
- Be active during the day. For example, if you’re able to exercise, you could go for a walk or do yoga.
- Relax before going to bed. For example, read a book, work on a puzzle, listen to music, or do another calming hobby.
- Ask family and friends to help with chores and errands. Check with your health insurance company to see if they cover home care services.
- You might have more energy when you exercise. Ask your radiation oncologist if you can do light exercise, such as walking, biking, stretching, or yoga. Read Managing Cancer-Related Fatigue with Exercise (www.mskcc.org/pe/fatigue-exercise) to learn more.
- Eat foods that are high in protein and calories. Read Eating Well During Your Cancer Treatment (www.mskcc.org/pe/eating-cancer-treatment) to learn more.
Some things can make your fatigue worse. Examples are:
- Pain
- Nausea (feeling like you’re going to throw up)
- Diarrhea (loose or watery poop)
- Trouble sleeping
- Feeling depressed or anxious
Ask your radiation oncologist or nurse for help if you have these or any other symptoms or side effects.
Changes to your blood cell counts
Your blood cell count is how many blood cells you have.
You may have lowered blood cell counts (fewer blood cells) if there are large areas of bone marrow in the treatment area. Bone marrow is the soft tissue inside your bones that makes blood cells. Chemo can also lower your blood cell count.
You have 3 kinds of blood cells:
- White blood cells. These fight off infection.
- Platelets. These help your blood clot when you injure yourself.
- Red blood cells. These carry the oxygen you need for energy.
CBC blood tests
You’ll have a blood test called a CBC (complete blood count) about once a week during your radiation therapy. The CBC counts the red blood cells, white blood cells, and platelets in a sample of your blood. It helps your care team keep track of your blood cell counts.
Low blood counts
If your blood counts get too low, your radiation oncologist may decide to stop your treatments until they get back to higher levels. They may also give you an injection to help raise your white blood cell count, if needed. We will tell you what to do if your blood counts get too low.
Call your healthcare provider right away if you have:
- A fever of 100.5 °F (38 °C) or higher
- Shaking chills
- Flu-like symptoms
- Bleeding
These things can mean you have an infection.
Appetite loss
Appetite loss is when you feel less hunger than usual. Sometimes, you may not feel hunger at all.
You may have appetite loss during your radiation therapy. But it’s important that your body gets protein and calories even if you don’t feel hungry. It uses these nutrients to repair normal cells injured from radiation. Also, if you use a mold during your treatments, it may not fit correctly if your weight changes. Try not to lose weight during your radiation therapy.
Be selective about what you eat to be sure you get enough calories and protein. We will give you Eating Well During Your Cancer Treatment (www.mskcc.org/pe/eating-cancer-treatment). It has many tips to add calories and protein to your diet. You can also use these tips:
- Try to eat small meals often throughout the day.
- If you never seem to feel hungry, set up a schedule to make sure you eat regularly. For example, set a schedule to eat every 2 hours.
- Eat your meals in a calm place. Take your time eating. Eat with family or friends whenever you can.
- Choose foods with different colors and textures to make your meals more appealing.
- Bring snacks and drinks to your treatment appointments. You can have them while you’re waiting or while you’re coming to and from your appointments.
- Drink liquid nutritional supplements if you’re not eating enough food. There are many products available, and they come in many flavors. Ask your healthcare provider which product is best for you.
Sexual health
You may have concerns about how cancer and your treatment can affect your sex life. You are not radioactive. You can’t pass radiation to anyone else. It’s safe to be in close contact with others.
You can be sexually active during your radiation therapy, unless your radiation oncologist gives you other instructions. If you or your partner are able to have children, you must use birth control (contraception) to prevent pregnancy during your radiation therapy.
Talking with your radiation oncologist or nurse about your sexual health can be hard, but it’s an important conversation to have. They may not bring it up unless you share your questions and concerns. You may feel uncomfortable, but most people in cancer treatment have similar questions. We work hard to make sure everyone in our care feels welcome.
Sexual health programs
MSK offers sexual health programs. These programs can help you manage the ways your cancer or cancer treatment affects your sexual health or fertility. Our specialists can help you address sexual health or fertility issues before, during, or after your radiation therapy.
- To learn about our Female Sexual Medicine & Women’s Health Program or to make an appointment, call 646-888-5076.
- To learn about our Male Sexual & Reproductive Medicine Program or to make an appointment, call 646-888-6024.
- To learn about our Cancer and Fertility Program, talk with your healthcare provider.
Other sexual health resources
Read Sex and Your Cancer Treatment (www.mskcc.org/pe/sex-cancer-treatment) to learn more about sexual health during cancer treatment.
The American Cancer Society also has resources about sexual health issues during cancer treatment. They’re called Sex and the Adult Male with Cancer and Sex and the Adult Female with Cancer. You can search for them at www.cancer.org or call 800-227-2345 for a copy.
Emotional health
|
|
|
You might also worry about telling your employer you have cancer or about paying your medical bills. You may worry about how your family relationships may change, or that the cancer will come back. You may worry about how cancer treatment will affect your body, or if you will still be sexually attractive.
It’s normal and OK to worry about all these things. All these kinds of feelings are normal when you or someone you love has a serious illness. We’re here to support you.
Ways to cope with your feelings
Talk with others. When people try to protect each other by hiding their feelings, they can feel very alone. Talking can help the people around you know what you’re thinking. It might help to talk about your feelings with someone you trust. For example, you can talk with your spouse or partner, close friend, or family member. You can also talk with a chaplain (spiritual advisor), nurse, social worker, or psychologist.
Join a support group. Meeting other people with cancer will give you a chance to talk about your feelings and learn from others. You can learn how other people cope with their cancer and treatment and be reminded you’re not alone.
We know that all cancer diagnoses and people with cancer are not the same. We offer support groups for people who share similar diagnoses or identities. For example, you can join a support group for people with breast cancer or for LGBTQ+ people with cancer. Visit www.msk.org/vp to learn about MSK’s support groups. You can also talk with your radiation oncologist, nurse, or social worker.
Try relaxation and meditation. These kinds of activities can help you feel relaxed and calm. You might try thinking of yourself in a favorite place. While you do, breathe slowly. Pay attention to each breath or listen to soothing music or sounds. For some people, praying is another way of meditation. Visit www.msk.org/meditations to find guided meditations lead by our Integrative Medicine and Wellness providers.
Exercise. Many people find that light movement, such as walking, biking, yoga, or water aerobics, helps them feel better. Talk with your healthcare provider about types of exercise you can do.
We all have our own way of dealing with tough situations. Often, we do what worked for us in the past. But sometimes that’s not enough. We encourage you to talk with your doctor, nurse, or social worker about your concerns.
Site-specific side effects of radiation therapy to your lymph nodes
You may also have side effects based on the area being treated. Your nurse will mark the site-specific side effects you may have.
You may also have side effects based on the area being treated. Your nurse will talk with you about which of these site-specific side effects you may have.
Mouth and throat changes
Your treatments may cause changes in your mouth and throat. You may have:
- Pain in your mouth, throat, or both
- Sores in your mouth, throat, or both
- Pain when you swallow
- Trouble swallowing
- Thicker saliva (spit) than usual
- Dry mouth
- Taste changes
Follow the guidelines below to help manage these side effects.
- Brush your teeth after you eat and before you go to bed. Use a soft-bristle toothbrush. Use the toothpaste your dentist recommended or a mild toothpaste that has fluoride.
- If you have dentures, a bridge, or a dental prosthesis, take it out and clean it each time you clean your mouth. Leave it out while you sleep. If your mouth becomes irritated, keep it out of your mouth as much as you can.
- If you floss your teeth now, keep flossing once a day before you go to bed. If you do not floss now, do not start during your radiation therapy.
Rinse your mouth every 4 to 6 hours, or more often for comfort. Use 1 of these liquids:
- One quart (4 cups) of water mixed with 1 teaspoon of salt and 1 teaspoon of baking soda.
- One quart of water mixed with 1 teaspoon of salt.
- One quart of water mixed with 1 teaspoon of baking soda.
- Water.
- A mouthwash with no alcohol or sugar.
To rinse, swish and gargle the liquid for 15 to 30 seconds, then spit it out.
- Use a lip moisturizer after you care for your mouth. Do not use lip moisturizer for 4 hours before your treatments.
If your mouth is dry, try these suggestions:
- Use a mouth moisturizer.
- Take sips of water or other liquids (such as coconut water, almond milk, Gatorade®, and broth) often during the day. It may be helpful to carry a bottle of water.
- Use an aerosol pump spray bottle filled with water to moisten your mouth.
- Use a humidifier, especially at night. Be sure to change the water in the humidifier and clean it as directed.
- Avoid using air conditioners.
If you start having trouble swallowing or pain when you swallow, tell your healthcare provider. They can prescribe medicine to make you more comfortable.
As you get side effects, your doctor may ask you to see your nurse every day. Your nurse will look at your mouth and spray your mouth, if needed.
Changes inside your nose
You may have changes inside your nose, such as:
- Dry nose.
- Stuffy nose.
- Occasional minor (not bad) nosebleeds.
Keep the inside of your nose moist to help manage these side effects. You can do this using saline nose spray, a humidifier, or both.
Ear pain
You may have ear pain from the swelling your treatments causes. If you do, tell your healthcare provider. Ear pain can also be a sign of infection.
Do not try to clean or clear out your ears. Do not use cotton swabs (such as Q-tips®) inside your ears.
Voice changes (hoarseness)
You may have hoarseness from swelling your treatments causes. Your voice may be more breathy, strained, rough, or high or low pitched. To help manage voice changes:
- Rest your voice as much as you can.
- Do not whisper. Whispering can strain your vocal cords.
- Use a humidifier.
- Gargle with one of the liquids listed in the “Mouth and throat changes” section.
Trouble eating and drinking
Many side effects of radiation therapy can make it hard to eat and drink. This can cause weight loss, fatigue, and dehydration.
If your weight changes, the immobilization device you use during your treatments may not fit how it should. This can make it harder to stay in the right position for your treatments. Follow these guidelines to help keep your weight from changing.
Change what you eat and drink based on your side effects
If you have mouth or throat pain or soreness or trouble swallowing:
- Eat soft, moist, bland foods. Take small bites and chew the food well.
- Use sauces and gravies to soften foods.
- Blend or purée your foods to change the texture.
- Avoid things that may irritate your mouth and throat, such as:
- Very hot foods and liquids.
- Dry, hard, and coarse foods, such as chips, pretzels, crackers, and raw vegetables.
- Spices, such as pepper, chili, horseradish, hot sauce, and curry.
- Acidic or citrus foods and juices, such as orange, grapefruit, lemon, lime, pineapple, and tomato.
- Alcohol.
- Tobacco.
If your mouth is dry:
- Rinse your mouth before eating.
- Use gravies and sauces to prepare your food.
- Drink liquids while eating dry foods, such as rice or bread.
If you have appetite loss:
- Eat small meals often throughout the day. If you never seem to feel hungry, set up a schedule to make sure you eat regularly.
- Choose foods and drinks with lots of calories and protein. Avoid foods and drinks that are filling but do not have many calories or protein.
- Eat your meals in a calm place. Take your time while eating. Eat with family or friends whenever you can.
- Bring snacks and drinks to your treatment appointments. You can have them while you’re waiting or while you’re coming to and from your appointments each day.
If you have nausea:
- Tell your healthcare provider. They may prescribe medicine to help.
- Eat foods that are less likely to upset your stomach, such as:
- Foods at room temperature or cooler.
- Cooled or chilled liquids.
- Dry, starchy foods, such as toast, soda crackers, melba toast, dry cereal, pretzels, and angel food cake.
- Yogurt, sherbet, and clear liquids, such as apple juice, Jell-O®, and ginger ale.
- Cold baked or broiled chicken or turkey with the skin removed.
- Soft fruits and vegetables.
- Avoid foods and liquids that may make nausea worse, such as:
- Hot foods with strong odors (smells).
- Spicy, fatty, greasy, and fried foods.
- Very sweet foods.
- Acidic or citrus foods and juices, such as orange, grapefruit, pineapple, and tomato.
- Alcohol.
Get enough nutrition during your radiation therapy
- Eat a well-balanced diet that’s high in calories and protein. This will help you stay around the same weight and feel better during your radiation therapy. Your dietitian will work with you to help you choose the best foods and liquids.
- Use liquid nutritional supplements. There are lots of products and flavors you can try. Talk with your doctor, nurse, or dietitian about which one is best for you.
- Take a daily multivitamin, if you want.
- Read the multivitamin’s label. Do not take more than the recommended daily amount (RDA) of any vitamin or mineral.
- Do not take any other dietary supplements (such as vitamins and herbal supplements) without talking with your doctor.
Read Eating Well During Your Cancer Treatment (www.mskcc.org/pe/eating-cancer-treatment) to learn more about eating during treatment.
Watch Nutrition Before and During Treatment for Head and Neck Cancer (www.mskcc.org/pe/hn-nutrition-before-radiation) to learn more about getting enough nutrition before, during, and after radiation therapy to your head and neck.
Diarrhea
Your bowel movements may change during your radiation therapy. You may have more bowel movements and softer stools than usual. You may also develop diarrhea. These side effects can start during the first few weeks of your radiation therapy and last until 2 to 4 weeks after your last treatment.
Here are guidelines to help you manage diarrhea and other changes in your bowel movements. Follow these guidelines until your bowel movements go back to normal.
- Eat foods that are low in fiber, low in fat, and lactose-free. Your nurse will give you . This resource has information about what foods to eat. When your bowel movements go back to your normal pattern, you can slowly start adding foods from your usual diet.
- Try to drink 8 to 12 cups (2 to 3 quarts) of liquids throughout the day. This will help replace the water and salts you lose in your bowel movements.
- Choose drinks such as Gatorade®, juices, and nectars. It’s best to dilute them (add a little bit of water) first so they’re not too strong. Non-fat soup broth and Pedialyte® are also good choices.
- Limit drinks with caffeine, such as coffee, tea, and colas. Caffeine can make you more dehydrated.
- Eat bananas and potatoes without the skin. They help replace important salts you may lose when you have diarrhea.
- Avoid any foods or drinks that makes your symptoms worse.
- Take medicine for diarrhea, such as loperamide (Imodium®). You can buy it a pharmacy without a prescription. Your doctor may prescribe other medicines.
Cough or shortness of breath
You may get a cough or start to feel shortness of breath anytime during or after your radiation therapy. Call your healthcare provider if you start to have a cough or shortness of breath. Call your healthcare provider if you have a cough or shortness of breath and it gets worse.
Here are suggestions to help you feel more comfortable if you have a cough or shortness of breath.
- Do not smoke. Smoking irritates the lining of your airway and causes more coughing. If you want help to stop smoking, your nurse can refer you to our Tobacco Treatment Program. You can also reach the program by calling 212-610-0507.
- Use 1 or 2 pillows to prop up your upper body while you sleep.
- Use a humidifier while you sleep. Be sure to change the water and clean the humidifier often. Follow the manufacturer’s instructions.
- Fatigue may make your shortness of breath worse. Follow the suggestions in the “Fatigue” section to help minimize your fatigue.
- Use cough medicine following your doctor’s instructions.
What happens after radiation therapy to your lymph nodes
Follow-up appointments
It’s important to come to all your follow-up appointments with your radiation oncologist. During these appointments, they will check how you’re recovering after your radiation therapy.
Write down your questions and concerns before your follow-up appointments. Bring this and a list of all your medicines with you. You can also call your radiation oncologist or nurse any time after you finish radiation therapy or between follow-up appointments.
Vitamins and dietary supplements after radiation therapy
- You might be getting other cancer treatments along with your radiation therapy. If you are, ask the doctor managing that treatment when it’s safe to start taking dietary supplements again. Some dietary supplements are not safe to take before surgery or during chemotherapy.
- If you are not getting other cancer treatments, you can start taking dietary supplements again 1 month after your last radiation treatment.
Tell your radiation nurse if you want to talk with a clinical dietitian nutritionist about your diet or supplements.
Late side effects after radiation therapy to your lymph nodes
You may have some side effects many months or years after you finish radiation therapy.
The exact side effects you may have depends on the area that was treated. Your nurse will mark the long-term side effects you may have. They will also give you more information after you finish radiation therapy.
The exact side effects you may have depends on the area that was treated. Your nurse will talk with you about the long-term side effects you may have. They will also give you more information after you finish radiation therapy.
- Changes in your thyroid hormone levels.
- A tingling feeling down your arms and legs when you bend your neck forward. This is called Lhermitte’s Syndrome. It will go away on its own.
- Shingles. People who get shingles usually get it within 1 to 2 years after radiation therapy.
- Radiation injury to your heart and the blood vessels in your heart. This is rare.
- Lung inflammation. This is called radiation pneumonitis. People who get radiation pneumonitis usually get it 1 to 3 months after finishing radiation therapy.
- Changes in fertility and hormone production.
- If your ovaries are in the treatment area, they may be affected. How they’re affected and when they start to be affected depends on your specific treatment plan. You may be able to have an operation to move your ovaries out of the treatment area. If this is an option for you, your clinical team will give you more information.
- If your testes are in the treatment area, they may be affected as soon as you start treatment.
- If you want to have children in the future, tell your clinical team before you start radiation therapy.
When to call your radiation oncologist or nurse
Contact your radiation oncologist or radiation nurse if you have:
- A fever of 100.4 °F (38 °C) or higher.
- Chills.
- Painful, peeling, blistering, moist, or weepy skin.
- Discomfort in the treated area.
- Any new or unusual symptoms.
Contact information
If you have questions or concerns, contact a member of your radiation therapy team. You can reach them Monday through Friday from to at these numbers.
Radiation oncologist: _____________________
Phone number: _________________________
Radiation nurse: ________________________
Phone number: _________________________
Outside those hours, you can leave a message or talk with another MSK provider. There is always a doctor or nurse on call. If you’re not sure how to reach your healthcare provider, call 212-639-2000.
Support services
MSK support services
Counseling Center
www.msk.org/counseling
646-888-0200
Many people find that counseling helps them. Our counseling center offers counseling for individuals, couples, families, and groups. We can also prescribe medicines to help if you feel anxious or depressed. Ask your healthcare provider for a referral or call the number above to make an appointment.
Integrative Medicine and Wellness Service
www.msk.org/integrativemedicine
Our Integrative Medicine and Wellness Service offers many services to complement (go along with) traditional medical care, including music therapy, mind/body therapies, dance and movement therapy, yoga, and touch therapy. Call 646-449-1010 to schedule an appointment for these services.
You can also schedule a consultation with a healthcare provider in the Integrative Medicine and Wellness Service. They will work with you to come up with a plan for creating a healthy lifestyle and managing side effects. Call 646-608-8550 to make an appointment.
Nutrition Services
www.msk.org/nutrition
212-639-7312
Our Nutrition Service offers nutritional counseling with one of our clinical dietitian nutritionists. Your clinical dietitian nutritionist will talk with you about your eating habits. They can also give advice on what to eat during and after treatment. Ask a member of your care team for a referral or call the number above to make an appointment.
Rehabilitation Services
www.msk.org/rehabilitation
Cancers and cancer treatments can make your body feel weak, stiff, or tight. Some can cause lymphedema (swelling). Our physiatrists (rehabilitation medicine doctors), occupational therapists (OTs), and physical therapists (PTs) can help you get back to your usual activities.
- Rehabilitation medicine doctors diagnose and treat problems that affect how you move and do activities. They can design and help coordinate your rehabilitation therapy program, either at MSK or somewhere closer to home. call Rehabilitation Medicine (Physiatry) at 646-888-1929 to learn more.
- An OT can help if you’re having trouble doing usual daily activities. For example, they can recommend tools to help make daily tasks easier. A PT can teach you exercises to help build strength and flexibility. Call Rehabilitation Therapy at 646-888-1900 to learn more.
Resources for Life After Cancer (RLAC) Program
646-888-8106
At MSK, care does not end after your treatment. The RLAC Program is for patients and their families who have finished treatment.
This program has many services. We offer seminars, workshops, support groups, and counseling on life after treatment. We can also help with insurance and employment issues.
Sexual Health Programs
Cancer and cancer treatments can affect your sexual health, fertility, or both. MSK’s sexual health programs can help you before, during, or after your treatment.
- Our Female Sexual Medicine & Women’s Health Program can help with sexual health problems such as premature menopause or fertility issues. Ask a member of your MSK care team for a referral or call 646-888-5076 to learn more.
- Our Male Sexual & Reproductive Medicine Program can help with sexual health problems such as erectile dysfunction (ED). Ask a member of your care team for a referral or call 646-888-6024 to learn more.
Tobacco Treatment Program
www.msk.org/tobacco
212-610-0507
MSK has specialists who can help you quit smoking. Visit our website or call the number above to learn more. You can also ask your nurse about the program.
Virtual Programs
www.msk.org/vp
Our Virtual Programs offer online education and support for patients and caregivers. These are live sessions where you can talk or just listen. You can learn about your diagnosis, what to expect during treatment, and how to prepare for your cancer care.
Sessions are private, free, and led by experts. Visit our website for more information about Virtual Programs or to register.
Radiation therapy support services
American Society for Therapeutic Radiology and Oncology
www.rtanswers.org
800-962-7876
This website has detailed information about treating cancer with radiation. It also has contact information for radiation oncologists in your area.
External support services
There are many other support services to help you before, during, and after your cancer treatment. Some offer support groups and information, while others can help with transportation, lodging (a place to stay), and treatment costs.
For a list of these support services, read External Support Services (www.mskcc.org/pe/external_support_services). You can also talk with an MSK social worker by calling 212-639-7020.
Questions to ask your radiation oncologist
Before your appointment, it’s helpful to write down questions you want to ask. Examples are listed below. Write down the answers during your appointment so you can review them later.
What kind of radiation therapy will I get?
How many radiation treatments will I get?
What side effects should I expect during my radiation therapy?
Will these side effects go away after I finish my radiation therapy?
What kind of late side effects should I expect after my radiation therapy?