This information explains why staging the mediastinal (MEE-dee-uh-STY-nul) lymph nodes is an important part of your lung cancer treatment.
About your mediastinum
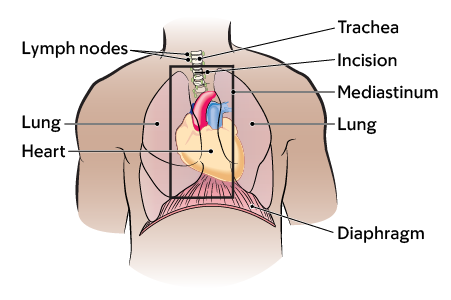
The area in the middle of your chest between your lungs is called your mediastinum (see Figure 1). Your mediastinum is made up of:
- Your heart.
- Your trachea (windpipe).
- Your esophagus (food pipe).
- Lymph nodes (small, bean-shaped glands that help fight infection and cancer).
About staging mediastinal lymph nodes
Staging is part of the diagnosis process. It tells us how advanced a cancer is. It describes the tumor’s size, location, and how far it has spread. Staging helps your care team choose the best treatment and follow-up care for you.
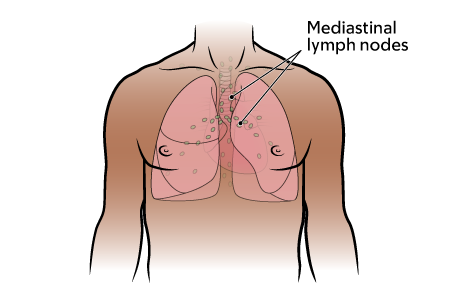
It is common for lung cancer to spread to the lymph nodes in your chest (see figure 2). Your healthcare provider will use these imaging tests to examine your chest:
- Computed Tomography (CT) Scan (www.mskcc.org/pe/ct_scan)
- Positron emission tomography (PET) scan
The images from these tests will help your healthcare provider find any tumors you may have. If there are tumors, the images will show where they’re located and their size.
Your doctor will give you a physical exam and review the results of your diagnostic and imaging tests. Then they will decide the stage of the cancer. They may also do a biopsy to find out if the tumors have spread to your lymph nodes. This means they will take a small tissue sample to look at it more closely.
Mediastinal staging procedures
Your healthcare provider will recommend one of the staging procedures below. Some people need both procedures. Talk with your healthcare provider about which procedure is right for you.
Endobronchial ultrasound (EBUS)
During EBUS, your healthcare provider will look into your bronchioles (air tubes) using a bronchoscope. A bronchoscope is a thin, flexible tube with a light on the end.
They will put this through your mouth and use it to see the lymph nodes next to your bronchioles. Then, they will pass a needle through the bronchoscope to take tissue samples from your lymph nodes.
Mediastinoscopy
During mediastinoscopy (MEE-dee-uh-sty-NOS-koh-pee), your healthcare provider will make a small (about 1 inch) incision in the front of your lower neck. An incision is a surgical cut.
They will place a mediastinoscope (MEE-dee-uh-STY-noh-skope) into your chest through the incision. A mediastinoscope is a thin, flexible tube with a light and camera on the end. They will use this to examine your chest.
Then, your healthcare provider will get samples of any important areas to check for cancer or other conditions.
They will close your incision with stitches that dissolve over time. They may also put Dermabond® (surgical glue), or a Steri-Strip™ (tape) and a small gauze dressing (bandage) over your incision.
Getting ready for your procedure
Ask about your medicine
You may need to stop taking some of your medicine before your procedure. We’ve included some common examples below. For instructions about which medicine you can take on the morning of your procedure, talk with your healthcare provider. If you have any questions about your medicine, ask your healthcare provider.
Follow your healthcare provider’s instructions for taking aspirin
Aspirin can cause bleeding. If you take aspirin or a medicine that has aspirin, you may need to change your dose or stop taking it 7 days before your procedure. Follow your healthcare provider’s instructions. Do not stop taking aspirin unless they tell you to.
To learn more, read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil (www.mskcc.org/pe/check-med-supplement).
Stop taking vitamin E, multivitamins, herbal remedies, and other dietary supplements
Vitamin E, multivitamins, herbal remedies, and other dietary supplements can cause bleeding. Stop taking them 7 days before your procedure. If your healthcare provider gives you other instructions, follow those instead.
To learn more, read Herbal Remedies and Cancer Treatment (www.mskcc.org/pe/herbal_remedies).
Stop taking nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs, such as ibuprofen (Advil® and Motrin®) and naproxen (Aleve®), can cause bleeding. Stop taking them 2 days before your procedure. If your healthcare provider gives you other instructions, follow those instead.
To learn more, read How To Check if a Medicine or Supplement Has Aspirin, Other NSAIDs, Vitamin E, or Fish Oil (www.mskcc.org/pe/check-med-supplement).
If you have pain or discomfort, take acetaminophen (Tylenol®). Do not take more acetaminophen than directed on the label or as instructed by your healthcare provider.
Follow your healthcare provider’s instructions for taking anticoagulants (blood thinners)
If you take medicine to thin your blood, you’ll need to stop taking it before your procedure. When you need to stop taking it depends on the medicine you take.
Examples of common blood thinners are listed below. There are others, so be sure your care team knows all the medicine you take. Do not stop taking your blood thinner without talking with a member of your care team.
|
|
Medicine for diabetes
If you take insulin or other medicine for diabetes, you may need to change the dose. Talk with your surgeon and the healthcare provider who prescribes your diabetes medicine about what do the morning of your procedure.
Get a letter from your cardiologist, if needed
If you have an automatic implantable cardioverter-defibrillator (AICD), you’ll need a clearance letter from your cardiologist before your procedure. A cardiologist is a doctor with special training in the cardiovascular system (heart and blood vessels).
Arrange for someone to take you home
You must have a responsible care partner take you home after your procedure. A responsible care partner is someone who can help you get home safely. They should be able to contact your care team if they have any concerns. Make sure to plan this before the day of your procedure.
If you don’t have a responsible care partner to take you home, call one of the agencies below. They’ll send someone to go home with you. There’s a charge for this service, and you’ll need to provide transportation. It’s OK to use a taxi or car service, but you still need a responsible care partner with you.
| Agencies in New York | Agencies in New Jersey |
| VNS Health: 888-735-8913 | Caring People: 877-227-4649 |
| Caring People: 877-227-4649 |
Presurgical testing (PST)
You’ll have a PST appointment before your procedure. You’ll get a reminder from your healthcare provider’s office with the appointment date, time, and location.
You can eat and take your usual medicine(s) the day of your PST appointment.
It’s helpful to bring these things to your appointment:
- A list of all the medicines you’re taking, including prescription and over-the-counter medicines, patches, and creams.
- Results of any medical tests done outside of MSK in the past year, if you have them. Examples include results from a cardiac stress test, echocardiogram, or carotid doppler study.
- The names and telephone numbers of your healthcare providers.
You’ll meet with an advance practice provider (APP) during your PST appointment. They work closely with MSK’s anesthesiology (A-nes-THEE-zee-AH-loh-jee) staff. These are doctors with special training in using anesthesia during a procedure.
Your APP will review your medical and surgical history with you. You may have tests to plan your care, such as:
- An electrocardiogram (EKG) to check your heart rhythm.
- A chest X-ray.
- Blood tests.
Your APP may recommend you see other healthcare providers. They’ll also talk with you about which medicine(s) to take the morning of your procedure.
What to do the day before your procedure
Note the time of your procedure
A staff member will call you after the day before your procedure. If your procedure is scheduled for a Monday, they’ll call you on the Friday before. If you do not get a call by , call 212-639-5014.
The staff member will tell you what time to arrive for your procedure. They’ll also remind you where to go.
If you need to cancel your procedure for any reason, please call the healthcare provider who scheduled it for you.
Instructions for eating and drinking: 8 hours before your arrival time
|
What to do the day of your procedure
Instructions for drinking: 2 hours before your arrival time
| Stop drinking 2 hours before your arrival time. This includes water. |
Things to remember
- Take only the medicine your healthcare provider told you to take the morning of your procedure. Take them with a few sips of water.
- Don’t put on any lotion, cream, powder, deodorant, makeup, or perfume.
- Don’t wear any metal objects. Remove all jewelry, including body piercings. The equipment used during your procedure can cause burns if it touches metal.
- Leave all valuables, such as credit cards and jewelry, at home.
- If you wear contacts, wear your glasses instead.
What to bring with you
- Medicine for breathing problems (such as inhalers), if you take any.
- Medicine for chest pain, if you take any.
- A case for your personal items, if you have one. This includes glasses or contacts, hearing aid(s), dentures, prosthetic device(s), wig, or religious articles.
- Your Health Care Proxy form and other advance directives, if you have filled them out.
Where to park
MSK’s parking garage is on East 66th Street between York and 1st avenues. If you have questions about prices, call 212-639-2338.
To get to the garage, turn onto East 66th Street from York Avenue. The garage is about a quarter of a block in from York Avenue. It’s on the right (north) side of the street. There’s a tunnel you can walk through that connects the garage to the hospital.
There are other parking garages on:
- East 69th Street between 1st and 2nd avenues.
- East 67th Street between York and 1st avenues.
- East 65th Street between 1st and 2nd avenues.
Where to go
Your procedure will be done at one of these locations:
The Presurgical Center (PSC) at Memorial Hospital on the 2nd floor
1275 York Avenue (between East 67th and East 68th Streets)
New York, NY 10065
Take the M elevator to the 2nd floor and check in at the desk in the PSC.
The Presurgical Center (PSC) at Memorial Hospital on the 6th floor
1275 York Avenue (between East 67th and East 68th Streets)
New York, NY 10065
Take the B elevator to 6th floor and check in at the desk in the PSC.
What to expect when you arrive
Many staff members will ask you to say and spell your name and birth date. This is for your safety. People with the same or similar names may be having a procedure on the same day.
When it’s time to change, you’ll get a hospital gown, robe, surgical head covering, and nonskid socks to wear.
Meet with a nurse
You’ll meet with a nurse before your procedure. Tell them the dose of any medicine you took after midnight (12 a.m.) and the time you took them. Make sure to include prescription and over-the-counter medicine, patches, and creams.
Your nurse may place an intravenous (IV) line in one of your veins, usually in your arm or hand. If your nurse does not place the IV, your anesthesiologist will do it in the operating room.
You’ll also meet with your healthcare provider or another member of your surgical team before your procedure. They’ll explain the procedure and answer your questions. They’ll also ask you to sign a consent form if you haven’t already.
Going into the operating room
You’ll either walk into the operating room or a staff member will bring you there on a stretcher. A member of the operating room team will help you onto the operating bed.
Inside the operating room
You’ll get anesthesia (medicine to make you sleep) during your procedure. After you’re asleep, your care team will place a small tube into your mouth and down your windpipe. This is to help you breathe during your procedure.
Your surgeon will do your procedure and biopsy. They will send the samples from the biopsy to a lab to be studied.
At the end of your procedure, your anesthesiologist will remove the breathing tube.
What to do after your mediastinoscopy
In the Post-Anesthesia Care Unit (PACU)
You’ll be in the PACU when you wake up after your procedure. A nurse will be keeping track of your temperature, pulse, blood pressure, and oxygen levels. You may get oxygen through a tube resting below your nose or a mask over your nose and mouth. You’ll also have compression boots on your lower legs.
Your nurse will also check the dressing around your incision. You’ll also have a chest X-ray to make sure your lung isn’t collapsed or deflated.
Your caregiver will be able to join you in the PACU, usually about 90 minutes after you arrive there.
Your nurse will bring you something to drink and eat. You’ll stay in the PACU until you’re fully awake and your healthcare provider has looked at your chest X-ray.
Once you’re ready to go home, your nurse will give you discharge instructions. They will also give you any prescriptions your healthcare provider ordered and answer any questions you have.
If your surgeon did a biopsy, your results will be ready 1 to 2 weeks after your procedure. Your healthcare provider will call you with your results or go over them with you during your follow-up appointment.
What to expect at home
After you’re discharged, schedule a follow-up appointment 1 to 2 weeks after your procedure. A nurse will call you the day after your procedure to see how you’re feeling.
You may have side effects for about 1 to 3 days after your procedure. These may include:
- Temporary tenderness or discomfort at your incision site. If you have pain, you can take acetaminophen (Tylenol) or the pain medicine your healthcare provider prescribed. If you’re allergic to acetaminophen, ask your healthcare provider what other medicine you can take.
- Hoarseness or a sore throat from the breathing tube that was used during your procedure. If your throat is sore, eat soft foods for a few days after your procedure. This includes oatmeal, mashed potatoes, and pasta.
Caring for your incision
- Keep the dressing over your incision for 24 hours (1 day). After 24 hours, you can take it off.
- You can shower 24 hours after your procedure. You can let soap and water run over the area. Remember to leave any glue or Steri-Strips in place until they start to peel at the edges. Once they start peeling, you can take them off.
- Avoid tub baths, swimming pools, and hot tubs for 10 days after your procedure.
You can go back to doing your usual activities as soon as you feel ready.
When to call your healthcare provider
Call your healthcare provider if you:
- Have trouble breathing.
- Lose your voice or it stays hoarse for 3 days or more.
- Have bleeding or redness at the incision site.
- Have a fever of 101 °F (38.3 °C) or higher.