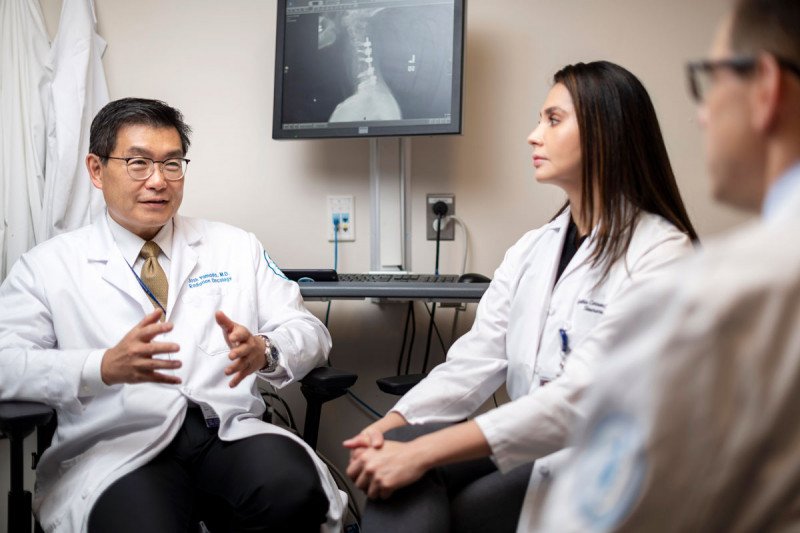
People with meningioma receive expert care from a team of specialists at Memorial Sloan Kettering, including radiation oncologist Josh Yamada and clinical nurse Cynthia Correa.
Meningioma is a typically slow-growing, noncancerous (benign) tumor that forms in the membranes that surround the brain on the inside of the skull. People with meningiomas generally have a good prognosis. But if meningioma grows back after treatment, it can become problematic, even life- threatening. People with grade I (benign) meningiomas usually have surgery and/or radiotherapy. There is a risk of the tumor coming back (recurring), particularly if it is not completely removed. Grade II (atypical) and grade III (anaplastic or malignant) tumors are more likely to recur after treatment.
Meningioma Treatment
The neurosurgeons, neuro-oncologists, and radiation oncologists at Memorial Sloan Kettering have deep experience in managing meningioma at all stages. We care for people from all over the world who have the most difficult brain tumors to treat, including meningiomas. The majority of meningiomas are noncancerous. They are either observed with MRIs or removed if they are large or growing. The main goal of treatment is to remove the tumor. If that is not possible or if the tumor is aggressive, our doctors use a combination of radiation and other treatments to slow down or stop the tumor’s growth.
Our treatment approaches include:
- MRI-guided microneurosurgery
- stereotactic radiosurgery
- image-guided radiation or re-irradiation
- proton radiotherapy
- brachytherapy
- targeted drug therapy and chemotherapy
- immunotherapy
Meningioma Experts
Geoffrey Beene Junior Faculty Chair
Attending Neurosurgeon

Assistant Attending Physician; Nicholls-Biondi Diversity Clinical Scientist Faculty Scholar
Instructor

Attending Physician

Associate Attending Physician

Attending Physician

Assistant Attending Physician

Associate Attending Physician

Vice Chair for Clinical Research, Department of Neurology; Chair, Institutional Review Board (IRB-C)

Director, Child Neurology Program

Instructor

Assistant Attending Physician

Chair, Department of Neurology; Chief, Brain Tumor Service; Evnin Family Chair in Neuro-Oncology
Attending Physician

Director, Neuro-Oncology Fellowship Program
Director, Neurology Clerkships and Sub-Internship
Assistant Attending Physician

Associate Director, Neuro-Oncology Fellowship Program

Director, Neurology Rotating Residency Program

Chair, Department of Neurosurgery; Theresa Feng Chair in Neurosurgery

Assistant Attending Physician
Co-Chief, Multi-Disciplinary Spine Tumor Service
Surgery for Meningioma
Meningioma can occur anywhere along the lining of the skull. The tumor’s location largely determines how complex the surgery will be. Tumors on top of the brain can be straightforward to remove surgically. Those at the skull base can require hours of surgery by teams of surgeons. Complicated surgeries require surgeons to work around and through the skull bones. As a result, all of a tumor may not be removed. This is especially likely if important arteries, veins, and cranial nerves are involved, or if the tumor has grown into the brain itself. These issues are more challenging for tumors that have regrown.
Surgeons who know what to expect are crucial to the success of an operation. At MSK, we use a range of sophisticated imaging techniques, including MRI. These methods allow doctors to see the tumors before surgery begins. Imaging can also be combined with a computerized view of the brain. This helps surgeons figure out how much of a tumor can be reached during a procedure, and whether there are risks to brain function. Sometimes brain mapping techniques are used. These help doctors determine how best to safely approach a meningioma, and to maximize safety if the tumor is near important parts of the brain.
MSK neurosurgeons devote themselves solely to the removal of brain tumors. We have vast experience with meningioma, both newly diagnosed and recurrent. Our care teams have access to the most advanced imaging equipment. This includes the best intraoperative navigation equipment, state-of-the-art surgical microscopes, and even an MRI scanner right in the operating room so surgeons can evaluate on the spot whether more of a tumor can be removed safely. Postoperative care at MSK, provided by our expert nursing staff, is second to none.
Sometimes the treatment of recurrent meningiomas includes brachytherapy. This involves placing radioactive sources directly in a tumor. Our surgeons work closely with MSK’s radiation oncologists to identify the people who will benefit from this treatment. Radiation oncologists and medical physicists plan the treatment in advance and come to the operating room to help the surgeons during the procedure.
Telemedicine Appointments
We know that rest is an important part of the healing process, and that travel to and from appointments can take a lot of time and energy. That’s why, for some neurosurgery visits, you may be able to see your MSK care team through our telemedicine program. If we determine that telemedicine would be appropriate for you, a member of your care team will reach out.
Telemedicine is the use of video technology to connect you with members of your MSK care team. We use secure technology to make sure all of your information stays private. You can communicate through face-to-face video conferencing via a desktop computer, laptop, or tablet device at several MSK locations. We can also use telemedicine while you or a loved one is in the hospital, either to connect you with your provider or to include someone who is not able to visit in person. During your appointment, your provider will be able to check how you’re doing, assess your follow-up needs, and discuss problems you may be having. You will be able to see and hear your MSK specialist, and they will be able to see and hear you — the only difference is that you won’t be in the same room.
A virtual visit saves you time and stress. It may also help prevent an unnecessary trip to an emergency room or urgent care center. In addition, telemedicine can help cut down on missed work days for both patients and caregivers due to travel for appointments.
Radiation for Meningioma
Radiation therapy can be used in several ways for meningioma. It may be recommended as additional therapy after surgery to prevent a tumor from growing back, depending on its location and grade. Radiation may also be used as the sole treatment for meningioma if the tumor can’t be reached through surgery. Radiation may also be used if a meningioma grows back after surgery. Occasionally, repeat radiation is given for new tumors that are in a different location than the initial meningioma, as well as to the same site of the initial tumor.
Radiation has been used to treat meningiomas for many years, but our ability to deliver radiation therapy has greatly improved. Radiation therapy is now more directed to the tumor. This precision spares nearby healthy tissue. We also have a better understanding of tumors, as well as improved radiation-planning technology. This is due to MRI and high-definition CT scans. We use imaging to verify within millimeters that the setup for each person is accurate and can be reproduced from treatment to treatment. These techniques allow for the more-precise targeting and delivery of radiation, leading to improved results.
The most common schedule for radiation therapy is five to six weeks of low-dose radiation treatment. This is well tolerated by most people and is less likely to harm nearby healthy tissue than larger, individual doses of radiation.
Recurrent or regrowing meningioma may need repeat radiation therapy. This requires special expertise and an understanding of the potential long-term effects. Repeat radiation therapy is sometimes given as a daily low dose over five to six weeks. It may instead be a shorter but more intense course of radiation therapy. Brachytherapy may be used as well.
The most common form of radiation delivery is external-beam radiation. This involves delivering radiation from a machine called a linear accelerator that creates radiation similar to what is used in an X-ray. External-beam radiation can be used very precisely in a treatment called intensity-modulated radiation therapy.
On occasion, we also use proton therapy. This type of external-beam radiation is most frequently used for a meningioma that is deep in the brain. At times it is used for treating a tumor that has grown back.
All of these options require the input of an experienced, multidisciplinary staff. Our meningioma care teams include radiation oncologists, neurosurgeons, neuroradiologists, neuropathologists, neuro-oncologists, and medical physicists. We meet regularly to review and discuss the best treatment for each person we care for.
Drug Therapy for Meningioma
Despite surgery and radiation, a small number of meningiomas may grow back. These require chemotherapy or another treatment. At MSK, our team is investigating new ways to deliver these therapies to patients. We sequence the genomes of individual meningioma tumors to determine the molecular makeup of the tumors. Our goal is to create a personalized care plan based on each individual tumor and patient situation. This may include traditional chemotherapy, molecularly targeted therapy, immunotherapy, or participation in a clinical trial.
For a list of available clinical trials for meningioma, visit our clinical trial finder.
New Patient Appointments
Available Monday to Friday, 8:00 a.m. to 6:00 p.m. (Eastern time)
