Larry’s Story
One morning, Larry noticed a tiny, painless bump on his neck. At the insistence of his dermatologist, he underwent a neck CT scan that revealed stage IV throat cancer. An ESPN sportscaster, Larry was fearful that treatment would damage his voice. Memorial Sloan Kettering’s head and neck cancer team offered him a combination chemotherapy-radiation approach to preserve his voice while eliminating the cancer.
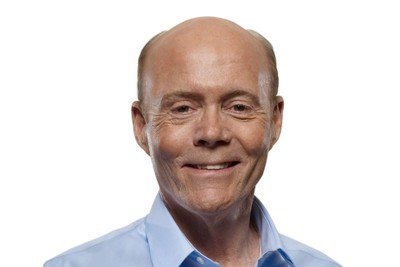
Larry Rawson
One morning in early 2005, I felt a painless lump while running my fingers down my neck after shaving. The little lump could only be felt when I pressed the skin into my neck. I’d had a harmless cyst on my back for years, so I figured it was something similar. I showed it to my internist and he told me it was nothing.
The lump was still there six months later when I had a routine appointment with my dermatologist. She calmly but firmly urged me to have it biopsied. She said, “I’ll make the appointment for you, and promise me that you’ll go.”
Around the same time, I began to feel something in my throat, like a little flap of skin. I didn’t feel it all the time, just a few times a day when swallowing, and it never hurt in any way.
I kept my promise and went for the needle biopsy. During the biopsy, I mentioned the flap of skin in my throat to the doctor and he decided to send me for a CT scan of my neck. He then referred me to a head and neck specialist and told me to follow up with him for the CT results. Several days later, the doctor who performed the biopsy called me and said that the results were negative — no cancer.
A week later, at my appointment to discuss the CT results, the head and neck specialist drew a circle on a piece of paper, colored in the area from 9 to 12 o’clock, and said, “Your cancer is here.” I was totally shocked. This wasn’t what I was expecting — I had been told the biopsy was negative. Now I was being told I had throat cancer.
The CT scan showed that I had squamous cell cancer at the base of my tongue and the cancer had spread to two areas of my lymph nodes. He called it a stage IV cancer. That scared me. He told me that my voice would probably be raspy for the rest of my life and that I would always have dry mouth because the radiation treatments would kill my salivary glands.
As a professional broadcaster who covers track-and-field events and major marathons for ESPN, I could see a career I loved possibly coming to an abrupt halt.
Getting a Second Opinion
My wife and I decided that I should definitely get a second opinion. While I was evaluating my options that evening, a cousin of mine, himself a medical doctor, heard from my sister of my plight and called me. He encouraged me to consider Memorial Sloan Kettering because he thought it was the best place to be treated. Aware of Sloan Kettering’s terrific reputation, I quickly agreed.
In researching my diagnosis, I read that treatment for this type of cancer could be disfiguring and could seriously harm my ability to speak, hear, and swallow. When I met with Dr. Dennis Kraus, a head and neck surgical oncologist at Sloan Kettering, he couldn’t promise what my outcome would be, but he did tell me that success rates can be dramatically different, depending on where a patient is treated. More experience in treating a particular type of cancer can lead to better outcomes, and I was comforted to know that Sloan Kettering is one of the most experienced hospitals in the nation for treating throat cancer.
Planning Treatment
My wife and I were very impressed by the level of detail and care that went into planning my treatment. A team of experts in specialties including dentistry, swallowing, and hearing worked together, which made me feel very confident that I’d be getting the right care. Dr. Kraus performed another biopsy to confirm the diagnosis. Then the team recommended that the best way to save my voice while getting rid of the cancer was with chemotherapy and radiation together, not surgery. Medical oncologist David Pfister took over my care.
Dennis Kraus, MD — Surgical Oncologist: Larry came to see me after he had been diagnosed by another physician who recommended surgery to treat his throat cancer. I re-biopsied the base of his tongue and determined that he had a moderately advanced squamous cell tumor in the back of his tongue that had spread to his neck.
About a decade ago, we would have operated on a base-of-tongue cancer. However, the surgery was often physically disabling and could have a pretty significant impact on the patient’s quality of life, namely on speech and swallowing. So more than ten years ago, we changed the way we approach these cancers. When possible, we avoid surgery and treat only with chemotherapy and radiation, the same way we treat larynx or voice-box cancer. That was the approach I recommended for Larry, so I sent him across the hall to see my colleague David Pfister, the Chief of Head and Neck Service for medical oncology here at Memorial Sloan Kettering.
David Pfister, MD — Medical Oncologist: In the United States, head and neck cancers only account for about 6 percent of all cancers diagnosed. And oropharyngeal cancer is a small subset of that. Since it is relatively uncommon, most community medical oncologists will have limited experience treating the disease.
Our extensive experience with head and neck cancers is a big advantage to being treated here. It puts us in a position to know the best therapies to use to cure a patient’s cancer, what symptom management strategies are most effective, how to modify treatments appropriately when something unexpected happens, and how to best combine the different parts of treatment to ensure the best possible outcomes. In addition, treating head and neck cancers involves concerns about quality of life, appearance and self-image, and functions such as vision, smell, hearing, speech, and swallowing, which all need to be considered when therapy is being planned.
One of the keys to our success here at Sloan Kettering is our multidisciplinary team approach. Oftentimes when patients see our surgeons, they’ll hear, “I don’t think surgery is the best way to go. I think another approach will be better.” As a disease management team, we have an integrated way to prioritize the possible therapies, and together we determine what we think is best for the patient.
We develop a comprehensive treatment plan for each patient that includes all aspects of their care. The surgeon, medical oncologist, radiation oncologist, and other specialists are all part of the treatment planning process. And since we work closely together in the same location, I often walk down the hall to discuss a patient’s progress with their surgeon or radiation oncologist. That allows us all to stay very well informed about our patients’ progress.
Saving a Voice
Larry: Knowing that I was a professional sportscaster, my doctors were very focused on saving my voice. Memorial Sloan Kettering audiologists conducted a complete hearing test before the start of chemotherapy, because some chemotherapy can damage hearing. I didn’t realize that I already had some minor hearing loss. Based on that information, Dr. Pfister decided to use the chemo drug that would be least likely to cause a further hearing problem. I’m very grateful for the attention they paid to preserving my speech and hearing.
Dr. Pfister: Larry’s baseline hearing test showed that he had some hearing loss, which at its current level did not affect his quality of life, but could if it got worse. In addition to curing a patient’s disease, we also strive to achieve the best possible functional outcome. In Larry’s case, knowing his occupation as a sportscaster, hearing and communication outcomes were of obvious importance. So, we looked carefully at the possible side effects of the chemotherapy options available to treat Larry’s cancer.
The drug that has been the cornerstone of throat cancer therapy is cisplatin, but it has been known to sometimes negatively affect hearing. So for Larry, we chose a combination of carboplatin and 5-fluorouracil, which we know is effective, but we felt posed less risk to his hearing than cisplatin.
Receiving Chemotherapy and Radiation
Larry: I never missed a day of work throughout the two months of chemotherapy and radiation therapy! During that time, I received three rounds of chemotherapy with a couple of weeks off in between. Each round involved a four-day continuous infusion of chemotherapy into my body. A portable pump sent the drugs through an access port, which had been implanted in my chest. The port sent the chemo into a vein, which went directly to my heart and then was pumped throughout my body.
Having the pump meant that I didn’t have to stay in the hospital to receive my treatment. I live near the hospital, and walked there five days a week for radiation treatments and, on certain days, a dose of another chemotherapy drug given through the port. Although I was occasionally tired from the treatments, I could still function pretty well, despite many issues that were going on.
Dr. Pfister: Larry was able to receive all of his therapy as an outpatient. He came to the hospital every day, Monday through Friday, for radiation. He also received 5-fluorouracil (5-FU), which was given over four days, once every three weeks, as well as a short intravenous carboplatin infusion on each of the four days he received the 5-FU.
5-FU is given as a continuous infusion, but we gave him a pump so that he could get it at home rather than staying in the hospital overnight. For patients who are otherwise healthy and who live nearby, this works well and is typically our recommendation. When patients aren’t as strong or we have concerns regarding their ability to safely receive their planned chemotherapy as outpatients, we may revise the treatment plan or recommend treatment as an inpatient.
The radiation is given over six to seven weeks. The chemotherapy is dispensed during the first week of radiation, in the middle, and at the end. Patients generally get the last dose of chemotherapy right when they’re ending their radiation treatments.
Nancy Lee, MD — Radiation Oncologist: Here at Sloan Kettering, we use an extremely precise, three-dimensional method of delivering radiation called intensity-modulated radiation therapy (IMRT). Using this technique, the radiation oncologist can “mold” the dose of radiation to the tumor. This makes it possible to use higher, more effective doses, while sparing healthy tissues and reducing the side effects.
These new approaches can often preserve patients’ ability to speak and swallow normally. Giving chemotherapy and radiation at the same time is effective in head and neck cancers because the chemotherapy drugs make the radiation work better than giving radiation alone.
Coping with Side Effects
Larry: My throat became very sore from the radiation treatments. I couldn’t eat at all for almost three months. Because this is a problem that often occurs during treatment for throat cancer, a feeding tube was inserted into my stomach, and I gave myself liquid nutrition through the tube during this time.
My chief difficulty during treatment was gagging from the very thick phlegm caused by the radiation. I carried a towel with me day and night to spit into. Lisa, one of my nurses, warned me that this would happen, but that it would eventually subside. Lisa and Nicole, the nurses in Dr. Pfister’s practice, were extremely knowledgeable and helpful throughout my treatment.
Other side effects of the chemo and radiation included a 20-pound weight loss, heavy perspiring at night, interrupted sleep, and dry mouth from the trauma to my salivary glands.
Dr. Pfister: As he went through his treatment, Larry had several of the typical side effects we often see. The treatment can lead to inflammation in the throat, excess phlegm, difficulty swallowing, and throat pain.
Because he had difficulty swallowing during treatment, Larry had a percutaneous endoscopic gastrostomy (PEG), or feeding tube, implanted in his abdomen to deliver food directly into his stomach. This measure is usually temporary, and may be needed during chemotherapy and radiation therapy because some patients have trouble eating. It’s important that cancer patients maintain their strength by getting proper nutrition and hydration. The feeding tube also helps patients get their treatment as an outpatient.
Swallowing is a major concern with head and neck cancer patients because if their throat hurts, some patients don’t try to swallow at all, and they get atrophy in the muscles of their throat. Through working on a regular basis with the specialists at the Speech and Swallowing Center, we get our patients swallowing as early as we can. It’s enormously important in terms of achieving a good outcome and for getting them back to their normal activities.
They “got it.”
Larry: Towards the end of my treatment, my medical team started to share with me their positive prognosis. My chemo was not yet finished when Dr. Pfister told me that it already looked like they “got it” — that the cancer was gone.
I am delighted to say that I have been cancer-free since the fall of 2005. My treatment ended less than one week before the 2005 New York City Marathon — and I was able to announce the race for ESPN, as I did for the many marathons I had broadcast in previous years. I had to hit the “cough” button occasionally to turn off my microphone so I could get the phlegm up, but I was still able to announce the entire race. At the end of the show, my co-host, Al Trautwig, presented me with a medal for my own endurance and courage. It was an emotional and moving moment for me.
Dr. Pfister: Larry is a prime example of the benefit of combination therapy to preserve form and function in head and neck cancer patients. When chemotherapy and radiation are used to treat throat cancer, the functional outcomes can vary. Some people’s voices are completely unchanged, while others experience some impact. In Larry’s case, the treatment worked remarkably well.
I often tell patients, “Don’t set yourself up for failure. When you go back to work, you may not be at 100 percent right away.” But Larry was intent on broadcasting the marathon. Although he was at the peak of his side effects, he announced the race five days after his last treatment. And he did an incredibly good job. For what he had been through, it was really remarkable.
Today, when we see Larry for follow-up visits, it’s to make sure he has not developed any suspicious symptoms, to do office endoscopies where we make sure the base of the tongue looks okay, as well as to feel his neck. Scans are not routine with each visit, but we do obtain scans after completing treatment to make sure there is no evidence of cancer and to have as a new baseline for future comparisons, if necessary. As he gets further out from treatment without any signs of trouble, the frequency of his visits will decrease.
I sound just like I did before.
My voice has healed very well and sounds exactly like it did before I had cancer. I can even hit the high falsetto notes when I sing in the shower. During my treatment, that had become impossible to do. And I have no swallowing complications, thanks to the expert therapists at the Swallowing Center at Sloan Kettering.
Before I started treatment, my radiologist told me that they were going to try to save some of my salivary glands, but it was possible that I could have dry mouth for the rest of my life. Thanks to the pinpoint radiation treatment that I received, about 65 percent of my salivary glands continue to function, and thus I have a far more normal life than I might have. I am so appreciative of that.
Having a positive attitude has always been a part of who I am. Set your goals, and go achieve them. That approach certainly helped me to get through my cancer treatment. It’s how I became a national caliber distance runner in my youth, and led my men as a Marine lieutenant in Vietnam.
But, obviously, I could not have done this alone. In addition to Dr. Pfister, Dr. Kraus, Dr. Narayana (my radiation oncologist who has since left Sloan Kettering), and Dr. Lee, my friends, family, and the track-and-field world were all so supportive throughout this ordeal and were beacons of strength for me. The woman who was invaluable to this whole process, my wonderful wife, Laura, could not have been more supportive. She was terrific.
I don’t take my continued good health for granted. I go to Sloan Kettering every three months for evaluation. It’s always a joy to see the doctors and nurses who took such good care of me. I will forever appreciate their dedication and excellence, which helped give me a brand new lease on life.