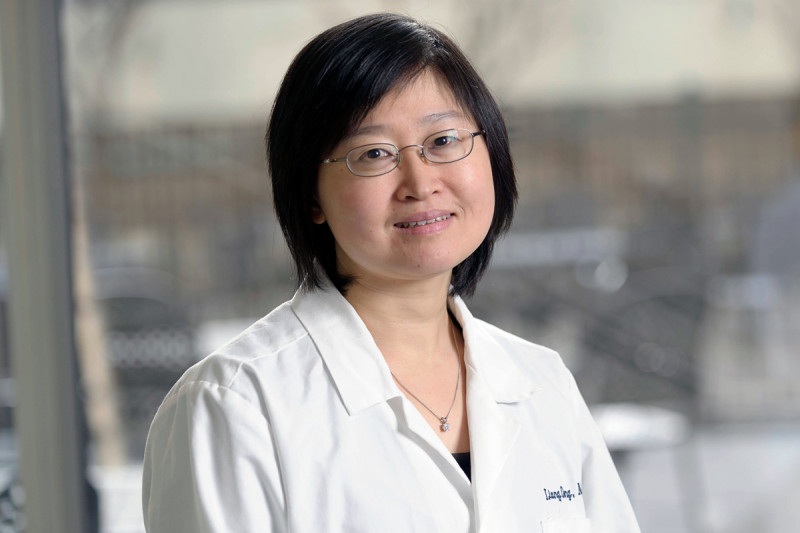
Physician-scientist Liang Deng studies poxvirus interface with the immune system and the development of poxviruses as oncolytic and immunotherapy for cancers. We spoke to her in 2013.
When physician-scientist Liang Deng joined the Memorial Sloan Kettering faculty in 2004, it marked a homecoming, as she returned to the institution and the research specialty — poxviruses — that began shaping her career a decade earlier.
Now a physician on the Dermatology Service and head of a Memorial Hospital research laboratory, she pursues her twin passions of caring for patients with skin cancers and investigating poxviruses, which cause human and veterinary diseases but also offer great therapeutic potential.
“It’s very gratifying to help patients fight their skin cancers, while at the same time seeking better therapies,” Dr. Deng says. “And research into poxviruses offers the potential to harness the power of the immune system to fight deadly skin cancers such as melanoma.”
Dr. Deng grew up in China and studied biology at Fudan University, in Shanghai, before receiving her undergraduate degree from the University of Rochester, in New York. She then moved to Weill Cornell Graduate School of Medical Sciences to pursue a PhD degree. As part of that work, she studied poxviruses in the laboratory of Sloan Kettering Institute molecular biologist Stewart Shuman.
The most well-known poxvirus is vaccinia, which has been used in vaccines to eradicate smallpox. Under Dr. Shuman’s guidance, Dr. Deng used vaccinia as a model system to study transcription, the process by which genetic information is converted from DNA to RNA. Upon completing her graduate work, she transitioned immediately to medical training at Weill Cornell Medical College.
During medical school and dermatology residency (receiving some training in skin oncology at Memorial Sloan Kettering under the guidance of Dermatology Service Chief Allan C. Halpern, physician Patricia L. Myskowski and others), Dr. Deng developed an interest in cutaneous immunity — the skin’s response to pathogens and allergens — and became curious about a subset of skin immune cells called epidermal dendritic cells and their role in infection and inflammation. After her medical training, Dr. Deng returned to Memorial Sloan Kettering to combine patient care with research on the interface of dendritic cells and the poxviruses that first sparked her interest.
“Poxviruses are some of the most complex viruses known, and they are well suited to being modified for therapeutic use,” Dr. Deng explains. “It is easy to insert foreign genes coding for cancer antigens or immune-stimulating molecules into the viral genome. The poxvirus then can be used as a vector (a delivery system) to express these foreign proteins in immune cells, prompting an immune reaction against a specific target. In addition, poxviruses readily infect cancer cells, allowing them to be used to destroy these cells directly.”
Research from her laboratory, in collaboration with Dr. Shuman, cancer immunologist Alan Houghton, and immunologists Taha Merghoub and James Young, has identified several viral-sensing pathways by which immune cells detect poxviruses. Intriguingly, they also have discovered that poxviruses produce proteins that act as viral antagonists, allowing the virus to evade an immune attack from the host.
“We found that wild-type (natural) vaccinia actually suppresses the immune responses of infected dendritic cells,” she says. “By contrast, a weakened form of the virus called modified vaccinia virus Ankara (MVA) has a stimulating effect on dendritic cells.” MVA is now a leading vector in vaccines being tested against infectious agents and cancers.
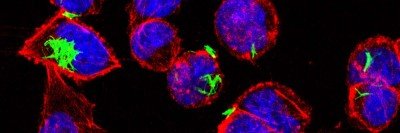
In collaboration with cell biologist Xuejun Jiang’s laboratory, Dr. Deng’s team has also been investigating how poxviruses affect autophagy — a process in which a cell under stress breaks down its own components to recycle them for energy or to destroy the infectious agent. “It is fascinating that wild-type vaccinia inhibits autophagy, whereas MVA induces it,” she says.
In addition, Dr. Deng collaborates with medical oncologist Jedd D. Wolchok and his team to explore using poxviruses as oncolytic viruses. In this approach, the poxvirus is injected directly into tumors, causing cancer cell death. The destroyed cells release proteins called tumor antigens, which are presented by dendritic cells to other immune cells to induce immunity against cancer.
“I hope in the next five years, we’ll be able to incorporate oncolytic therapies into melanoma treatments,” she says. “But combination therapy will probably be necessary to enhance their efficacy.”
She and Dr. Wolchok’s laboratory have preliminary results suggesting tumors can be destroyed more effectively by combining oncolytic therapies with a drug called ipilimumab, which removes a natural brake from the immune system and is already approved for use against advanced melanoma.