Common Names
- MLT
- Pineal hormone
For Patients & Caregivers
Tell your healthcare providers about any dietary supplements you’re taking, such as herbs, vitamins, minerals, and natural or home remedies. This will help them manage your care and keep you safe.
Melatonin is a hormone your body makes to grow and develop. It also controls your cycle of being asleep and awake. Small amounts of melatonin are found in fruits, nuts, olive oil, and wine.
You can also take it as a supplement to help you sleep.
Melatonin is used to:
- Treat insomnia (trouble sleeping)
- Treat seasonal affective disorder (SAD)
- Treat migraines
- Treat insomnia in children with autism spectrum disorder
Melatonin also has other uses that haven’t been studied by doctors to see if they work.
Talk with your healthcare provider before taking melatonin supplements. They can interact with some medications and affect how they work.
For more information, read the “What else do I need to know?” section below.
Side effects of using melatonin may include:
- Headaches
- Drowsiness
- Changes in sleep patterns
- Trouble sleeping
- Bad dreams
- Confusion or altered mental state
- Fast heart rate
- Flushing or getting red in the face
- Itching
- Stomach cramps
- Low body temperature
- Avoid melatonin if you’re driving or operating heavy machinery until you’re familiar with how it affects you. It can cause drowsiness.
- Talk with your healthcare provider if you have hormone-sensitive cancer like breast or prostate cancer. Melatonin can change the amount of estrogen in your body. This may worsen your condition.
- Talk with your healthcare provider if you’re taking nifedipine (Procardia®). Using melatonin at the same time can increase your blood pressure and heart rate.
- Talk to your healthcare provider if you’re taking blood thinners such as warfarin (Jantoven® or Coumadin®). Melatonin may increase your risk of bleeding.
- Talk with your pediatrician before giving your child melatonin. Taking too much melatonin can cause serious side effects in children under age 3, including trouble breathing and death.
- Keep your melatonin in a safe place (such as in a locked cabinet) and out of children’s reach.
For Healthcare Professionals
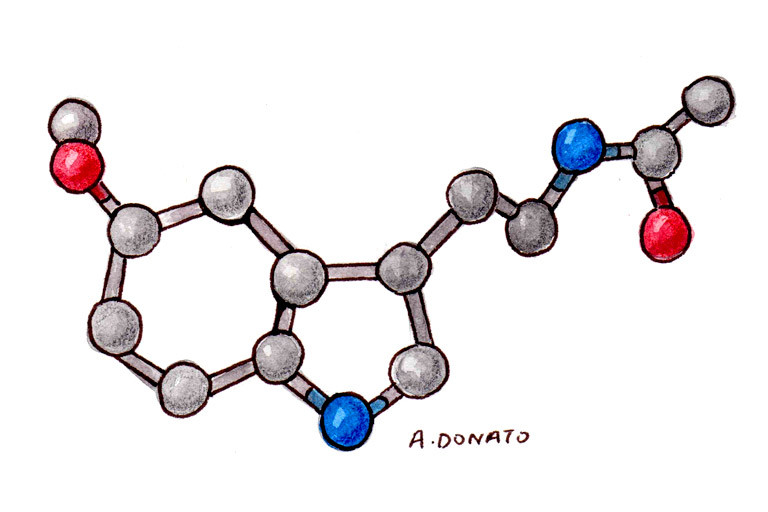
Melatonin is produced endogenously in humans by the pineal gland. Although the exact mechanism of action is unknown, it is thought to control the circadian pacemaker and promote sleep (1). Small amounts of melatonin are found in fruits, nuts, olive oil, and wine. The supplemental form is used as a sleep-aid.
Melatonin may decrease sleep latency and improve sleep duration (2) (3) (4), although randomized trials have produced mixed data (27) (28) (29). Meta analyses did not find any significant effects with melatonin on insomnia disorder (75), secondary sleep disorders associated with medical, neurological, or substance abuse disorders (5), or on sleep quality in menopausal women (71), but supplementation improved subjective sleep quality in patients with traumatic brain injury (44) and Parkinson’s disease (76), and cognitive outcomes in patients with Alzheimer’s disease (72). Melatonin may also benefit those with jet lag (51) (52).
Melatonin was shown to decrease surgery-associated anxiety and pain (6), frequency of migraine attacks (7) and perioperative anxiety (30) (56), but there is insufficient evidence for its use to improve delirium in hospitalized patients (57), to improve depression or depressive symptoms (47), or for seasonal affective disorder (SAD) (48). Studies in patients with nocturia (53) (77) and those in ICU produced mixed results (46) (64). Whether it can help in benzodiazepine withdrawal is also unclear (49) (50).
Data suggest benefits of child-appropriate, prolonged-release melatonin for long-term treatment in children and adolescents with autism spectrum disorder and insomnia (59). The American Academy of Neurology guidelines recommend using melatonin, starting with a low-dose, for children and adolescents with autism spectrum disorder and sleep disturbance if behavioral strategies have not been helpful, and if contributing coexisting conditions and use of concomitant medications have been addressed (60).
Clinical trials evaluating melatonin as a monotherapy or in combination with other agents, and in patients with solid tumors reported improvements in fatigue (68) (78), and quality of life and survival time (10) (11) (12) (13) but conflicting data suggest no benefits (79) (80). Melatonin also did not improve appetite, weight, or quality of life in cancer patients with cachexia (35). In studies of postmenopausal breast cancer survivors, short-term supplementation did not influence estradiol levels (36) but improved sleep quality (37). Data also suggest melatonin may help reduce incidence of chemotherapy side effects including thrombocytopenia, asthenia, and neurotoxicity (54); improve cognitive function, sleep quality and depressive symptoms (61); minimize radiotherapy-induced reduction in blood cell counts (58); protect against radiation-induced genotoxicity (62)and dermatitis (81); and reduce the incidence of oral mucositis caused by chemo- and radiotherapy (69). In addition, melatonin was found comparable to zolpidem in affecting sleep duration, latency, efficiency, and disturbance in colorectal cancer patients undergoing chemotherapy (65). But in survivors of childhood cancers, there were no effects on sleep or neurocognitive performance (70).
According to a case report, oral melatonin may delay menopause in pre-menopausal women by modulating levels of follicle stimulating hormone (FSH) and estrogen (31).
Small amounts of melatonin are found in fruits, nuts, olive oil and wine.
- Insomnia
- Seasonal affective disorder
- Migraines
- Insomnia in children with Autism Spectrum Disorder
Melatonin is an endogenously produced indolamine hormone secreted by the pineal gland in humans. Nocturnal secretion is regulated by circadian rhythms and nighttime darkness (17), and melatonin is thought to control the circadian pacemaker and promote sleep. Ironically, it is associated with wakefulness and activity in nocturnal animals (14). As levels of melatonin increase, an associated drop in core body temperature occurs. Both elderly and depressed patients tend to have lower basal levels of melatonin (2).
Melatonin is a free-radical scavenger (18) (38) and enhances antioxidative enzyme activities (39), interacting with cytosolic calmodulin and stimulating IL-4 production in bone marrow T-lymphocytes (1). In vitro and animal studies suggest that antitumor effects may occur through antimitotic or immunomodulatory activity. In vitro studies demonstrate antiproliferative effects on human breast cancer (HS578T) (19) and mouse melanoma (B16BL6, PG19) (8). Decreases in breast cancer metastasis may occur via modulation of Rho-associated kinase protein-1 expression (41). Melatonin reduces proliferation of PC-3 and LNCaP cells in mice, but has no effect on apoptosis (9). Its effect on tumor cell growth may be mediated in part by melatonin receptor signaling (20) (21). In endometrial cancer cells, it interferes with estrogen receptor expression (22). Other laboratory studies suggest that melatonin behaves both as a selective estrogen receptor modulator (SERM) and as an aromatase inhibitor (42) (43). In a murine model, it modulated expression of genes crucial for DNA repair — Ogg1, Apex1, and Xrcc1 — in peripheral blood cells, to reduce X-ray-induced DNA damage (45).
- Melatonin may cause drowsiness and should not be taken when driving or operating heavy machinery.
- Drowsiness, alterations in sleep patterns, altered mental status, disorientation, tachycardia, flushing, pruritus, abdominal cramps, headaches, trouble sleeping, bad dreams, hypothermia (1) (2) (14) (15) (36)
- Hypothermia in autism with sleep disorder: In a 3-year-old girl whose body temperature dropped to 34°C following a single dose of melatonin. Supplementation was stopped, but hypothermia continued for 2 more days after which her temperature returned to normal value (63).
- Exacerbation of myasthenia gravis: In 3 patients following melatonin use, likely due to an upregulation of the adaptive immune system and an interaction with corticosteroids and other immunosuppressives (66).
-
Facial swelling and erythema: In a 66-year-old man, with a history of baseline postoperative facial lymphedema following head and neck surgery and radiotherapy for desmoplastic melanoma, with melatonin use. His symptoms resolved after stopping supplementation (67).
Pediatric Cases — Hospitalizations, severe outcomes and fatalities - Between January 1, 2012-December 31, 2021, 260,435 pediatric cases of melatonin ingestion were reported to the Poison Control Centers’ National Poison Data System (NPDS). Melatonin ingestion cases also accounted for 4.9% of all pediatric ingestions reported in 2021 compared with 0.6% in 2012. Five children required mechanical ventilation, and two died (73).
- Seven deaths of infants and toddlers, aged 2 months to 3 years. Although the cause and manner of deaths were reported as undetermined, exogenous melatonin was detected following toxicological analysis with concentrations ranging from 3-1400 ng/mL in whole blood (74).
- Bleeding episodes in an 18-month-old associated with the mother’s use of valerian and melatonin supplements. The bleeding ceased after discontinuing melatonin (82).
Nifedipine: Concomitant administration of melatonin and nifedipine has resulted in elevations in blood pressure and heart rate (16).
CYP1A2 substrates: Melatonin inhibits CYP1A2 and may increase the bioavailability of substrate drugs, like fluvoxamine (23) (26) (34).
Anticoagulants: Oral melatonin intake is associated with lower plasma levels of factor VIII and fibrinogen (25). Therefore, this may increase the risk of adverse effects when used with anticoagulant medications.
Rhubarb: A study using human primary hepatocytes showed that concomitant use can cause metabolic disorder of melatonin (55).
May lower plasma levels of factor VIII and fibrinogen (25).