This information describes swallowing problems that can be caused by radiation therapy to your head and neck. It also describes how to prevent them.
About normal swallowing
Many muscles and nerves work together to help you swallow (see Figure 1).
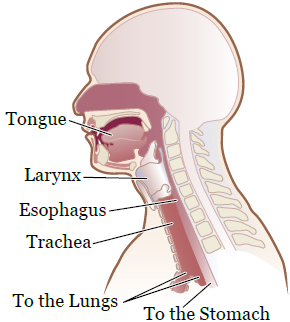
When you eat and drink, foods and liquids mix with your saliva. Your saliva makes the food soft and moist. Chewing your food breaks it down. As you chew, the food and saliva form a ball called a bolus.
When you swallow, your tongue pushes the bolus to the back of your mouth. Then, a reflex takes over and the back of your tongue pushes the food into your esophagus (food pipe).
At the same time, your larynx (voice box) closes to keep the food from entering your trachea (airway). The bolus then moves down your esophagus and into your stomach.
Sometimes, food or liquid can stick in your esophagus or enter your airway or lungs. This happens if the muscles in your mouth or throat are weak, or not working like they should. Both of these things can harm you.
When food or liquid enters your airway or lungs, it’s called aspiration (AS-pih-RAY-shun). Aspiration can lead to health problems, such as:
- Pneumonia (noo-MOH-nyuh). This is an infection in 1 or both of your lungs.
- Respiratory infections. These infections affect your nose, throat, airways, or all 3.
How cancer and radiation therapy can affect swallowing
Radiation therapy can weaken the muscles and structures that help you swallow. Whether this happens to you depends on your tumor’s size and location. It can also keep the muscles and structures from working as well as they did before you started radiation therapy. This can make it harder to eat and drink normally.
Radiation therapy can cause:
- Pain when swallowing
- Mucositis (myoo-koh-SY-tis), which are painful areas or sores in your mouth or throat
- Dry mouth
- Thicker saliva
- Swelling in your mouth, throat, or both
- Taste changes
These symptoms usually start 1 to 2 weeks after you start radiation therapy. They may get worse during treatment. Most symptoms will start to get better about 2 to 4 weeks after your treatment ends.
Radiation therapy can also cause fibrosis (fy-BROH-sis). This is tissue scarring that’s permanent (does not go away). The effects of this scarring depend on the area that was treated. Some effects of scarring are:
- Trismus. This is a condition that causes your jaw muscles to become tight. This tightening can make it hard to open your mouth and chew your food.
- Your salivary glands may not make enough saliva. This can make it hard to swallow because your mouth is too dry.
- The muscles in your tongue and the back of your throat may not be able to move as well. This can make it harder to push foods or liquids down your throat and open your esophagus.
- The muscles that help protect your airway when you swallow may get weaker. They may not be strong enough to keep foods or liquids from going down your airway.
- Your esophagus may narrow. This can cause food to get stuck in the back of your throat.
Not everyone will have all these problems. We plan your treatment so there’s less of a chance these problems will happen. Your care team will also teach you things you can do to help prevent and manage these problems.
Other treatments can also affect swallowing. Surgery can affect parts of your mouth and throat, which could make swallowing harder. Some chemotherapy medicines can cause sores in your mouth and throat. This can make swallowing painful.
Managing problems with swallowing
Having trouble swallowing is called dysphagia (dis-FAY-jee-uh). Your care team will work with you to help you manage dysphagia. This team includes your doctors, nurses, a swallowing specialist, and a clinical dietitian nutritionist.
You will see a swallowing specialist before, during, and after your treatment. They will:
- Explain how treatment can affect your swallowing.
- Teach you exercises to stretch your swallowing muscles and keep them strong.
- Look for any changes in your ability to swallow as you go through radiation therapy.
- Help guide you on what is best and safe to eat and drink during and after radiation therapy.
- Help you keep your ability to swallow after your treatment is done. This can prevent changes that are long-term (last a long time) or late-onset (happen a long time after treatment).
Painful swallowing
If it’s painful when you swallow, your care team will give you pain medicine to help. Follow your doctor’s instructions for taking the medicine. If it does not help, tell your doctor or nurse. There are many different medicines that can be used to help manage your pain.
Aspiration
When you’re having trouble swallowing, food or liquid can pool (get stuck) in the back of your throat. This can make you more likely to aspirate your food. Signs of aspiration are:
- Coughing when you swallow
- Coughing after you swallow
- Changes in your voice while you’re eating or drinking
If any of these things happen, contact your swallowing specialist right away. They will check to see if there are any changes in your ability to swallow. If there are, they will recommend foods and liquids that are safe and easy to swallow. They can also practice swallowing exercises with you to help prevent more changes in your ability to swallow.
Call your doctor or nurse right away if you have any of these symptoms:
- Shortness of breath
- Wheezing (a whistling or squeaking sound when you breathe)
- Pain when breathing
- A cough with phlegm (pronounced like flem) or mucus
- A fever of 100.4 °F (38 °C) or higher
These things can be signs of pneumonia or a respiratory infection.
Trismus
Trismus is when you cannot open your mouth as wide as usual. Trismus can happen anytime during, right after, or even years after your treatment.
When you cannot open your mouth well, it’s hard for your doctor to look at the area. You may also have problems with:
- Oral hygiene (cleaning your mouth and teeth). This can lead to bad breath, cavities, and infections.
- Chewing and swallowing. This can make it hard to eat and drink.
- Talking.
- Kissing.
- Having a breathing tube placed, such as if you ever need general anesthesia. This is medicine to make you sleep during a surgery or procedure.
- Having routine dental treatment.
Once trismus develops, it’s very hard to treat. That’s why it’s important to prevent trismus and treat it as early as you can. Your swallowing specialist will teach you exercises to help prevent trismus. It is also important to keep good oral hygiene and good posture.
Exercises
These exercises will help prevent changes in your ability to swallow during your radiation therapy. They will also help you keep your ability to swallow over time. Your swallowing specialist will tell you which exercises are best for you and when to start them. The exercises will not be helpful if you:
- Start them too soon after surgery.
- Start them too soon before your radiation therapy.
If you need to swallow for an exercise, use only your saliva, if you can. If you need to take small sips of water to help you, that’s OK.
Do each exercise 3 times a day. Repeat each exercise 10 times before moving on to the next one. Your swallowing specialist may tell you to do them more or less often. Follow your swallowing specialist’s instructions.
Swallowing exercises
Tongue hold exercise (Masako exercise)
- Put the tip of your tongue between your front teeth.
- Swallow. Keep the tip of your tongue between your front teeth while you swallow.
You can relax and move your tongue back to its normal position between each swallow.
Effortful swallow exercise
- Swallow normally, but squeeze hard with your throat and tongue muscles.
To help squeeze hard, pretend you’re swallowing something big (such as a spoonful of peanut butter).
Mendelsohn swallow maneuver exercise
- Start to swallow normally. When you feel your throat and Adam’s apple move up or squeeze, pause for 2 seconds. Then, let your throat relax.
To pause during the swallow, pretend you’re holding your breath in the middle of the swallow for 2 seconds. Then, let your throat relax. It may also help to place your hand lightly on your throat. This helps you feel when the muscles are moving up or tightening during the swallow.
Supraglottic (SOO-pruh-GLAH-tik) swallow exercise
- Breathe in (inhale) and hold your breath.
- While holding your breath, swallow.
- Breathe out (exhale) forcefully or cough out the breath you were holding.
Tongue range of motion (ROM) exercises
Tongue protrusion exercise
- Stick out your tongue as far as you can, until you feel a good stretch.
- Hold it there for 5 seconds.
Tongue retraction exercise
- Pull your tongue far back in your mouth, as if you’re gargling or yawning.
- Hold it there for 5 seconds.
Tongue lateralization exercise
- Move your tongue to the left as far as you can, until feel a good stretch.
- Hold it there for 5 seconds.
- Move your tongue to the right as far as you can, until you feel a good stretch.
- Hold it there for 5 seconds.
Tongue tip exercise
- Place the tip of your tongue behind your top teeth or on your gums.
- While holding this position, open your mouth as wide as you can for 5 seconds.
Back tongue exercise
- Say a strong “k” or “kuh” sound. Do this by pulling the back of your tongue to the back of your throat.
Tongue resistance exercises
Your swallow specialist will tell you if you need to do these exercises and when to do them. You will need a tongue depressor for these exercises. This is a thin piece of wood that looks like a popsicle stick.
- Hold the tongue depressor steady over the middle of your tongue. Push up with your whole tongue for 5 seconds.
- Hold the tongue depressor right in front of your tongue. Push the tip of your tongue against the tongue depressor for 5 seconds.
- Place the tongue depressor on the left side of your tongue. Push your tongue against the tongue depressor for 5 seconds. Try not to turn the tip of your tongue.
- Place tongue depressor on the right side of your tongue. Push your tongue against the tongue depressor for 5 seconds. Try not to turn the tip of your tongue.
Jaw exercises
Active range of motion and stretching exercises
You can do these exercises while sitting or standing. Hold your head still while doing these exercises.
- Open your mouth as wide as you can, until you can feel a gentle stretch but no pain (see Figure 2). Hold this position for 10 seconds.
- Move your lower jaw to the left (see Figure 3). Hold this position for 3 seconds.
- Move your lower jaw to the right (see Figure 4). Hold this position for 3 seconds.
- Move your lower jaw in a circle to the left.
- Move your lower jaw in a circle to the right.


Passive stretching exercise
- Place your thumb under your top front teeth or on your gums.
- Place the pointer (index) finger of your other hand on your bottom front teeth or on your gums (see Figure 5).
- Open your mouth as wide as you can. Push your fingers gently against your teeth or gums to give extra resistance. This will help to keep your mouth from closing. You should feel a gentle stretch, but no pain.
- Hold this position for 15 to 30 seconds.
Your swallowing specialist may notice changes in your ability to swallow. If so, they may teach you other exercises or ways to help you keep swallowing during your treatment.
Dietary guidelines
Eating well is an important part of your cancer treatment. If you’re having pain or trouble swallowing:
- You may not be able to eat enough food. This can make you lose weight and have less energy.
- You may not be able to drink enough liquids. This can make you dehydrated.
Your care team will talk with you about what you should eat and drink during your treatment. Your swallowing specialist will recommend the right food and liquid textures for you. When you try new foods and liquids, make sure they have the textures your swallowing specialist recommends.
Your care team may also recommend you drink nutritional supplements (such as Ensure®) to help you get more calories. You can buy nutritional supplements at your local grocery store, pharmacy, or online.
For more dietary recommendations, read Eating Well During Your Cancer Treatment.
Managing dry mouth or thick saliva
Try these suggestions if dry mouth or thick saliva is a problem for you:
- Drink 8 to 10 (8-ounce) cups of liquids a day. Being well-hydrated will help loosen thick saliva.
- Keep a bottle of water or other liquid with you when you’re away from home. Sip from it often.
- Chew sugarless gum or suck on sugarless candy. This can make more saliva flow.
- Add sauces, gravies, or other liquids to your food.
- Use a humidifier to help loosen thick saliva.
- Rinse your mouth often during the day with a solution you can make. To make your own solution, mix 1 liter (about 4.5 cups) of water, 1 teaspoon of salt, and 1 teaspoon of baking soda. You can sip, rinse, or gargle with the solution.
If these suggestions do not help you, talk with your care team. They can suggest other ways to help manage dry mouth or thick saliva.
Contact information
For more information, contact a speech and swallow specialist in Memorial Sloan Kettering (MSK)’s Speech and Hearing Center. You can reach a specialist Monday through Friday, from to at 212-639-5856.
The Speech and Hearing Center is in Memorial Hospital at:
1275 York Ave. (between East 67th and East 68th streets)
Bobst Building, 4th Floor, Suite 7
New York, NY 10065
The Speech and Swallowing Center is in the David H. Koch Center for Cancer Care at MSK at:
530 E. 74th St.
16th Floor, Suite 11
New York, NY 10021
