This information explains cardiomyopathy caused by chemotherapy, including its signs, how it’s diagnosed, and how it’s treated.
About Cardiomyopathy
Cardiomyopathy is a disease where your heart muscle becomes weak and doesn’t pump blood to the rest of the body as well as it should.
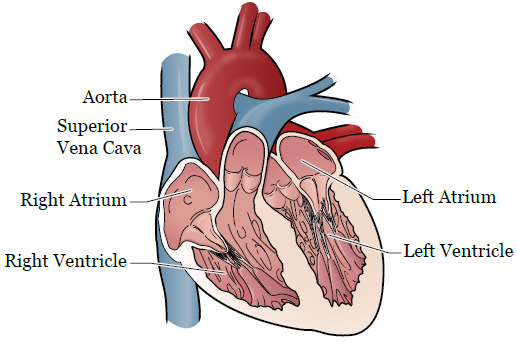
There are many different types of cardiomyopathy. A type of cardiomyopathy that can happen after some chemotherapy treatments is dilated cardiomyopathy. Dilated cardiomyopathy happens when the left ventricle (chamber) of the heart becomes enlarged and can’t pump blood as well as it should (see Figure 1). This can lead to heart failure or arrhythmia. Arrhythmia is when the rhythm of your heartbeat isn’t regular. It can be too fast or too slow.
Causes of Cardiomyopathy in Cancer Patients
For cancer patients, some cancer treatments may cause cardiomyopathy, especially if you have a history of a heart condition.
- Previous heart conditions or diseases that may have caused damage to your heart, such as coronary heart disease and hypertension (high blood pressure).
- Anthracyclines are a type of chemotherapy medication. They include doxorubicin (Adriamycin® and Rubex®), daunorubicin (Cerubidine®), epirubicin (Ellence®), and idarubicin (Idamycin®). You’re more likely to get cardiomyopathy from these medications if you get high doses of them.
- Trastuzumab (Herceptin®). This type of chemotherapy medication is used to treat breast cancer and can cause cardiomyopathy. In many cases, once you stop taking it, the cardiomyopathy should partially or fully go away.
- Radiation treatment to your chest can also put you at a higher risk for developing cardiomyopathy.
If you’re concerned about getting cardiomyopathy after your cancer treatment, talk with your healthcare provider.
Symptoms of Cardiomyopathy
The following are common signs of cardiomyopathy:
- Trouble breathing when you’re active or resting. Some people might also need to sleep sitting up or with many pillows under their head to help them breathe.
- Fatigue (feeling more tired or weak than usual).
- Swelling in your legs, ankles, or feet.
- Coughing, which may be worse when lying down at night.
- Sudden weight gain.
- Bloating in your abdomen (belly).
- Feeling dizzy, weak, or lightheaded.
- Heart palpitations, which may feel like a fluttering or pounding feeling in your chest.
Preventing Cardiomyopathy
You can’t completely prevent cardiomyopathy, but the following suggestions can help you reduce your risk for getting it:
- If you have hypertension, high cholesterol levels, or diabetes, make sure that they’re under control. Read the resource About Hypertension (High Blood Pressure) (www.mskcc.org/pe/high-blood-pressure) for more information on these conditions.
- Avoid drinking alcohol, smoking, or using recreational drugs.
Diagnosing Cardiomyopathy
There are many different tests to diagnose cardiomyopathy. You may have 1 or more of the following tests below. Your healthcare provider will tell you what to expect.
Chest x-ray
This will help your healthcare provider see if there’s fluid in your lungs, if your heart is enlarged, or both.
Echocardiogram (echo)
This is an imaging test that uses ultrasound (sound waves) to take pictures of your heart. It shows how your heart is beating and pumping blood and can show if there’s anything wrong with your heart muscle, heart valves, or both.
Electrocardiogram (EKG)
An electrocardiogram shows the electrical activity of your heart. It shows things such as how fast your heart is beating and if you have an arrhythmia. During this test, your healthcare provider will place sensors (electrodes) on your chest, arms, legs, or all 3. The sensors will show how your heart is working.
Cardiac catheterization (“cath” or angiogram)
During this procedure, your healthcare provider will insert a thin catheter (long, flexible tube) into a blood vessel in your arm or leg and move it up to your heart. Once the end of the catheter is in your heart, your healthcare provider will put a special dye into the arteries of your heart. They’ll use a special x-ray machine to watch the dye move out of your heart and see how it flows through your coronary arteries (the blood vessels that carry blood to your heart muscle). This can help your healthcare provider find out if there are any blockages in your heart or blood vessels.
Cardiac magnetic resonance imaging (MRI)
This test uses a magnetic field and radio waves to make an image of your heart. This can show your healthcare provider how your heart functions. This test may also be done with an echo test as well.
Treating Cardiomyopathy
Cardiomyopathy can be treated with medications, implanted devices, a heart transplant, and sometimes all 3. Your cardiologist (heart doctor) will help you decide which treatment is best for you.
Medication
Many types of medication can treat cardiomyopathy. The following are a few examples of each type, but there are others. Your healthcare provider will decide which type is best for you.
- ACE inhibitors and angiotensin II receptor blockers (ARBs) are medications that relax your blood vessels and lower your blood pressure. This makes it easier for your heart to pump. Some examples are lisinopril (Prinivil®) and losartan (Cozaar®).
- Beta blockers slow your heart rate and lower your blood pressure. This helps reduce the amount of work your heart has to do. Examples are carvedilol (Coreg®) and metoprolol (Lopressor®).
- Antiarrhythmic medications help control abnormal (not normal) heart rhythms. One example is amiodarone (Cordarone®).
- Diuretics (water pills) help your body get rid of extra salt and fluid. They can help with swelling and can help you breathe better. One example is furosemide (Lasix®).
Implanted devices
- Left ventricular assist device (LVAD). This device helps your heart pump blood to the rest of your body. This can be a long-term treatment or a short-term treatment for people who are waiting for a heart transplant.
- Implantable cardioverter defibrillator (ICD). This device keeps track of your heart rate. If it senses a dangerous arrhythmia (abnormal heartbeat), the device will send an electric shock to your heart to help your heart return to a normal heartbeat.
Heart transplant
In a heart transplant surgery, a very diseased heart is replaced with a healthy heart from a donor. This surgery is only done if all other treatments options have failed.
Lifestyle Changes for Managing Cardiomyopathy
There are many ways you can take care of yourself if you have cardiomyopathy. The following are healthy habits and lifestyle changes you can make to help you manage your cardiomyopathy.
- MSK has specialists who can help you quit smoking. For more information about our Tobacco Treatment Program, call 212-610-0507. You can also ask your nurse about the program.
- Weigh yourself every day. If your weight increases by 2 pounds in 1 day or 4 pounds in 1 week, call your healthcare provider. This might mean you have fluid build-up and your diuretic dose may need to be increased.
- Follow a healthy diet.
- Eat less salt in your diet. Most people with cardiomyopathy shouldn’t eat more than 2 grams of sodium every day, but talk with your healthcare provider about the amount that’s right for you. Read the resource 2-Gram Sodium Diet (www.mskcc.org/pe/2-gram-sodium) for more information about following a low-sodium diet.
- Avoid processed foods, such as canned soups, frozen meals, and cold cuts.
- Be as physically active as you can. Talk with your healthcare provider about how much physical activity you should be doing.
- Reduce your stress levels. Some ways to do this include meditation or deep breathing exercises. MSK’ Integrative Medicine and Wellness Service patients and caregivers with services such as massages, acupuncture, yoga classes, reflexology, meditation, and nutritional consults. For more information, call 646-449-1010 or go to www.mskcc.org/cancer-care/integrative-medicine.
- Avoid using recreational drugs and drinking alcohol. Decrease your alcohol intake to no more than 1 drink per day if you’re female and 2 drinks per day if you’re male.
- Get 7 to 8 hours of sleep every night.