The greatest hurdle facing cancer immunotherapy today is understanding why the treatment works for only a subset of the people who receive it — between 20% and 40%, depending on the type of cancer and the particular drug. Several potential biomarkers that can predict a patient’s response to these drugs have been proposed, including the number of immune cells found in a patient’s tumor and the level of a molecule called PD-L1.
But measuring these two biomarkers requires tumor biopsies, and neither is a perfect indication of how well a person will do on immunotherapy.
A new study published in the journal Nature — the result of a collaboration between Memorial Sloan Kettering, the University of Pennsylvania, and the Parker Institute for Cancer Immunotherapy — provides evidence that the blood can be an important source of information regarding a patient’s response to this type of treatment. The team found that blood contains clues about who is responding and who isn’t. Examining those clues could one day help a doctor decide when it’s time to try a different therapy.
It’s Reinvigorating
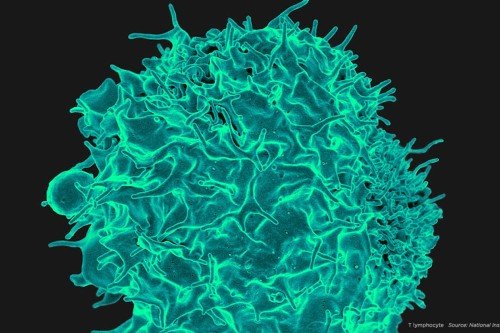
In this study, researchers analyzed changes in the blood of 47 patients (18 from MSK, 29 from Penn) with stage IV melanoma who were treated with the PD-1-blocking drug pembrolizumab. In particular, the researchers looked for signs of “reinvigoration” among circulating immune cells called T cells. (When T cells are overworked, they become “exhausted” and lose their ability to fight cancer; immunotherapy drugs can reinvigorate these cells to help them keep fighting.)
The study authors found that the level of a particular protein made by these T cells was a useful predictor of the outcome to therapy, provided that doctors also took into account the amount of the patient’s cancer — essentially, the size and number of their tumors.
“The idea is that there is a relationship between the reinvigoration of the immune system and the amount of tumor that the patient is facing,” says Michael Postow, a medical oncologist at MSK and a co-author of the paper. “So if a patient has a small amount of tumor and a lot of reinvigoration, they are likely to do well. If the patient has poor reinvigoration and a lot of tumor, they are unlikely to do well — at least with PD-1-blocking drugs alone.”
Dr. Postow suggests that this protein biomarker, when factored in along with other prognostic information, could one day provide doctors with a way to determine early on whether an immunotherapy treatment is working for a particular patient.
“The fact that we can gain useful information about a patient’s response to immunotherapy with just a simple blood draw is a really significant step toward having a biomarker that can guide treatment decisions,” Dr. Postow says. “We’re not quite there yet in terms of the blood telling us everything we need to know, but this study is a good reminder that the blood is an important area in which to look.”
A Freezer Full of Data
To home in on this biomarker, the team analyzed stored blood samples from patients who had been treated with pembrolizumab as part of early clinical trials, some dating back to 2012. It’s routine for patients in clinical trials to have blood collected, frozen, and stored. In this case, that stored blood proved to be a gold mine.
Researchers thawed the blood and then stained it with various antibodies to detect known markers of exhaustion and reinvigoration. One marker of exhaustion is PD-1 itself. PD-1 is a so-called immune checkpoint, a protein that acts as a kind of brake, or check, on immune cell activity. Immune cells make PD-1 as a way to shut themselves down after they’ve successfully controlled a threat — an infection, say, or a budding cancer. But cancer cells are sneaky and can sabotage this natural control mechanism by making a molecule that engages the PD-1 brake on T cells, shutting them down prematurely. That molecule is called PD-L1. Drugs that block either PD-1 (such as pembrolizumab or nivolumab [Opdivo®]) or PD-L1 (such as atezolizumab [Tecentriq®]) prevent the PD-1 brake from being engaged, allowing immune cells to either stay active for longer or even reawaken.
But how could researchers tell, just by analyzing blood, whether these PD-1-positive cells were being reinvigorated? The team found that the number of PD-1-positive T cells that were also making a protein called Ki67 rose dramatically in the weeks following treatment with pembrolizumab. From previous laboratory studies in mice, the researchers knew that Ki67 is a sign of actively dividing immune cells. So their finding then suggested that Ki67 might be an appropriate biomarker of T cell reinvigoration.
Indeed, the change in Ki67 after treatment was a good predictor of a patient’s ultimate outcome — but only when adjusted for the amount of disease. This result indicates that it’s the balance between the two variables that is important. (While 75% of all patients had a rising Ki67 level after treatment, only 38% clinically benefited.)
Mission Possible
The Nature paper is the first major publication to come out of the collaborative Parker Institute for Cancer Immunotherapy, of which MSK and Penn are both founding members. Launched in April 2016, the Parker Institute is the brainchild of serial tech entrepreneur Sean Parker and is led by UCSF immunologist Jeffrey Bluestone.
“I think this study is really emblematic of what Sean Parker and Jeff Bluestone envisioned for the Parker Institute,” says Jedd Wolchok, Chief of the Melanoma Service and Director of the Parker Institute at MSK. “It shows what can be accomplished when cancer centers pool their resources and join intellectual forces to answer common problems.” Dr. Wolchok was the principal investigator of the immunotherapy trial at MSK for which these blood samples were taken. His research has helped establish this immunotherapy approach, called checkpoint blockade. Study co-author Dr. Postow conducts research in Dr. Wolchok’s laboratory, in addition to seeing patients.
At Penn, the study was led by E. John Wherry, an expert in the phenomenon of T cell exhaustion. The idea to combine forces on the study came from a conversation between Dr. Wolchok and Dr. Wherry at a conference. The two scientists recognized that their labs were working on similar problems, and both scientists had samples of stored blood that could be analyzed.
“John then reached out to me, and that’s kind of where this all came from,” Dr. Postow says. “It’s been a great collaboration.”
He adds, “I’m really glad they approached us because this study allowed us to take advantage of the blood that our patients so generously provided.”