Metastasis, the process that allows some cancer cells to break off from their tumor of origin and take root in a different tissue, is the most common reason people die from cancer. Yet most tumor cells die before they reach their next destination, especially if that destination is the brain. In people with lung cancer, for example, occasional tumor cells may enter the bloodstream and infiltrate the brain, but very few survive long enough to seed new tumors.
Now a team of Memorial Sloan Kettering scientists has looked into why most circulating tumor cells die upon reaching the brain and why, in exceptional cases, other cells don’t. Their latest study, published today in the journal Cell, identifies genes and proteins that control the survival of metastatic breast and lung cancer cells in the brain.
These survival factors might one day be targeted with drugs to further diminish people’s risk of metastasis. According to the study’s senior author, Sloan Kettering Institute Director Joan Massagué, a single mechanism is likely to enable cancer cells to colonize various organs, including the brain, in a number of disease types.
An Understudied Disease Type
Metastatic brain tumors occur in several types of cancer — including breast, lung, and colorectal cancer, among others — and are estimated to be about ten times more common than primary brain cancers. Until now, little research has been done into how metastatic brain tumors develop.
Dr. Massagué and his coworkers began to tackle this problem four years ago and have since learned that the brain is better protected than most organs against colonization by circulating tumor cells. To seed in the brain, a cancer cell must dislodge from its tumor of origin, enter the bloodstream, and cross a densely packed vasculature structure called the blood-brain barrier. Mouse experiments in which metastatic breast cancer cells were labeled and imaged over time revealed that a very small number were able to complete this journey, and of those cells that did make it to the brain, fewer than one in 1,000 survived.
“We didn’t know why so many of these cells die,” Dr. Massagué says. “What kills them? And how do occasional cells survive in this vulnerable state — sometimes hiding out in the brain for years — to eventually spawn new tumors? What keeps these rare cells alive and where do they hide?”
Dodging Death Signals
To answer these questions the researchers conducted experiments in mouse models of breast and lung cancer, two tumor types that often spread to the brain, investigating a panel of genes that have been linked to brain metastasis. Their research revealed that many cancer cells that enter the brain are killed by astrocytes — the most common type of brain cell — that secrete a protein called Fas ligand.
When cancer cells encounter this protein, they are triggered to self-destruct by the activation of an internal death program. The study also showed that the exceptional cancer cells that escape do so by producing a protein called Serpin, which acts as a sort of antidote to the death signals fired at them by nearby astrocytes.
Hugging Blood Vessels
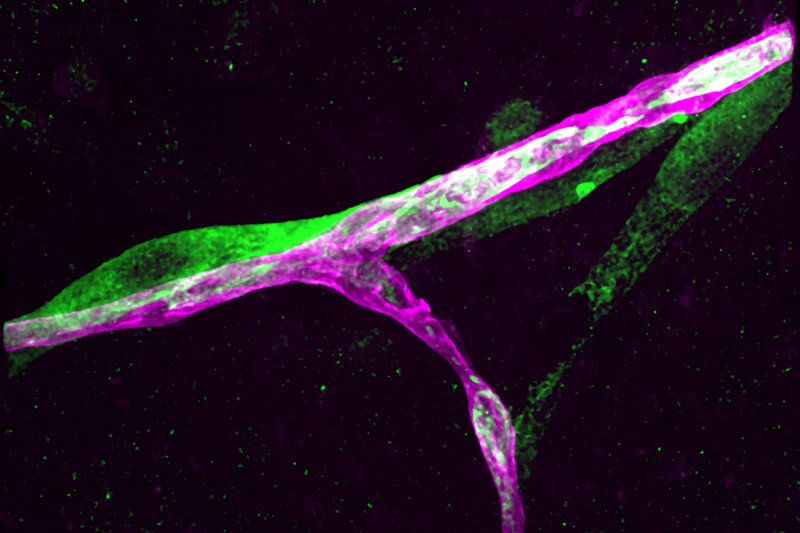
The researchers used imaging methods to examine the behavior of these defiant metastatic cells in the brains of mice. They noticed that the surviving cells grew on top of blood capillaries — each cell sticking closely to its vessel “like a panda bear hugging a tree trunk,” Dr. Massagué says.
“This hugging is clearly essential,” he explains. “If a tumor cell detaches from its vessel, it gets killed by nearby astrocytes. By staying on, it gets nourished and protected, and may eventually start dividing to form a sheath around the vessel.”
Under the microscope, the researchers watched these sheaths grow into tiny balls, which eventually became tumors. “Once you’ve seen it, you can never forget this image,” Dr. Massagué says.
The scientists also did experiments to pinpoint the molecular basis of the cells’ behavior and showed that a protein produced by the tumor cells acts as a kind of Velcro, attaching the cells to the outer wall of a blood vessel.
Therapeutic Ideas
The findings give scientists new possibilities to understand and study the biology of metastasis, and could also lead to the development of new therapies that would work by strengthening the natural impediments to metastasis. The study identifies several mechanisms such drugs could target. Dr. Massagué is particularly interested in the ability of some tumor cells to hug blood vessels, as he suspects this behavior may be essential for the survival of metastatic cancer cells not only in the brain but also in other parts of the body where metastatic tumor growth can occur.
“Most cancer patients are actually at risk of having their tumor spread to multiple sites,” Dr. Massagué notes. For example, breast cancers can metastasize to the bones, lungs, and liver as well as to the brain. “What we may be looking at,” he adds, “is a future way to prevent metastasis to many organs simultaneously,” using drugs that make tumor cells let go of the blood vessels they cling to.





