En esta información se explican las causas, el diagnóstico y el tratamiento del esófago de Barrett.
Información sobre el esófago de Barrett
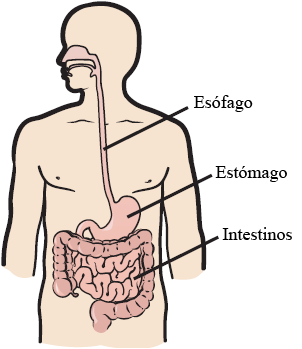
El esófago es el conducto por el que pasan los alimentos que vienen de la boca y se dirigen al estómago (véase la figura 1). Cuando una persona tiene esófago de Barrett, las células normales que revisten el esófago están reemplazadas por células de un tipo que no suele encontrarse allí. Estas nuevas células se asemejan más a las que revisten los intestinos. Este proceso se llama metaplasia intestinal.
Tener esófago de Barrett puede aumentar el riesgo de contraer cáncer esofágico. Debido a ese riesgo, es importante hacerse chequeos médicos periódicos y seguir el plan de tratamiento.
Causas y factores de riesgo
No se sabe exactamente qué causa el esófago de Barrett. La mayoría de las personas que tienen esófago de Barrett han tenido enfermedad por reflujo gastroesofágico (ERGE). La ERGE es un trastorno en el que el contenido del estómago regresa al esófago. También la llaman reflujo. La ERGE puede provocar acidez (una sensación de ardor en la garganta o el pecho).
Con el tiempo, el ácido y la bilis provenientes del estómago dañan el revestimiento del esófago. Algunas personas con antecedentes de ERGE pueden contraer esófago de Barrett si el daño es grave. Lea el recurso Enfermedad por reflujo gastroesofágico (ERGE) para obtener más información acerca de esta enfermedad.
La mayoría de las personas que contraen esófago de Barrett tienen las siguientes características:
- Son mayores (superan los 40 años)
- Hombres
- Son de raza blanca
- Son obesos o tienen sobrepeso
Diagnóstico del esófago de Barrett
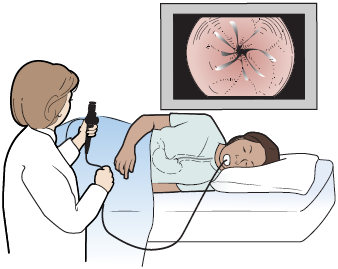
Para diagnosticar el esófago de Barrett, se debe hacer un procedimiento de endoscopia. Durante la endoscopia, su proveedor de cuidados de la salud utilizará una sonda flexible que se llama endoscopio para ver el interior del esófago en una pantalla de video (véase la figura 2).
Antes del procedimiento, le darán anestesia (medicamento para hacer que se duerma), por lo que no sentirá ninguna molestia. Durante la endoscopia, su proveedor de cuidados de la salud se fijará si el color del esófago ha cambiado. Se fijará si hay zonas de color anaranjado en la parte inferior del esófago. Es posible que su proveedor de cuidados de la salud le tome una muestra de tejido del revestimiento del esófago en la zona de color anaranjado y le haga una biopsia. Esta muestra se enviará al departamento de patología de MSK para ver si hay metaplasia intestinal y tejido precanceroso (tejido que puede convertirse en cáncer). Al tejido precanceroso de la muestra se le llama displasia.
Tratamiento del esófago de Barrett
El tratamiento del esófago de Barrett dependerá de si hay o no hay displasia.
Tratamiento en caso de que no haya displasia
Medicamentos
Si no hay displasia, el esófago de Barrett se puede tratar con los mismos medicamentos que se usan para tratar la ERGE. Estos medicamentos ayudan a reducir la cantidad de ácido del estómago y a aliviar otros síntomas que se pueden presentar. También pueden ayudar a evitar que el esófago se irrite. Si los medicamentos no contribuyen a aliviar los síntomas, es posible que se deba hacer una cirugía antirreflujo. Si es necesario hacer la cirugía, su proveedor de cuidados de la salud le explicará en qué consiste.
Los medicamentos no curan el esófago de Barrett, pero pueden ayudar a enlentecerlo para que no empeore. Aunque no haya displasia, su proveedor de cuidados de la salud debe controlar su afección, así que puede ser necesario hacer una endoscopia cada pocos años.
Tratamiento en caso de que haya displasia
Si hay displasia, el tratamiento del esófago de Barrett será diferente. La displasia puede ser de bajo grado o alto grado. El nivel de displasia indica el riesgo de padecer cáncer y ayuda al proveedor de cuidados de la salud a decidir qué tipo de tratamiento es necesario en su caso.
- Bajo grado de displasia: si el grado de displasia que usted tiene es bajo, las células exhiben pocas modificaciones precancerosas. El riesgo de que estas células se conviertan en cáncer es bajo. No obstante, cuanto más zonas haya con displasia de bajo grado, mayor es el riesgo de que esta se convierta en cáncer.
- Alto grado de displasia: si el grado de displasia que usted tiene es alto, las células exhiben muchas modificaciones precancerosas. El riesgo de que estas células se conviertan en cáncer es muy alto.
Hay 2 tipos principales de tratamientos contra la displasia: tratamientos endoscópicos y cirugía.
Tratamiento endoscópico
En los tratamientos endoscópicos se mata o extrae el tejido anormal (las células precancerosas) sin necesidad de extraer el esófago. Los siguientes son los tipos de tratamientos endoscópicos:
- Mucosectomía endoscópica (EMR): durante la endoscopia, es posible que se inyecte una solución salina debajo del tejido anormal para elevarlo. A continuación, el tejido anormal se rasura y se envía al patólogo para que lo analice.
- Destrucción con radiofrecuencia (RFA): durante este procedimiento, se introduce un dispositivo especial por el esófago. Este dispositivo emite breves ráfagas de ondas de radio intensas (calor) para matar el tejido anormal.
- Criodestrucción: durante este procedimiento, se introducen un líquido y un gas muy frío por el esófago a través de un endoscopio, para congelar y matar el tejido anormal.
- Terapia fotodinámica (PDT): durante este procedimiento, se inyecta en la vena un medicamento que hace que las células anormales se vuelvan sensibles a la luz. A continuación, se usa una luz láser roja para matar el tejido anormal.
Cirugía
Es posible que su proveedor de cuidados de la salud le recomiende que se haga una cirugía para extirpar el esófago o las partes dañadas del esófago. A esta cirugía se le llama esofagectomía. Su proveedor de cuidados de la salud le brindará más información sobre este procedimiento si es necesario que se lo haga.
Cambio de hábitos en caso de esófago de Barrett
Si usted tiene esófago de Barrett, su proveedor de cuidados de la salud le recomendará un tratamiento y exámenes de seguimiento. Además, debe intentar poner en práctica los siguientes cambios de hábitos:
- Permanecer sentado después de las comidas. Esto puede contribuir a evitar que el ácido del estómago suba e ingrese en el esófago.
- No ingerir alimentos en las 2 o 3 horas previas a ir a la cama.
-
Evitar alimentos que pueden provocar ácido, como los siguientes:
- Alimentos y bebidas con cafeína, como el café, el té, los refrescos y el chocolate
- Productos lácteos, como la leche
- Menta
- Tomates o salsa de tomate
- Alcohol
- Dormir con la cabecera de la cama elevada, de modo que la cabeza quede a una altura superior a la del estómago. Esto se puede hacer colocando bloques o cuñas debajo de la cama.
- Evitar las comidas abundantes y ricas en grasas, como las que contienen alimentos fritos o carnes procesadas.
Hable con su proveedor de cuidados de la salud si tiene alguna pregunta.
