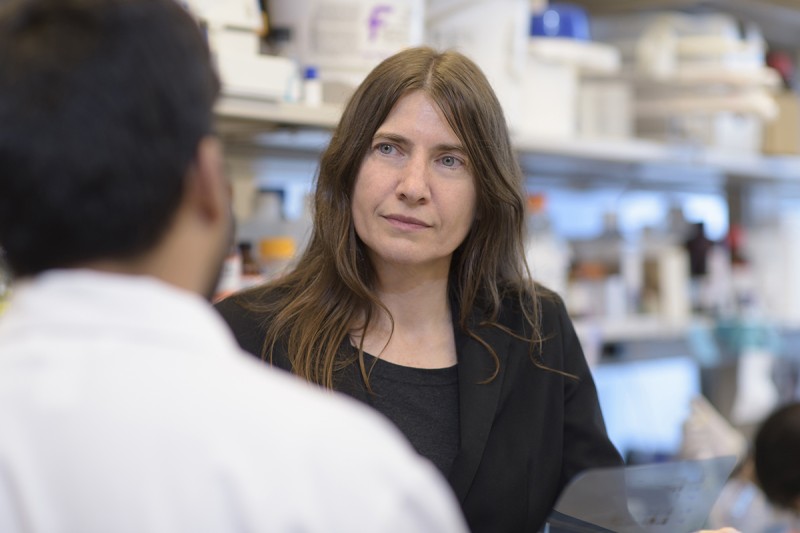
Chemical biologist Gabriela Chiosis is developing drugs that target processes in cells that aren’t working properly.
Like cancer, Alzheimer’s disease involves changes in proteins. When functioning normally, proteins are important for cells to work properly. Also like cancer, Alzheimer’s occurs more commonly in older people, reflecting the idea that it usually takes a long time for these kinds of cellular changes to build up to a point that they cause real damage.
So although it may be a bit surprising, it’s not an impossible stretch to think that a drug developed to treat cancer may also work against Alzheimer’s disease. A family of these drugs has its origins at Memorial Sloan Kettering.
MSK chemical biologist Gabriela Chiosis has developed compounds for both cancer and Alzheimer’s. This week she spoke about her work at the National Institutes of Health’s Alzheimer’s Disease Research Summit. Dr. Chiosis was among top researchers from around the world who were invited to present their research on the biology of Alzheimer’s.
“Of Dr. Chiosis’s many intriguing discoveries, one that stands out is that Alzheimer’s disease shares a common cellular abnormality with many cancers,” says Larry Norton, Deputy Physician-in-Chief for Breast Cancer Programs at MSK, who has collaborated with Dr. Chiosis on the development of drugs. “The fact that there is a common mechanism raises the possibility of a common therapy. So her research could have profound implications for many human diseases, particularly those associated with aging.”
Targeting the Disease Process
Dr. Chiosis’s current work is focused on a type of regulatory network found inside cells called epichaperomes. “Epichaperomes form under conditions of chronic stress, something that is found in both cancer and Alzheimer’s disease,” she says. “One of the roles of these networks is to enhance the processes that become disrupted in diseased cells. These processes include defective signaling, increased production of certain proteins, and inflammation.”
In 2005, Dr. Chiosis and her colleagues developed a drug called PU-H71 for the treatment of cancer. PU-H71 is now in a phase I/II trial for people with metastatic breast cancer. Based on their discoveries about PU-H71, she and her team later developed a related drug, which they called PU-AD, for Alzheimer’s disease.
Both drugs bind to a protein called Hsp90 but only when it’s incorporated into the epichaperome network. Hsp90 is a protein found in essentially every cell in the human body. Its normal role is to help with proper protein folding. But when it becomes part of the epichaperome, Hsp90 contributes to stabilizing the proteins inside cells that let the disease develop.
“The formation of the epichaperome keeps damaged cells alive while they remain dysfunctional,” Dr. Norton explains. “Dr. Chiosis’s discoveries about epichaperomes are important because they are so overarching and could apply to many diseases.”
Taking a Look Inside Cells
Dr. Chiosis’s research has also led to imaging methods for detecting epichaperomes in cancer and Alzheimer’s, called PU-PET and PU-AD PET, respectively. She has collaborated with other investigators at MSK, including radiochemists Jason Lewis and Naga Vara Kishore Pillarsetty and radiologists Mark Dunphy and Steven Larson, on their development.
The approach involves attaching a weak radioactive label to PU-H71 or PU-AD, which then can be imaged with PET scanning. For cancer, PU-PET allows doctors to identify who is most likely to benefit from PU-H71 treatment. It can also help doctors monitor how well the drug is working.
In her presentation at the NIH summit, Dr. Chiosis discussed how an understanding of the epichaperome network can be used to identify some of the changes that occur in a number of different pathways in brain cells. These pathways can lead to Alzheimer’s disease, and learning more about them could suggest possibilities for the development of new targeted drugs.
She also talked about how PU-AD PET can be used to visualize Alzheimer’s disease in the brain. “The negative effects on memory, behavior, and the ability to think clearly that are commonly witnessed in people with Alzheimer’s are due to accumulation of toxic proteins called amyloid and tau in the brain,” Dr. Chiosis says. “But toxic changes in the neuron may begin 20 years before these deposits or the clinical symptoms of the disease develop. As such, we believe that using PU-AD PET to detect Alzheimer’s during this long preclinical phase may provide a promising window of opportunity for treatment.”
Both the PU-PET and PU-AD PET scans are now being tested in clinical trials at MSK. Dr. Norton and Dr. Chiosis have established a company called Samus Therapeutics that is focused on developing these scans as well as new therapies that target the epichaperome.