-
An experimental prostate cancer treatment uses MRI to target radiation and intensify the dose to the tumor — and at the same time reduce side effects.
- It’s more precise because MSK radiation oncologists take multiple MRI images during the procedure to adjust for tumor movement in real time.
When Alexandros Washburn was diagnosed with prostate cancer in early 2021, his first thought was: “Get the tumor out.” Multiple friends, many of them physicians, offered their advice on the best treatment and put him in touch with cancer specialists. But there were so many choices. “Everyone you know has an opinion, and they all recommend an expert you should see,” Alexandros recalls.
He met with two top doctors who made persuasive cases for radiation or surgery. But Alexandros also was doing his own research, which led him to Memorial Sloan Kettering Cancer Center (MSK).
MRI-Guided Radiation and Its Benefits
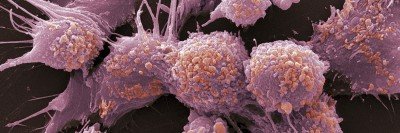
At MSK, he learned about an experimental new radiation approach that might work better than standard therapy. The method uses magnetic resonance imaging (MRI) to safely intensify the dose of radiation to treat the tumor abnormality with extraordinary precision — and reduce the chance the tumor will return in the same spot. The technique, called MRI-guided radiotherapy, enables doctors to obliterate tumors in just five treatment sessions without harming nearby cells.
For certain tumors it provides an advantage over current radiation techniques because it adjusts to changes in the tumor’s position in real time, allowing for the higher radiation dose with incredible focus. Prostate tumors are a moving target, so there is a great advantage to mapping its location at the moment of treatment.
Results from 15 patients receiving the treatment were reported by MSK radiation oncologist and prostate cancer specialist Victoria Brennan at the annual meeting of the American Society for Radiation Oncology (ASTRO). Despite the high radiation doses, the patients did not suffer noticeable side effects — suggesting the new approach is safe and effective.
MSK radiation oncologists have now treated more than 100 people with this technique. They are currently enrolling patients in a phase 2 clinical trial to see if the high-dose method can prevent intermediate-risk prostate cancer from returning.

Which Prostate Cancer Patients Can Benefit From MRI-Guided Radiotherapy?
This treatment is suited to Alexandros’ specific type of prostate tumor — a dominant intraprostatic lesion (DIL), which is visible on an MRI and confined to one spot in the prostate. These cancers tend to be aggressive and have a high rate of recurrence in the same spot. An extra-high dose of radiation could prevent the cancer from coming back.
MSK’s MR-Linac system uses a single device to take images and deliver radiation, allowing doctors to make real-time adjustments to the radiation beam based on slight changes in the tumor’s shape or position.
To Alexandros, a 59-year-old urban designer and father of five living in Brooklyn, this noninvasive treatment sounded like the ideal solution. He could avoid some of the side effects of prostate surgery — such as higher risk of erectile dysfunction or urinary problems — while feeling assured the tumor would be destroyed and unlikely to return.
“My job was just to stay still and breathe, and they did the rest,” Alexandros says.
MRI-Guided Radiotherapy Delivers Intense Doses
The MRI-guided treatment represents the latest advance in radiation therapy pioneered at MSK using precisely targeted, intense radiation doses split into fewer sessions. Over the past decade, MSK doctors have used an approach, called MSK Precise®, to greatly reduce the number of radiation treatments needed for certain prostate cancer patients. It relies on MRIs rather than CT scans.
“Using MRI is an incredible enhancement in accuracy, giving us exquisitely precise live snapshots of the anatomy at each moment,” Dr. Brennan says. “Other institutions are investigating similar technologies, but very few in the world have the image resolution or accuracy that MSK has, and we are doing it routinely with techniques specific to prostate cancer enabling us to focally boost the visible disease. We think this gives us a better chance at eradicating the disease with minimal side effects.”

MR-Linac Device Combines Imaging and Treatment
In 2020, MSK began using a machine that takes images and delivers radiation with a single device. Known as the Elekta 1.5T Unity MR-Linac system, the machine gives radiation oncologists high-resolution scans of the tumor area during the treatment — as the session is happening. Doctors are then able to adjust the radiation beam based on even the slightest changes in the tumor’s shape or position.
Because doctors can pinpoint the radiation so precisely, they can safely increase the dose.
The constant adjustments require meticulous coordination among radiation oncologists and medical physicists. The device is housed in the David H. Koch Center for Cancer Care at Memorial Sloan Kettering Cancer Center.
“We have a team of expert physicists and radiation therapists working with the radiation oncologist in real-time to deliver each adaptive treatment,” Dr. Brennan says. “This enables a highly accurate and focused treatment that adapts to daily changes in the patient’s anatomy.”
In conventional radiation treatment, a CT or MRI might be done at the beginning of all the sessions, and a treatment plan would be based on this information. Unfortunately, the shape and position of the treatment area can shift between sessions.
For the new approach, the MSK team creates a “daily adaptive plan” to tailor the radiation dose based on an MRI. Even during this planning period, which can be about 45 minutes, the bladder might fill with urine, changing the location of the tumor. So just before delivering the radiation, the doctors do an additional “verification” MRI, to see if final small treatment adjustments should be made.
“We often make 2 to 3 millimeter adjustments to adapt to last-minute changes in the position of the tumor or nearby sensitive organs,” Dr. Brennan says. “This enables us to hit the abnormality spot-on, without harming the surrounding organs.”
What MRI-Guided Radiation Is Like for Patients
For Alexandros, the treatment, including the planning, took place over several weeks in May 2021. First, doctors placed fiducial markers (tiny metal objects that are visible on imaging scans) in his prostate. This allowed the team to mark the exact location of the tumor and design a baseline treatment plan. He also had a “spacer gel” placed between the prostate and rectum to move the rectum away from the prostate and the planned radiation target.
Alexandros says, “You really saw the teamwork involved, which impressed me and made me feel good about the process.”
Alexandros then underwent five radiation treatment sessions over a 10-day period. Each lasted about an hour, which included the time needed to make daily adjustments before delivering the radiation.
“With the first treatment, your body is really feeling that you’ve had a serious intervention. But after that, you get used to it,” Alexandros says. “You have to be comfortable being inside an MRI during the treatment, but it was kind of cool to zone out and not worry about anything other than my breathing.”
MRI-Guided Therapy Effective for Alexandros
When all the treatments were done, Alexandros scaled back his normal activity for about a month. Then a friend got him interested in a new civics design project, and Alexandros decided to plunge back into action. He started exercising for an hour a day — usually biking — regardless of whatever else was going on or how he was feeling.
“That combination — getting involved in the civics architectural work and doing regular exercise — opened up the path to getting back to normal,” he says.
Follow-up appointments at MSK suggest the treatment has been effective. Alexandros’ prostate-specific antigen (PSA) levels have dropped dramatically and continue to decline. An MRI has shown no evidence of cancer.
Alexandros continues to keep busy, doing architectural consulting around the world, restarting his second career as a painter, and staying active with his family. He has recommended the radiation treatment to others, including a neighbor who was also considering surgery before consulting at MSK.

Refining the Procedure Further
The team of experts has continued to refine the MRI-guided radiation procedure.
“When we started the program, we were treating one lesion in the prostate. But now we are treating more complex cases with up to four lesions,” says medical physicist Neelam Tyagi, a co-author of the ASTRO abstract.
The integrated team makes it possible to have unmatched image resolution, accuracy, and nuances of treatment.
“Our experience with the first 15 patients gave us a lot of important feedback and allowed us to improve our techniques,” Dr. Brennan says. “We have been able to streamline the whole process so that treatment times are shorter, and we are getting even better coverage of the treatment area.”
This story was originally posted in October 2022 and has been updated.