
Early-stage colon cancer often does not cause symptoms. That’s why we recommend you get regular screenings, based on your risk factors for colon cancer.

You may be reading this because you or someone you care about has learned they have colon cancer. Or maybe you’re curious about your risk of getting colon cancer.
It’s important to get to know the signs of colon cancer. It’s best if we can catch it early, when it may be easier to treat. But at MSK, we have treatment options for colon cancer at every stage.
This guide is a good place to learn about what causes colon cancer and how to prevent colon cancer. You can learn about the signs and symptoms of colon cancer.
This information can help you get ready to talk with your healthcare provider and understand your next steps.
Colon cancer happens when healthy cells in your colon grow out of control and form a mass called a tumor.
Colon and rectal cancers are often grouped together because the colon and rectum are part of the same organ. The colon is the first 5 feet of the large intestine. The rectum makes up the last 6 inches of the large intestine.
Cancer that starts in the colon is called colon cancer. When cancer starts in the rectum, it’s called rectal cancer. Cancer in the colon or rectum is also known as colorectal cancer.

Early-stage colon cancer often does not cause symptoms. That’s why we recommend you get regular screenings, based on your risk factors for colon cancer.

Colonoscopies are screening tests that can find and treat colon cancer in its early stages.

Surgery is a common treatment for colon cancer. Some people also have other treatments, such as chemotherapy.
After you swallow food, it moves into your esophagus (ee-SAH-fuh-gus). This long tube carries food from your mouth into your stomach. In your stomach, the food starts to digest (break down).
From your stomach, the food moves into your small intestine. Digestion also takes place here. The intestines absorb many nutrients. Anything that isn’t absorbed is called waste.
The waste moves to your colon. Some water is reabsorbed (taken back) into your body. The rest of the waste enters the end of your colon, which is called your rectum. Your rectum is a holding area for the waste (poop) until it leaves your body through your anus.
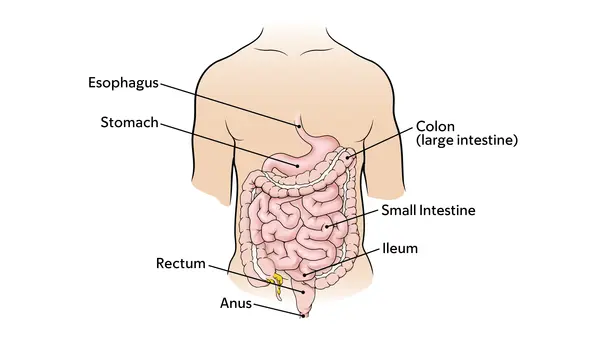
The digestive system, including the colon.

Parts of the colon.
Colon cancer can grow slowly over a few years. It often starts as a small abnormal (not normal) growth on the inside lining of the colon. This is called a colon polyp.
Colon polyps are common, and they are not cancer. Most types will not harm you.
Still, most colorectal cancers start from a polyp. The polyp grows slowly, and it can take as long as 10 years for a polyp to become cancer. For example, most colorectal cancer start in adenomatous (ad-uh-NO-muh-tus) polyps. That’s why it’s so important to remove any polyps that show up during a routine screening. That way we can prevent colon cancer.
Colon cancer starts because of genetic changes (mutations or variants). These genetic causes sometimes may be inherited (passed from parents to children).
A risk factor is anything that raises your chance of getting a disease, such as cancer.
There are some risk factors you cannot control. These include your age, race, or the genes you were born with.
There are other risk factors that you may be able to change. Research shows that having healthy habits can lower your risk for cancer.
A few risk factors can raise your risk for getting colon cancer. Examples are:
Most colon cancers start after age 50. But in recent years, more young people in their 20s, 30s, and 40s are getting colon cancer. Most people under age 50 with colorectal cancer do not have a family history of the disease.
Your risk may be higher if you have had:
Your risk for colon cancer is higher if:
Your risk may be higher because of genetic changes (mutations or variants) you were born with. These mutations may be hereditary (they run in your family).
But only a small number of colorectal cancers are caused by gene mutations that are inherited (passed down from parents).
These are some genes that can mutate and cause colon cancer:
There are inherited conditions that raise your chances of getting colon cancer. They include Lynch syndrome and familial adenomatous polyposis (A-deh-NOH-muh-tus PAH-lee-POH-sis).
You can lower your colon cancer risk by living a healthy lifestyle. This includes eating a balanced diet and exercising regularly. You should also avoid or limit tobacco (smoking, vaping, and chewing tobacco) and alcohol.
These risk factors can raise your risk for colon cancer:
Fiber may lower your risk for some common cancers. Our nutrition experts recommend most people aim for 25 grams of fiber a day. Try to get most of your fiber from whole foods, such as whole grains, vegetables, and fruit. Add fiber slowly with simple changes, like swapping white bread or pasta for whole grains.
You may be at high risk for colorectal cancer if you:
Your race can also play a role in your risk for getting colorectal cancer. For example, colorectal cancers affect the Black community in the U.S. at a higher rate than other races.
Talk with an MSK Care Advisor. We're here 24 hours a day, 7 days a week.
The genes you were born with (inherited) can raise your chances of getting colorectal cancer.
MSK is one of the few hospitals that can test for changes in many genes at the same time. Our multi-gene panel test can find a hereditary cause of cancer faster. This genetic testing can help us find the best treatment for the type of colon cancer you have.
MSK’s test checks DNA for mutations linked to hereditary colorectal cancer and polyposis. It also can check for gene mutations linked to Lynch syndrome, which can cause colorectal cancer.
Having Lynch syndrome raises your risk for colon and rectal cancers. MSK has a special program to help families with Lynch syndrome. Our experts will monitor you and schedule regular cancer screenings. MSK CATCH can help prevent or catch colon cancer at an earlier stage, when it’s easier to treat.
There are some steps you can take to lower your risk for colon cancer. There also are some risk factors that you cannot control.
Research shows that some healthy habits can lower your risk. Making healthier choices in your everyday life can help.
You can also lower your risk by taking care of your health in these ways:
Eat more fruits, vegetables, and fiber, and less animal products and fat. To learn more, we have information about following a healthy diet. By making healthy food choices, you can lower your cancer risk by:
Exercise regularly. Even some regular physical activity can lower your risk for colon cancer. Try taking the stairs instead of the elevator, and walk whenever you can.
Keep a healthy weight. Obesity is a big risk factor for colon cancer.
Talking about cancer screening and risks with your doctor can help you feel confident when making decisions about your care.
Colon cancer screening means getting routine tests to find colon cancer, even before you have any signs or symptoms. The goal of regular screening is to find cancer early, when it’s easier to treat.
Colon cancer screening aims to find tumors or lesions that are precancerous (can become cancer). This lets us remove precancerous lesions before they can form a tumor.
The most common screening test for colon cancer is a colonoscopy.

Gastroenterologist Dr. Mark A. Schattner is a colon cancer screening expert at MSK in New York City.
There are a few kinds of colorectal cancer screening tests and guidelines.
A colonoscopy is the most common way to screen for colorectal cancer. It’s the only screening test that can both find and remove small growths on the colon’s inner lining.
These growths in the colon or rectum are called polyps. They’re not cancer, but can become cancer. This means that a colonoscopy can both find and prevent colon cancer.
Your doctor will put a flexible tube with a camera through your anus. They’ll look at your rectum and colon. Watch our video to see what happens during a colonoscopy.
A flexible sigmoidoscopy uses a shorter tube than a colonoscopy. Like a colonoscopy, your doctor can remove polyps. But they can only check the lower part of the colon.
A virtual colonoscopy, also called a CT colonography, is an imaging test. CT scan technology makes 2D and 3D images of the colon and rectum. You may still need a regular colonoscopy if we must get a sample or remove a polyp or other lesion.
Other tests are based on stool (poop) to indirectly look for signs of cancer or polyps. One example of a stool DNA test is known by its brand name, Cologuard. You’ll still need a colonoscopy if the test result suggests you may have polyps.
Learn more about screening tests for colon cancer.
These are MSK’s latest screening guidelines for colon cancer. They may be different from those of other groups of experts. We base your type of screening, and your screening schedule, on your personal risk for colon cancer.
It’s important to talk with your doctor about your level of risk for getting colon cancer. You can decide on the best schedule to start colon cancer screening.
MSK recommends people at average risk for colon cancer start getting screened at age 45.
We also recommend people at higher risk for colorectal cancer talk with their healthcare provider about when to start screening.
If you’re 75 or older, talk with your healthcare provider about whether screening is right for you. In general, we do not recommend routine screening after age 85.
You’re at average risk for colorectal cancer if you’re 45 or older and have:
You’re at higher risk for colorectal cancer if you:
Colon cancer often does not cause symptoms in the early stages. That’s why we recommend you get regular screenings for colon cancer, such as a colonoscopy, even if you feel well. Screening needs are based on your age, health history, and other risk factors.
There are some things that may be signs of colon cancer. If you have any rectal bleeding or blood in the stool, tell your doctor right away.
This video has information about the guidelines for when to get colorectal cancer screening, what the test is like, and why it's important to get screened.
Visit your healthcare provider if you notice these possible symptoms of colon cancer, and they last for 2 weeks:
Most often, these symptoms do not mean you have colon cancer. Tell your healthcare provider if a symptom is very bad or lasts longer than 2 weeks.
When you turn age 45, it’s time to schedule a colonoscopy. If you’re younger than 45, it’s very important to watch for these symptoms. Talk with your healthcare provider right away.
More young people are getting colon cancer. MSK cares for about 500 people with young-onset colorectal cancer each year.
MSK's Ralph Lauren Center offers free or lower cost cancer care, including referrals for colorectal cancer screenings. Some people do not get screened because they’re worried about the cost, say MSK researchers. New York residents who are uninsured or underinsured may be able to get screened with no out-of-pocket costs.
Our experts always are discovering new information about colon cancer. We’re learning ways to diagnose the exact type and stage of colon cancer. We’re finding out how to find it early when it’s easier to treat. Explore the latest colon cancer news from MSK.

Research by MSK psychologist Rosario Costas-Muñiz has uncovered some of the main barriers Latinos face in colorectal cancer prevention.