The ability to isolate and grow pluripotent stem cells has offered many new opportunities for biological and medical research since the technique was first developed about 20 years ago. These cells are remarkable because they have the ability to develop into any type of cell in the body — from liver cells to nerve cells to heart cells and more.
The field of regenerative medicine is based on the premise that doctors may eventually be able to engineer stem cells to replace tissues that have been lost due to injury or disease. Increasingly, pluripotent stem cells are also proving to be a valuable tool in the lab, especially for studying how genetic changes affect cell growth and division.
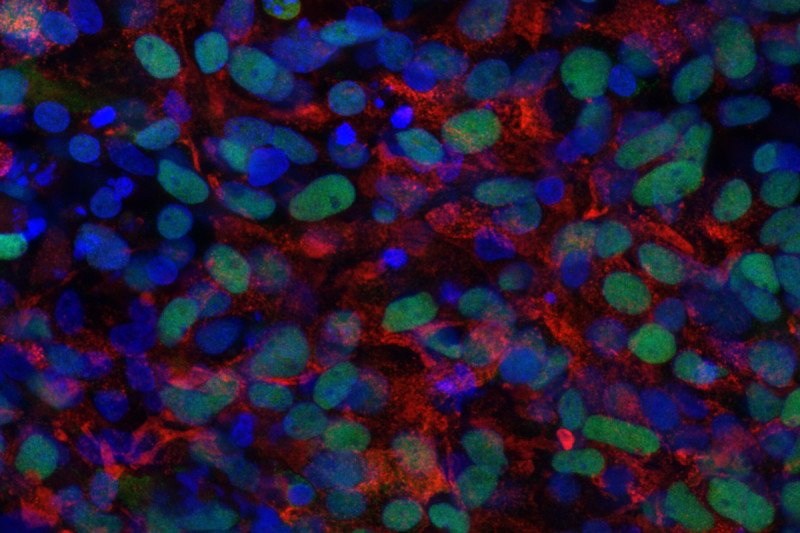
In a new study published February 9 in the journal Cell Stem Cell, a team of researchers led by Memorial Sloan Kettering developmental biologist Danwei Huangfu has demonstrated the value of using pluripotent stem cells to study how pancreatic cells form in a person. Their research has implications for the study of diabetes — a disease characterized by dysfunction in certain types of pancreas cells — as well as pancreatic cancer.
“Many diseases have been difficult to recreate in animal models like mice, which makes it hard for us to study them,” Dr. Huangfu says. Using pluripotent stem cells to create pancreas cells in a dish is teaching her lab members about the role certain genes play in pancreatic diseases and may lead to new kinds of treatments.
Making Changes with Gene Editing
In the new study, the investigators looked at the function of a gene called GATA6 in pancreas cells. In humans, mutations in this gene can cause a range of medical problems that result from the inability of the pancreas to develop and function normally.
To study the gene, the team used a gene-editing technology called CRISPR/Cas9, which acts like a molecular scissors and enables researchers to make precise changes to DNA. Specifically, the MSK researchers used the technology to create pancreas cells that had only one copy of the GATA6 gene rather than the normal two copies, a state called haploinsufficiency. This situation is similar to what is seen in some forms of diabetes.
Recreating these defective pancreas cells in a dish has already enabled the researchers to make new discoveries about GATA6 and its interaction with another gene called GATA4 in pancreatic defects, some of which they report in the Cell Stem Cell paper.
“We believe this is the first study in human pluripotent stem cells to look beyond diseases caused by relatively rare single-gene mutations,” Dr. Huangfu says. “Our research illustrates the important contribution that human pluripotent stem cells can make in studying common but complex diseases characterized by multiple genetic factors as well as by potential environmental factors.”
Implications for Cancer Research
Dr. Huangfu’s lab is also using gene editing to study the formation of cancer in the pancreas. “Because MSK sequences many of our patients’ tumors, we know a lot about the mutations that are present in cancer,” she says. “But we don’t always know which ones are important.”
In cancer, genetic changes in tumors are categorized as driver mutations — errors that are important for the formation and growth of tumors — or passenger mutations, which just go along for the ride.
“Doing experiments with cancer genes inserted into these pancreas models helps us understand the cellular basis of the disease, and to separate the drivers from the passengers,” Dr. Huangfu explains. “Then we can work toward developing better diagnostic methods and treatments for cancer, based on knowing which mutations come first and which are the most important.”