For patients with acute myelogenous leukemia (AML), a rare blood cancer, the biggest problem is relapse following initial treatment: The cancer resurges in about 85% of cases, usually causing death.
Memorial Sloan Kettering chemical biologist Gabriela Chiosis is hoping to change that grim statistic.
For several years, Dr. Chiosis has been developing a new drug — dubbed PU-H71 — that she hopes will provide more durable control of the disease. In a recent paper published in Cell Reports, Dr. Chiosis and her colleague Monica Guzman of Weill Cornell Medical College present new findings that help explain why PU-H71 kills some AML cells but not others.
The drug is most effective at treating AML cells that are “addicted” — the technical term — to a particular network of signals in the cell. By disrupting this network, the drug removes crucial support that leukemia cells need to grow.
PU-H71 is already being tested in clinical trials, and the new research may help doctors select the most appropriate patients to receive it.
Designer Drug
The drug Dr. Chiosis studies is not a chemical that existed in the world before she created it. “PU-H71 didn’t come out of screening existing chemicals,” Dr. Chiosis says. “It’s a compound unknown to man or nature.”
She designed the drug by first looking at the structure of the target she wanted to hit — a protein called Hsp90. Using computer-aided models to visualize its structure, she found that Hsp90 had a distinct “pocket” that made it a particularly tempting target for a structurally minded chemical biologist like her. “I looked at the pocket in the protein and mentally designed a chemical to fit in it,” she says.
The first time she tested her newly built chemical, it behaved just the way she hoped it might — blocking Hsp90 in tumor cells from binding ATP, and therefore from doing its job. Years of additional chemical optimization eventually resulted in the drug PU-H71.
Addicted to Signaling
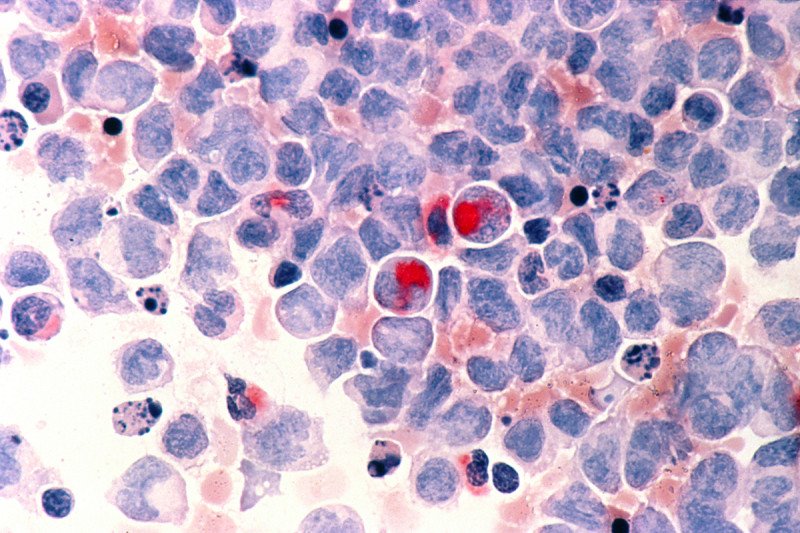
Like all cancers, AML is driven by mutations that lead cells — in this case, white blood cells — to divide uncontrollably. Many of these mutations affect proteins that are part of signaling networks that communicate important messages through the cell. Cancer results from inappropriate activation of these signals — including, for example, signals for growth that are permanently stuck “on.”
As AML becomes more aggressive, it grows more addicted to these growth signals — and therein lies a weakness that scientists can exploit. Interrupting this network of signals deprives the cancer cells of their signaling “fix,” cutting them off cold turkey.
How can a single drug such as PU-H71 affect multiple signaling proteins at once? Many proteins require the assistance of special molecules called chaperones that help them fold properly and guide them to the right place in the cell. Hsp90 — the target of PU-H71 — is the particular chaperone that assists most signaling proteins. Blocking the action of Hsp90 disrupts all the signaling proteins that depend on it.
Unlike many other anticancer drugs, including many chemotherapies, PU-H71 kills cancer cells specifically. That’s because PU-H71 targets a form of Hsp90 found only in cancer cells, leaving normal cells unaffected. That means less toxicity for patients.
And, because a whole network of signals is disrupted rather than just one or two, it should be much harder for cancer cells to develop resistance to the drug.
Selecting the Appropriate Patients
Not all AML cells respond equally well to PU-H71, raising the question of which patients should receive it. With other targeted drugs, such as BRAF inhibitors in melanoma or Herceptin in breast cancer, it’s clear who should get the drug: individuals with a BRAF mutation or HER2 overproduction. But for AML, there is no one mutation that correlates with response to PU-H71, a fact that has plagued drug development efforts.
“Over 20 Hsp90 inhibitors have entered clinical testing, but they have progressed very slowly because it has not been possible to figure out the right patients to target,” Dr. Chiosis says. “If your therapy works on only 10 percent of patients, you need to know who those 10 percent are.”
Dr. Chiosis’s research suggests that only patients with AML cells that are highly addicted to signaling networks will respond to the drug. Targeting just these cancers provides a way to tailor the treatment to the patients most likely to respond.
A Big Step Forward
The new research would not have been possible without extensive collaboration across multiple labs and disciplines. “You really have to put people from different fields and with different minds together to get to a great answer,” Dr. Chiosis says. “Otherwise, you’re always stuck with the little answer and only little steps forward.”
In addition to her collaboration with Dr. Guzman of Weill Cornell, Dr. Chiosis worked with basic scientists and clinicians in several other departments at MSK. The strong support for translational research that bridges basic and applied science has been crucial to the success of the project, she says.
“There aren’t many places you can take something all the way from a computer screen to the clinic,” she notes.


