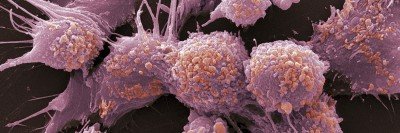
A diagnostic technique called liquid biopsy is quickly emerging as an alternative to conventional tissue biopsy. This less-invasive method screens a person’s blood for cancer cells that have broken free from a tumor and are circulating the body. The cells can be analyzed to reveal critical information about how the cancer may be progressing or responding to treatment.
Liquid biopsy has already shown promise for guiding prostate cancer treatment decisions. By detecting molecular markers in the circulating tumor cells (CTCs), doctors hope to determine which drugs are likely to work better. The challenge has been to prove conclusively that these markers are reliable. Circulating tumor cells represent approximately one cell in a billion of those found in the bloodstream, so the test must be exquisitely sensitive.
Now a study published in JAMA Oncology provides solid proof that a liquid biopsy can accurately predict the best therapy option for many people whose disease has become resistant to initial treatment.
“This test is an important advance in helping doctors and patients make treatment choices more confidently after frontline therapy no longer works,” says Memorial Sloan Kettering medical oncologist Howard Scher, who led the study. “The uncertainty can be a source of great anxiety among patients and families.”
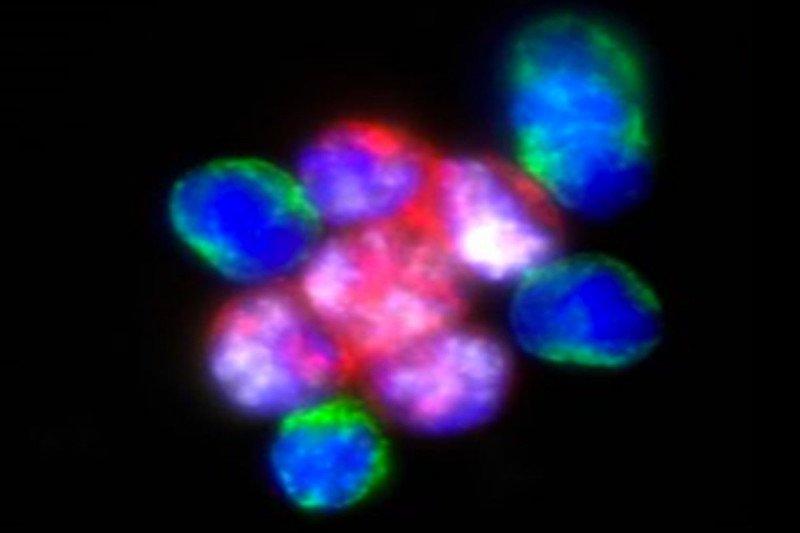
The test focuses on a protein found in people with metastatic castration-resistant prostate cancer (mCRPC), the most advanced form of the disease. The protein, AR-V7, is altered due to a genetic mutation. Developed by Epic Sciences, the Oncotype DX® AR-V7 Nucleus DetectTM test detects AR-V7 in CTCs. The presence or absence of AR-V7 predicts how well the cancer will respond to a therapy.
A Prostate Cancer Treatment Dilemma
Virtually all men with metastatic prostate cancer develop the castration-resistant form. This means the cancer continues growing despite treatment to bring its main source of fuel, testosterone, to low levels. Patients with mCRPC usually receive a drug called an androgen receptor (AR) inhibitor as a first treatment. These next-generation drugs, which include abiraterone and enzalutamide, are usually less toxic than chemotherapy and can be taken by pill at home. Most people respond well to them.
However, if the cancer becomes resistant to the first AR inhibitor, giving a second AR inhibitor is often ineffective. Clinicians have not been able to predict whether the subsequent treatment should be a second AR inhibitor or a type of chemotherapy drug called a taxane. It was hard to tell which category a patient fell into.
In recent years, research has suggested that AR-V7 could hold the key to solving this problem. Patients who failed initial treatment with AR inhibitors and whose cancer cells have AR-V7 seemed to respond better to taxane chemotherapy than an AR inhibitor. Conversely, patients who did not have the mutated version fared better on a second AR drug.
Researchers have hoped that a liquid biopsy focused on AR-V7 in CTCs could point the way to the best second-line treatment option. In 2016, research led by Dr. Scher provided preliminary evidence for this by looking at how AR-V7 would predict drug response using more traditional measures such as prostate specific antigen levels and whether the cancer progressed.
Independent Validation of a Treatment Decision Tool
The new study provides conclusive, independent validation of these findings by looking at how long mCRPC patients survived following second-line treatment with either drug. The researchers analyzed data from 248 patients from MSK and institutions in Canada and the United Kingdom. The AR-V7 status was determined analyzing CTCs in a single blood draw. The patients were followed for up to 4.3 years.
Patients with AV-V7-positive CTCs lived longer when treated with chemotherapy (median overall survival was 14.3 months) compared with those treated with ARS inhibitors (7.3 months). In contrast, patients with AR-V7-negative CTCs lived longer when treated with AR inhibitors (median overall survival 19.8 months) than those treated with chemotherapy (12.8 months).
“That is a significant difference in survival time and illustrates the value of this test in making a more informed treatment decision,” Dr. Scher says. “Even for AR-V7 patients who cannot receive chemotherapy — or choose not to — this test can help them avoid ineffective AR inhibitors and direct them to other treatments or enrollment in a clinical trial.”