This information explains what an artificial urinary sphincter (AUS) is. It also explains the surgery to have it placed and what to do after surgery.
About your urinary sphincter
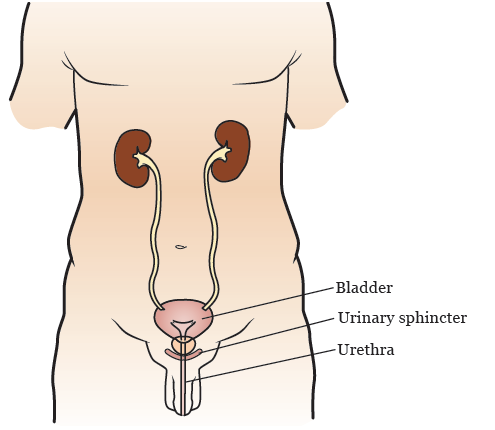
Your urinary sphincter is a muscle that controls the flow of urine (pee) out of your bladder (see Figure 1). When your urinary sphincter is contracted (closed), it blocks the opening of your bladder. This stops urine from leaking out.
Normally, your urinary sphincter stays closed until you choose to relax (open) it to urinate (pee). When you relax your urinary sphincter, urine leaves your bladder and flows out of your body through your urethra. Your urethra is the tube that carries urine from your bladder out of your body.
Some people have trouble controlling their urinary sphincter. This causes them to leak urine. This can happen after surgery to remove the prostate or radiation therapy to the prostate.
About artificial urinary sphincters
If you lose control of your urinary sphincter, you may need an AUS. An AUS is a device that works like your natural urinary sphincter (see Figure 2). It is made up of 3 parts:
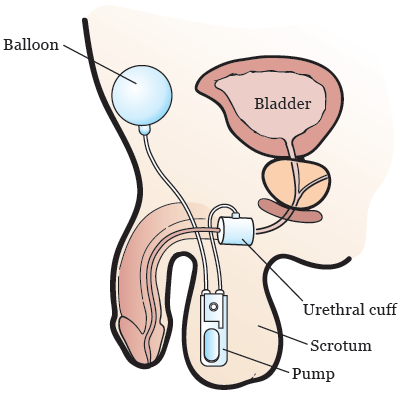
- Urethral cuff: This wraps around your urethra to control the flow of urine. When the cuff is closed (filled with fluid), no urine can pass through. When it’s open (not filled with fluid), urine can pass through.
- Pump: The pump goes into your scrotum and moves fluid into or away from the urethral cuff.
- Balloon: The balloon goes under your abdominal (belly) muscles. It holds the same fluid as the cuff. Fluid moves to the balloon when the urethral cuff is open or deflated.
To urinate with an AUS, you must squeeze the pump in your scrotum. The pump moves fluid from the urethral cuff into the balloon. This allows the cuff to open or deflate and your urethra to open. The cuff stays open for about 3 minutes so that you can urinate. The cuff will close automatically.
A urologist will do the surgery to place your AUS.
Risks of having an AUS
The following problems are not common, but can happen with an AUS:
- Pain.
- Bleeding.
- Infection. If this happens, your healthcare provider may remove your AUS.
- Problems with any part of the AUS. If this happens, your healthcare provider may replace your AUS or take it out.
- Injury to your urethra.
- Leakage of urine that does not stop.
- Long-term or permanent problems urinating. Your healthcare provider may put a catheter into your bladder to drain your urine. You may also need to have another surgery to fix the problem.
- Trouble holding in your urine.
Your AUS can wear out over time. This usually takes 8 to 10 years. When it does, you will need to have it replaced.
About your AUS placement surgery
Your healthcare provider will give you information about how to get ready for your surgery. Follow their instructions. Call your doctor’s office if you have any questions.
What to expect during your AUS placement surgery
You’ll get anesthesia (medication to make you sleep) before your surgery. Once you’re asleep, your surgeon will make 2 small incisions (surgical cuts). They’ll make an incision in the space between your scrotum and anus. They’ll make the other incision near your lower abdomen (belly). Your surgeon will then place your AUS.
When the surgery is done, they will close your incisions with sutures (stitches). These will dissolve on their own. You do not need to have them removed.
What to do after your AUS placement surgery
In the Post-Anesthesia Care Unit (PACU)
You’ll be in the PACU when you wake up after your surgery. A nurse will be keeping track of your temperature, pulse, blood pressure, and oxygen levels. You may get oxygen through a tube resting below your nose or a mask over your nose and mouth. You’ll also have compression boots on your lower legs.
You will have a urinary (Foley®) catheter to drain urine from your bladder. Your care team will give you fluids, antibiotics, pain medicine, and other medicine as needed through an intravenous (IV) line.
These devices are usually removed before you leave the hospital. If you leave the hospital with any of them in place, your healthcare provider will teach you how to care for them.
Urine may leak from your AUS after your surgery. This is normal. It should stop once your doctor activates the AUS. They will do this about 6 to 8 weeks after your surgery.
Call your doctor’s office to make a follow-up appointment for about 2 weeks after your visit.
Order MedicAlert® jewelry
Before you leave the hospital or at your first follow-up visit, order a MedicAlert® bracelet or necklace. Your healthcare provider will give you an order form. Your bracelet or necklace should have the following information:
AUS: Artificial Urinary Sphincter
Brand: AMS 800
Phone: 800-328-3881
Medicine
You may get prescriptions for the following medicine before you go home:
- An antibiotic.
- Pain medicine.
- A stool softener to prevent constipation (having fewer bowel movements than usual).
You will be able to go home the day after your surgery.
At home
Your bandages may fall off or get dirty in the first 48 hours after your surgery. If they do, replace them with clean bandages.
Showering
You can shower 48 hours after your surgery. If you have any bandages, take them off when you shower. You do not need to put more bandages on after you shower.
Wear a scrotal support
For the first week after your surgery, you must wear the scrotal support that you received before you left the hospital. If the scrotal support gets wet, you will need to replace it. You can buy another scrotal support at any drug or surgical supply store.
Going back to your normal activities
You can go back to doing most of your normal activities the day after your surgery.
You’ll need to wait 6 weeks to do any strenuous activity. This includes:
- Working out at the gym.
- Playing golf.
- Riding a bicycle.
- Lifting objects heavier than 10 pounds (4.5 kilograms).
Your doctor will tell you when you can resume sexual activity.
Make a follow-up appointment
Schedule an appointment with your doctor 2 weeks after your surgery. Call your doctor’s office to make the appointment.
When to call your healthcare provider
Call your healthcare provider if you have:
- A fever of 101 °F (38.3 °C) or higher.
- Increased bleeding or swelling.
- Pain that doesn’t get better even after you take pain medicine.
- Severe bladder spasms.
- Trouble urinating.