This information explains your reproductive system and how cancer treatment may affect your fertility (your ability to have biological children). It also explains your options for building a family after cancer treatment.
About your reproductive system
Your reproductive system is in your lower abdomen (belly). It’s made of many parts that work together to help you have sex, menstruate (get your period), make eggs, get pregnant, carry a pregnancy, and give birth (see Figure 1).
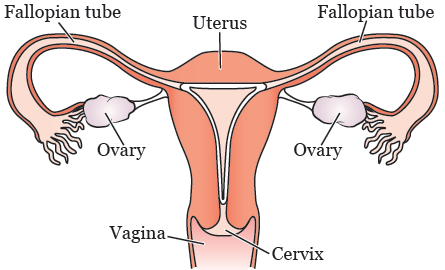
Your reproductive system includes your:
- Vagina: Your vagina is the canal that connects your vaginal opening to your uterus.
- Uterus: Your uterus is a hollow, pear-shaped organ between your bladder and rectum. The muscles in your uterus expand during pregnancy to hold a baby. The lower end of your uterus is called your cervix.
- Ovaries: Your ovaries are small, oval-shaped glands on the left and right side of your uterus. They make, store, and release eggs into your fallopian tubes when you ovulate. They also help your body make hormones.
- Fallopian tubes: Your fallopian tubes are narrow tubes attached to the upper part of your uterus. They help your eggs travel from your ovaries to your uterus.
About ovulation
You’re born with about 1 million eggs. After puberty, your hormones help the eggs in your ovaries mature. Each month, 1 mature egg goes into your fallopian tube. This is called ovulation.
If sperm goes into your egg, it may form an embryo (early stages of a baby). The embryo passes into your uterus, where it grows into a baby. If sperm doesn’t go into your egg, your uterus lining breaks down and bleeds, causing a period.
About menopause
As you age, the number and quality of your eggs decreases. With fewer and less quality eggs, it’s harder to get pregnant and your monthly periods may become irregular. At around age 50, you will have so few eggs that your monthly periods will stop. This is when menopause (a permanent end of your monthly periods) starts. About 5 to 10 years before menopause, you will become infertile (unable to have biological children).
How cancer treatment may affect your fertility
Some cancer treatments may affect your fertility. Since there are many things that can affect fertility, it’s hard to know how you may be affected by your treatment.
We cannot know for sure if you will be able to get pregnant after treatment or not. If you’re fertile after your treatment, it may be for a shorter period of time than it would have been without treatment. If you have questions about how your treatment may affect your fertility, talk with your healthcare provider.
Here are some examples of how cancer treatment may affect fertility.
Fertility after chemotherapy
-
Some chemotherapy medications destroy eggs. This may lead to infertility after treatment. Factors that may impact your future fertility include your age and the type of treatment you receive.
- The older you are during treatment, the less eggs you have already so losing more eggs will likely affect your fertility.
-
Chemotherapy can also impact your ovaries. This affects your fertility the same way that natural aging does.
- Some people may lose so many eggs that they become infertile and begin menopause right after treatment.
- Some people still have eggs after treatment but may start menopause at a younger age. This means that you may still be able to get pregnant after treatment but not for long.
- Some people are not affected by chemotherapy and are able to get pregnant.
Fertility after radiation therapy
-
Radiation therapy to the pelvis or whole abdomen (belly) destroys eggs. Radiation may also damage the uterus.
- People who get high doses of radiation to the uterus will not be able to become pregnant or carry a pregnancy.
- People who get lower doses of radiation to the uterus may become pregnant, but their uterus may not be able to fully expand. This increases the chances of having a miscarriage (when a pregnancy ends on its own) or premature labor (having a baby before your due date).
- Radiation therapy to the brain may affect your pituitary gland. This gland makes the hormones that help you grow eggs and ovulate. You may need to take hormone medication to help you get pregnant.
Fertility after surgery
- Having surgery on your pelvis may affect your reproductive organs, such as your ovaries and uterus. Depending on the surgery, this can affect if you can get pregnant or carry a pregnancy.
- Having brain surgery may affect your pituitary gland. This doesn’t damage the eggs in your ovaries. You may need to take hormone medication to help you get pregnant.
How to check your fertility after cancer treatment
After your treatment, talk with a reproductive endocrinologist to discuss your fertility. A reproductive endocrinologist is a doctor that specializes in fertility. We recommend waiting at least 1 year after completing cancer treatment to see a reproductive endocrinologist. This gives your ovaries time to recover from treatment.
Your reproductive endocrinologist will do many tests to check your fertility. These tests may include:
-
A transvaginal ultrasound. This is when your doctor places a thin wand in your vagina to see inside your ovaries and uterus. They will see if you have enough eggs to get pregnant naturally or with some type of fertility treatment.
- Your doctor may be able to do the ultrasound using a wand placed on your abdomen instead of your vagina.
- Blood tests. Blood tests are done to measure your hormone levels related to fertility. Your doctor will check your anti-mullerian hormone (AMH) levels. The more eggs you have, the higher your AMH level.
Your reproductive endocrinologist will review your results with you. They will recommend the best options for building your family based on your results.
Pregnancy after cancer treatment
Talk with your healthcare provider before trying to get pregnant
Talk with your healthcare provider before trying to get pregnant after cancer treatment. They may recommend you wait at least 1 to 2 years after treatment before trying to get pregnant. There are many reasons for this:
- If you had chemotherapy or radiation to your pelvic area, some of your eggs may have been damaged. It takes about 1 year to clear these from your ovaries.
- Your body needs time to recover from treatment so it’s able to handle pregnancy.
- If you become pregnant during this time when you’re most at risk for an early recurrence (cancer coming back), your healthcare providers may not be able to monitor you with certain tests or scans.
Ask your healthcare provider if you will have a high-risk pregnancy
While some people don’t have any problems with pregnancy after cancer treatment, some may have a high-risk pregnancy. This depends on the type of treatment you had and the possible late effects from that treatment.
Talk with your healthcare provider about how your treatment may affect your pregnancy. Ask them if you should see a maternal fetal medicine (MFM) specialist. If your healthcare provider recommends this, you may need to talk with an MFM specialist before you try to get pregnant.
Ask your healthcare provider if you’re at risk for early menopause
If you aren’t ready to start a family yet, ask your healthcare provider if you’re at risk for early menopause. If you’re at risk, you may want to learn about freezing your eggs or embryos so you can use them in the future.
For more information, read Fertility Evaluation and Fertility Preservation After Cancer Treatment: Options for People Born with Ovaries and a Uterus.
Your options for building a family after cancer treatment
Once you’re cleared by your healthcare provider, your options for building a family after cancer treatment may include:
- Natural conception
- Assisted reproductive options such as ovarian stimulation, intrauterine insemination, or in vitro fertilization
- Using your own frozen eggs or embryos
- Using donor eggs or embryos
- Surrogacy
- Adoption
Natural conception
Some people can get pregnant without medical help. If you try to get pregnant and aren’t able to after 3 to 6 months, make an appointment with a reproductive endocrinologist. They will do tests to check your fertility. Based on the results, they will discuss family building options with you.
Assisted reproductive options
Based on your testing, the fertility doctor will recommend family building options that may include:
- Ovarian stimulation: Your healthcare provider will prescribe medication to stimulate the ovaries to ovulate and increase your chances of pregnancy.
- Intra-uterine insemination (also called IUI or artificial insemination): This is when your healthcare provider places sperm (from your partner or a donor) in your uterus around the time you ovulate. This helps the sperm get closer to your egg and may help you get pregnant.
- In vitro fertilization (IVF): With IVF, you will need to have ovarian stimulation to mature your eggs. After your eggs are mature, you have a procedure to remove the eggs from your ovaries. Your eggs are mixed with sperm (from your partner or a donor) in a lab to make embryos. Then, you will have a procedure where your healthcare provider puts 1 or more embryos into your uterus. This is called an embryo transfer. You and your healthcare provider will decide how many embryos to transfer. The rest of your embryos can be frozen and stored so you can use them in the future.
Using your own frozen eggs or embryos
If you froze your eggs or embryos before treatment, you can use them to try to get pregnant. Here are the steps to the process:
- You will need to take hormone medication to get your uterus ready.
- Your eggs or embryos will be thawed. If your eggs were frozen, then sperm (from your partner or a donor) will be placed into your egg to create embryos.
- You will have a procedure to place the embryo(s) into your uterus.
- If you get pregnant, you will take hormone medication for a few months to support your pregnancy.
Using donor eggs
Another option is to use eggs from a donor. While your child will not have your genes, you would experience pregnancy and childbirth.
Eggs are usually donated by people who want to help others build families. Most donors are anonymous, but some may allow a child to contact them when they reach adulthood. Donors may be willing to have contact with you during the process. Donor eggs can cost as much as $35,000.
Using donor embryos
Another option is to use embryos from a donor. While the child will not have genes from you or your partner, you would experience pregnancy and childbirth.
You can find donor embryos through your fertility center or an embryo donation agency. The cost of donor embryos is less than that of donor eggs.
Surrogacy
If you cannot carry a pregnancy after cancer treatment, you can have someone carry a pregnancy for you. This is called surrogacy. Embryos you froze before treatment, fresh embryos created with your own eggs or donated eggs, or donor embryos are transferred into the person’s uterus. They will not have any genetic relationship to the child.
Talk with a reproductive lawyer before starting this process. They will be able to tell you the surrogacy laws in your state.
You can find a surrogate (a person that carries a pregnancy for you) through a surrogacy agency. You can also find one through a reproductive lawyer who specializes in surrogacy. Surrogacy can cost up to $150,000 when finding an unrelated surrogate through an agency or lawyer.
Visit www.menhavingbabies.org for more information.
Adoption
Adoption is another way of building your family after cancer treatment. Adoptions can be domestic (the child is born in the United States) or international (the child is born and lives outside of the United States). The cost of adopting a newborn child in the United States is around $40,000 and can take 1 to 4 years. International adoptions have different policies depending on the country. Many agencies require that you don’t have cancer for a period of time before adopting a child.
Arranging an adoption
Adoptions can be arranged by adoption agencies or lawyers. Agencies may be public or private. An agency caseworker is often involved in matching the birth parents with the adoptive parents. The match is based on what the birth parents are looking for in adoptive parents and the characteristics of the child you’re hoping to adopt.
Public agencies are part of the state Department of Social Services. They usually work with children who have been taken away from their birth parents due to alleged abuse. Private agencies may handle domestic adoptions, international adoptions, or both.
Each agency has its own standards about who they will accept as adoptive parents. Children adopted through private agencies are usually younger than children adopted through public agencies. A private domestic adoption may be the best option if you want to adopt a newborn child.
Adoption lawyers can arrange private adoptions. Adoption laws vary by state. Work with a lawyer who specializes in adoption and is licensed in the state in which you want to adopt.
- To find an adoption agency, go to the National Foster Care and Adoption Directory website at www.childwelfare.gov/nfcad/. Select your state and the type of agency you’re looking for (such as public, private domestic, or private intercountry)
- To find agencies that focus on international adoption, search the Intercountry Adoption website at https://travel.state.gov/content/travel/en/Intercountry-Adoption.html
- To find an adoption lawyer, search the American Academy of Adoption and Assisted Reproduction Attorneys website at www.adoptionart.org
Adoption resources
The following resources can help you learn more about adoption:
- Adoptive Parents Committee: wwww.adoptiveparents.org
- Adoption.com: www.adoption.com
- Adoption.org: www.adoption.org
- Adoptive Families: www.adoptivefamilies.com
- Child Welfare Information Gateway: www.childwelfare.gov
- Intercountry Adoption: https://travel.state.gov/content/travel/en/Intercountry-Adoption.html
- American Academy of Adoption and Assisted Reproduction Attorneys: www.adoptionart.org
Resources to learn more about your options
Many professional organizations give information and support on all options for building a family. Search within each of their websites for specific topics.
- American Society of Reproductive Medicine, Reproductive Facts: www.reproductivefacts.org
- The International Council on Infertility Information Dissemination (INCIID): www.inciid.org
- Path2Parenthood: www.path2parenthood.org
- RESOLVE: The National Infertility Association: www.resolve.org
- Society for Assisted Reproductive Technology: www.sart.org
- University of California, San Francisco: Fertility options for transgender persons: https://transcare.ucsf.edu/guidelines/fertility
You may also find it helpful to read the book Having Children After Cancer: How to Make Informed Choices Before and After Treatment and Build the Family of Your Dreams by Gina M. Shaw.
MSK resources
MSK’s Sexual and Reproductive Medicine Program
www.mskcc.org/cancer-care/diagnosis-treatment/symptom-management/sexual-health-fertility/health/female-medicine
646-888-5076
Cancer and cancer treatments can affect your sexual health, fertility, or both. Our program can help with sexual health problems, such as premature menopause or fertility issues. We can help before, during, or after treatment. Call for more information or to make an appointment.
MSK’s Fertility Program
www.mskcc.org/cancer-care/diagnosis-treatment/symptom-management/sexual-health-fertility/fertility
This program helps you manage issues related to fertility and your cancer treatment. Ask your healthcare provider for a referral to talk with a fertility nurse specialist.

