This information explains what bursitis is. It also describes some of its common causes and symptoms, and how it can be treated.
About bursitis
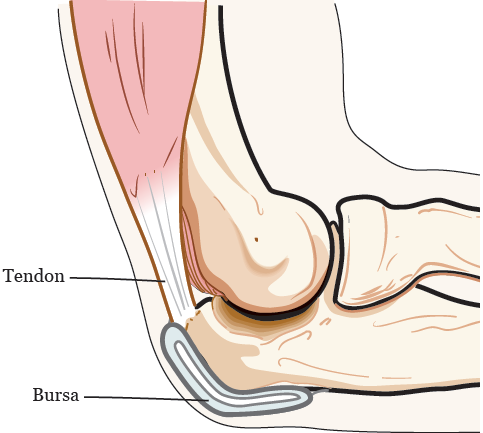
Bursitis (ber-SY-tis) is a common condition that can affect the bursa in your joint. A bursa is a small pad filled with fluid. It acts as a cushion between your bone, tendon, and the muscle near your joint (see Figure 1). There are over 150 bursae (ber-SAY) in your body.
When a bursa swells you get bursitis, which is painful. Bursitis can happen in your shoulder, elbow, hip, knee, and other joints.
Symptoms of bursitis
Common symptoms of bursitis are:
- Pain, stiffness, swelling, or discomfort around your shoulder, elbow, hip, knee, or other joints. You may feel this while you’re moving or at rest.
- Loss of movement due to pain and swelling.
Causes of bursitis
There are many causes of bursitis, such as:
- Wearing tight-fitting shoes
- Kneeling, sitting, or lying on your side for long periods of time
- Stressing or overusing a joint by bicycling, running, playing tennis, throwing a ball many times, or carrying heavy objects
- Injuries, especially falls
- Aging
- Poor posture (not sitting straight or standing tall)
-
Irritation of a bursa from:
- Joint surgery or hardware that was placed in your body during surgery, such as a hip replacement
- Bone spurs (bony growths on the edges of your bones)
- Calcium deposits (a buildup of calcium that can harden) on your tendons
- Other medical conditions, such as gout, diabetes, thyroid disease, and rheumatoid arthritis (ROO-muh-TOYD ar-THRY-tis)
Diagnosis of bursitis
Your healthcare provider can often tell if you have bursitis based on your symptoms and a physical exam. They may give you a blood test and take X-rays to rule out other possible problems.
If there are signs of infection or lots of inflammation, you may need to have an aspiration (AS-pih-RAY-shun) done. This is a procedure that uses a needle and syringe to take out some fluid from the bursa. The fluid is then tested for signs of infection or inflammation, and a treatment plan is made.
Treatment for bursitis
There are treatments that can help ease the symptoms of bursitis. The amount of time it takes for symptoms to get better or go away is different for everyone.
Your healthcare provider will make treatment recommendations based on your symptoms. The type of treatment you get depends on how long you’ve had your symptoms. It also can depend on how bad your symptoms are.
The goal of treatment is to:
- Reduce pain and inflammation.
- Keep your joints working normally.
- Stop bursitis from coming back.
Your treatment may include:
Rest
Rest your joints and avoid activities that cause pain and make your symptoms worse.
Medicine
Your healthcare provider may recommend you take nonsteroidal anti-inflammatory drugs (NSAIDs). Some NSAIDs are prescription medicines, while others are over-the-counter medicines. A prescription medicine is one you can only get with a prescription from a healthcare provider. An over-the-counter medicine is one you can buy without a prescription.
Some examples of NSAIDs are:
- Ibuprofen (Advil®, Motrin®)
- Celecoxib (Celebrex®)
- Naproxen (Aleve®, Naprosyn®)
- Diclofenac (Voltaren®)
- Mobic (Meloxicam®)
NSAIDs may cause side effects. Ask your healthcare provider if they’re safe for you to take.
Ice
Your healthcare provider may tell you to ice your joints. Apply the ice every 4 to 6 hours for 15 minutes. Do not keep the ice on for more than 15 minutes at a time.
Rehabilitation therapy
Your healthcare provider may refer you to an occupational therapist (OT) or physical therapist (PT). Your OT or PT will:
- Show you how to do exercises that will strengthen your joints.
- Tell you how to protect your joints, which helps with healing and stops bursitis from coming back.
- Perform an ultrasound, massage, or other therapies. These therapies will ease your pain, increase blood flow, and help you heal faster.
Steroid injections and fluid draining
If your pain doesn’t go away after trying other treatments, talk with your healthcare provider. They may suggest steroid injections (shots), fluid draining (aspiration), or both.
If you have fluid in your joint, your healthcare provider will drain it using a needle and syringe. This will help to reduce your pain.
If you need a steroid shot, your healthcare provider will inject a steroid into the area surrounding your joint. This will help to reduce swelling and pain. To learn more, read Steroid Injections.