This information will help you care for your wet colostomy.
About your wet colostomy
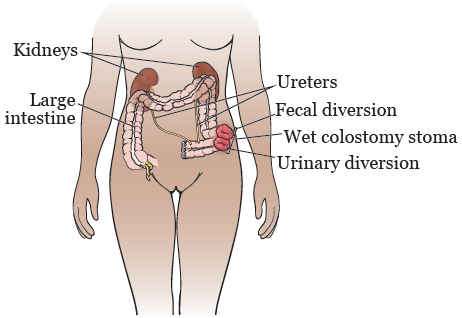
After your surgery, your urine (pee) and stool (poop) will leave your body through your wet colostomy stoma. Your stoma will have 2 parts (see Figure 1):
- A urinary diversion. Your urine will flow from your kidneys, through your ureters, and out of your body through your urinary diversion.
- A fecal diversion. Your stool will move through your large intestine (colon) and out of your body through your fecal diversion.
Your stoma should be a deep pink or red color at all times. While it’s contracting and expanding to move stool out of your body, it may look slightly paler in color (change from red to pink). This should only last for a few seconds to minutes. If your stoma looks dark maroon, grey, brown, or black, call your doctor right away.
Your stoma will slowly get smaller as it heals. This usually takes about 6 to 8 weeks after your surgery.
Learning about your wet colostomy
While you’re in the hospital, your wound, ostomy, and continence (WOC) nurse and nursing staff will teach you how to care for your wet colostomy. Your case manager will arrange for a home care nurse to visit you at home after you’re discharged from (leave) the hospital. They will also make sure you leave the hospital with enough supplies to care for your wet colostomy for the first month you’re home.
After you’re discharged, a home care nurse will help you care for your wet colostomy. At your first appointment after surgery, a WOC nurse will teach you more about caring for your wet colostomy. They will review how to:
- Empty your pouch (bag)
- Change your pouching system
- Care for your skin around your stoma
- Order supplies
If you have any questions or problems once you’re home, call your doctor’s office.
About your pouching (bag) system
After your surgery, you will wear an odor-proof pouching (bag) system over your wet colostomy. The pouching system will probably be a 2-piece system made up of a skin barrier (wafer) and a high-output collection pouch.
- The wafer sticks to your skin and is sized to fit around your stoma. It protects the skin from getting irritated by your urine and stool.
- The high-output pouch attaches to the wafer and collects your urine and stool. You will need to empty the pouch multiple times each day.
For the first 6 to 8 weeks after your surgery, you may need to change the size of your pouching system as your stoma gets smaller. Your WOC nurse and home care nurse will help you measure your stoma and find the pouching system that fits best.
While you’re getting used to your wet colostomy and pouching system, you may find it helpful to buy a waterproof mattress cover. The cover will protect your bedding and mattress if the pouching system leaks.
Emptying your pouch (bag)
While you’re in the hospital, your nurse and WOC nurse will teach you how to empty your pouch (bag). After you leave the hospital, your home care nurse will help you get more comfortable with changing it.
Empty your pouch when it’s ⅓ to ½ full. Don’t let your pouch get too full.
You will also need to empty your pouch every night before bed. You can use a night drainage bag so you don’t need to empty your pouch during the night. A night drainage bag connects to your pouching system and rests on the floor.
Changing your pouching (bag) system
Your WOC nurse will teach you how to change your pouching (bag) system. You should change your pouching system every 3 to 5 days. If your pouching system is leaking, change it right away. This is to keep urine or stool from irritating the skin around your stoma.
If you’re having leakage or irritation, call your doctor’s office to make an appointment with your WOC nurse. You may need a different pouching system that fits your stoma better.
About wearing gloves
You can decide if you want to wear gloves when you change your pouching (bag) system. Just as you didn’t wear gloves when using the bathroom before your wet colostomy, you don’t need to wear them now. You can wear gloves if you will feel more comfortable, but there’s no risk of infection if you don’t wear them.
Wash your hands before and after caring for your pouching system.
What to do if you see blood on your stoma
Your stoma has many blood vessels and may bleed easily. It’s normal to see a small amount of blood on the gauze when you’re cleaning your stoma.
If your stoma starts bleeding, apply pressure to the area that’s bleeding. It should stop on its own within a few minutes. If you take a blood thinner or aspirin, you may bleed more easily and for a longer time. Call your doctor if you bleed a lot or if the bleeding doesn’t stop after 5 to 10 minutes.
If there’s blood in your stool or coming from the inside of your stoma, call your doctor right away.
Odor control
Pouching (bag) systems are designed to be odor-proof. You shouldn’t smell anything while your pouching system is in place. If you do notice an odor, this means there’s urine or stool leaking underneath the wafer or that the outside of the pouching system is dirty.
There will be some odor when you’re emptying your pouch or changing your pouching system. There are deodorants that you can put into your pouch to help lessen the odor. The deodorants come as drops, charcoal tablets, or lubricating gels. You may need to try a few different types to find one that works best for you. Check with your doctor or nurse before using any deodorants in your pouch. You can also buy a deodorant spray to help freshen the air after you empty your pouch.
Ordering ostomy supplies
Talk with your WOC nurse about ordering supplies. Your WOC nurse is familiar with the latest products on the market. You can also call companies and ask for samples of their products. You may want to wait to do this until you’re comfortable with caring for your stoma. Too many options may get overwhelming.
Mail-order medical supply companies
Mail-order supply companies will mail your supplies to you every month. Choose a company that accepts your insurance. You can call the company directly to find out. If they don’t accept your insurance, call your insurance company to get a list of suppliers that do.
The company you’re ordering from will contact your doctor’s office to get a prescription for your supplies. It’s important for you to give your doctor’s office a clear and complete list of the supplies you need, including the product numbers, so they can send a correct prescription to the supply company.
Below is a list of some mail-order medical supply companies. These companies offer many different products. You can call and ask them to send you a catalog, or you can view one online.
| Byram Healthcare 877-902-9726 www.byramhealthcare.com | Liberator Medical 877-649-7359 www.liberatormedical.com |
| CCS Medical 800-722-2604 www.ccsmed.com | McKesson Medical-Surgical 800-453-5180 www.mckesson.com |
| Edgepark Medical Supplies 888-394-5375 www.edgepark.com | 180 Medical (ConvaTec supplies only) 877-688-2729 www.180medical.com |
You can also buy ostomy supplies at your local pharmacy or medical supply store. However, the prices may be higher, or they may not take your insurance. Also, they may not be able to get the exact product you need.
Ostomy product manufacturers
If you have questions about your supplies, you can call an ostomy product manufacturer. Many of these companies have a WOC nurse on staff to answer questions. You can also call to ask for samples of products.
Below is a list of some companies that make ostomy products (such as wafers and pouches) and other ostomy accessories (such as barrier strips, powders, and rings).
| Coloplast 888-726-7872 www.coloplast.us | Hollister 888-740-8999 www.hollister.com |
| ConvaTec 800-422-8811 www.convatec.com | Marlen 216-292-7060 www.marlenmfg.com |
| Cymed 800-582-0707 www.cymed-ostomy.com | Nu-Hope Laboratories, Inc. 800-899-5017 www.nu-hope.com |
Lifestyle issues
Staying hydrated
It’s important to drink 8 to 10 (8-ounce) glasses of liquids every day. This will help you stay hydrated, keep your kidneys healthy, and keep urine flowing. Limit the amount of caffeine and alcohol you drink, because these things can make you dehydrated.
If you get diarrhea (loose or watery bowel movements), call your doctor’s office. Make sure to drink extra liquids so you don’t get dehydrated. You should also call your doctor’s office if you feel nauseous (like you’re going to throw up) or weak.
Nutrition
Your appetite may be smaller than it was before your surgery. You will probably be able to eat the same foods you did before your surgery. Foods that upset your stomach before your surgery may still upset your stomach after your surgery. If you feel bloating and pain after eating a certain food, remove it from your diet. Try eating it again in a few weeks. If you’re still having discomfort and bloating after eating this food, avoid it.
Now that you have a wet colostomy, you won’t be able to control when you pass gas. You may want to avoid things that increase gas, such as:
- Cruciferous vegetables (such as cabbage and broccoli)
- Carbonated drinks
- Drinking through a straw
- Chewing gum
If you have tried avoiding these things but have a problem with gas, talk with your WOC nurse or a clinical dietitian nutritionist.
If you’re having problems with gas building up inside your pouch (bag), talk with your WOC nurse. They may suggest using pouches with charcoal filters. The filter can help keep gas from building up and inflating your pouch. You may also find it useful to use a pouch with a filter when you travel on an airplane, because the altitude changes may cause air pressure to build up inside your pouch.
If you’re constipated (having fewer bowel movements than usual):
- Drink more liquids.
- Eat foods that are high in fiber, such as fruits, vegetables, and bran.
- Exercise, if you can. Walking is an excellent form of exercise.
Exercise
Talk with your doctor about what exercise is right for you. For most people, walking and light stretching are good exercises to do while recovering from surgery. Avoid lifting or pushing anything heavier than 10 pounds (4.5 kilograms) for 2 to 3 months after your surgery. This includes housework such as vacuuming or mowing the lawn. If this will be a problem for you, talk with your doctor.
Don’t do sit-ups, push-ups, or any strenuous exercise for 2 to 3 months after your surgery. This will help prevent a hernia (bulging of your intestines through a weakened abdominal muscle) near or around your stoma.
Your WOC nurse can measure you for a hernia belt to wear while you exercise. Your nurse will also tell you how you can order one.
Showering, bathing, and swimming
Your colostomy pouching (bag) system is waterproof. Always wear your pouching system when you take a bath or swim. You can use waterproof tape around the edges of the wafer or adhesive strips to help keep a tight seal around your pouching system, if needed. Most people can wear the same swimsuit they wore before their surgery. Some companies sell swim wraps or bathing suits to cover the pouching system.
You can shower with or without your pouching system. If you shower without your pouching system, urine, stool, or both may leak out of your stoma and you will need to clean the shower area afterward.
Positioning your pouch (bag)
You can position your pouch (bag) downward or to the side. You can also fold it, if you prefer.
Wearing a belt
Try to wear the belt above or below your stoma. If the belt is worn directly on your stoma, it can cause irritation, bleeding, or an overgrowth of tissue. There are stoma guards that help protect your stoma from being injured by your belt. If you’d like to order a stoma guard, ask your WOC nurse for more information.
Going back to work
You can go back to work when you and your doctor feel you have recovered and are able to work.
You may feel uncomfortable going back to work. This is okay. Your pouching (bag) system probably won’t be visible. You will probably be able to wear most of the same clothes you wore before your surgery.
You can choose if you want to tell your coworkers, friends, or family about your wet colostomy. Usually, people won’t know you have a wet colostomy unless you tell them.
Traveling
Some people are nervous the first few times they travel. If you feel anxious, it may help to look up the locations of some bathrooms on your route.
Always carry 2 sets of extra supplies with you wherever you go, even if it’s only a short trip or a doctor’s appointment. This way, you will be prepared in case you have an accident while away from home. Remember to bring:
- Pouches (bags)
- Wafers
- Clamps (if you have a pouching system with a clamp closure)
- Cleaning items such as paper towels, gauze, or wipes
- Adhesive remover wipes and skin prep wipes
- A trash bag for dirty items
If you’re going to be away from home for several hours, think about where you’re going and prepare yourself in case you need to empty your pouch while you’re out of the house.
When you’re traveling on an airplane:
- Pack your ostomy supplies in at least 2 places, such as in your carry-on and checked luggage.
- Take extra supplies in case you’re stranded where supplies aren’t available.
- You may want to precut your pouches at home and pack them already cut into your travel bag.
You may want to bring a letter from your doctor that says that you have an ostomy and need ostomy supplies. The letter should also ask transportation security administration (TSA) staff members to use a private area if they need to do an extended search. You may also want to carry copies of the catalog pages that show and explain your equipment.
If you’re traveling to a foreign country, it’s a good idea to have important ostomy information written in that language. One of the 70 members of the International Ostomy Association may be able to help with this translation and with finding supplies while visiting their country. For more information, visit www.ostomyinternational.org.
The United Ostomy Association of America web site (www.uoaa.org) has more information and travel tips that you can print and use.
About parastomal hernias
If the area around your stoma seems to bulge, you may have a hernia. A hernia is when a loop of bowel (intestine) pokes through a weak area of muscle. This causes a bulge to form. A hernia that’s near a stoma is called a parastomal hernia. If you see a bulge around your stoma, contact your doctor or WOC nurse.
Hernias can feel tender, uncomfortable, like pressure, or like something is hanging. Sometimes, hernias can become twisted or blocked and need to be treated.
If your hernia is causing pain or any other symptoms, call your doctor’s office. You should also call your doctor’s office if you have:
- Nausea (feeling like you’re going to throw up) or vomiting (throwing up)
- Pain in your abdomen (belly)
- Bloating in your abdomen and no gas or stool in your pouch (bag)
If you have a parastomal hernia, your WOC nurse can suggest a hernia support belt. You can also use a girdle, specially made spandex clothes, or biking shorts to support the hernia. If you use biking shorts, you will need to cut out a hole for your pouch. Talk with your WOC nurse about what will work best for your needs.
Using a hernia support belt, girdle, or biking shorts won’t cure the hernia, but they may keep the hernia from getting worse. They can also make you feel more comfortable and pull in the bulge to help your clothes fit better.
About Urinary Tract Infections (UTIs)
The signs and symptoms of a UTI are:
- Cloudy urine
- Back pain
- Nausea and vomiting
- Loss of appetite
- Fever of 100.4 °F (38 °C) or higher
If you think you have a UTI, call your doctor’s office.
To keep from getting a UTI:
- Drink 6 to 8 (8-ounce) glasses of liquids every day. It’s best to drink water.
- Limit the amount of alcohol and caffeine you drink.
- Use a night drainage system overnight, if possible. This keeps urine from sitting on your stoma and causing an infection.
- Empty your pouch (bag) when it’s ⅓ to ½ full.
What to do before medical tests
Always bring an extra set of supplies when going to the doctor for tests. You may need to remove your pouching (bag) system for the test.
If you live an hour or more away from the hospital, empty your bag before leaving. You may also need to change or empty your bag or use a leg bag on the trip home. You may also want to keep a urinal or other container in your car in case of an emergency.
Imaging scan with contrast
If you’re having a scan with contrast, bring an extra pouch (bag) and wafer, including an extra leg bag or night bag (if you use one). For the scan, you will need to drink more liquids than usual. This will help the contrast leave your body, but it will also increase your urine output. You may need the extra pouch and wafer if you have a leak because of increased urine output.
Chemotherapy
If you’re having chemotherapy, bring an extra pouch (bag) and wafer, including an extra leg bag or night bag. Chemotherapy may cause your body to make more urine. Using a leg bag or night drainage bag during treatment may help prevent leakage due to increased urine output.
Chemotherapy may also make your skin more sensitive or change the way the wafer sticks to your skin. Schedule an appointment with your WOC nurse if you notice changes to the skin around your stoma or have issues with your pouching system while you’re getting chemotherapy.
What to do before being admitted to the hospital
If you’re admitted to the hospital, you may want to bring 1 or 2 extra sets of supplies with you. The hospital may have a different product than the one you use, or they may not have any supplies at all.
Contact your healthcare provider if:
- Your stoma looks dark maroon, grey, brown, or black.
- Your stoma bleeds for longer than 5 to 10 minutes.
- There’s blood coming from the inside of your stoma.
- There’s blood in your stool.
- You’re having problems with your pouching (bag) system leaking.
- The skin around your stoma is irritated.
- You have diarrhea.
- You feel nauseous or weak.
