This information will help you understand mouth cancer, including what it is and how to treat it.
About your mouth (oral cavity)
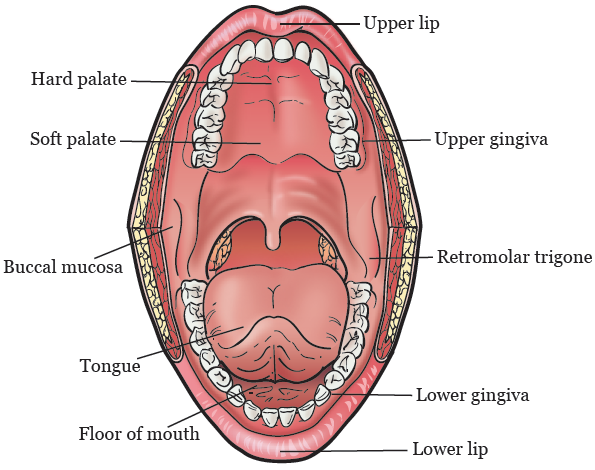
Your mouth helps you speak, chew, swallow, and breathe. Your mouth includes:
- Your lips.
- The front ⅔ of your tongue.
- The roof of your mouth. This is called your hard and soft palate.
- The floor of your mouth. This is under your tongue.
- The lining of the inside of your cheeks. This is called your buccal mucosa (BUH-kul myoo-KOH-suh).
- Your gums, which are also called your gingiva (JIN-jih-vuh).
- The small area behind your wisdom teeth in your lower jaw. This is called your retromolar trigone (reh-troh-MOH-ler TRY-gone).
Risk factors for mouth cancer
Some risk factors can make people more likely to get mouth cancer. They include:
- Tobacco use. People who smoke cigarettes, cigars, or pipes, or chew or dip tobacco have a higher risk for mouth cancer.
- Alcohol use. People who drink alcohol have a higher risk of mouth cancer. People who both drink alcohol and use tobacco have an even higher risk for mouth cancer.
- Sun exposure without sunscreen. Spending a lot of time in the sun without wearing sunscreen can cause skin cancer of your lip(s).
- Age. People ages 65 to 74 are at higher risk for mouth cancer. This is because of their longer exposure to other risk factors.
Call 212-610-0507 to talk with a Tobacco Treatment Specialist.
If you use tobacco or alcohol, you’re at higher risk for mouth cancers. If you would like help, talk with your healthcare provider.
MSK has specialists who can help you quit smoking or smoke less. For more information about our Tobacco Treatment Program, call 212-610-0507.
Visit www.mskcc.org/cancer-care/types/mouth for more information about mouth cancer.
Signs and symptoms of mouth cancer
The following changes in and around your mouth could be signs of cancer. They also can be caused by other things. Talk with your healthcare provider if you have any of the following:
- A sore, lump, or thick or hard area on your lip or in your mouth that does not heal.
- A white or red patch on your gums, tongue, or in the lining of your mouth.
- An infection in your mouth that does not get better within 1 month after treatment.
- Loose teeth or dentures that no longer fit well.
- Chronic (long-lasting) pain in your mouth or throat.
- Bleeding or numbness in your lip or mouth.
How we diagnose mouth cancer
Here are some ways that mouth cancer is diagnosed.
Biopsy
A biopsy is a procedure done to take samples of tissue or cells to check for cancer. During a biopsy, your doctor removes a small amount of cells or tissue for a pathologist to examine.
A pathologist is a doctor who uses a microscope to make a diagnosis. The pathologist will examine your tissue sample under a microscope to look for cancer cells. The biopsy results usually take at least 5 days to come back.
If you have not had a biopsy, you may have one during your first visit at MSK. If you already had a biopsy, an MSK pathologist will check your tissue samples.
Imaging scans
You may also have imaging scans. Some examples are a computed tomography (CT) scan, magnetic resonance imaging (MRI), or Panorex X-ray. A Panorex X-ray shows your full upper and lower jaw, including your sinuses. These scans give more details about the lesion (area of diseased or damaged tissue).
Visit www.mskcc.org/cancer-care/types/mouth/mouth-cancer-diagnosis for more information about diagnosing mouth cancer.
Mouth cancer surgery
Your doctor may recommend surgery if your results and exam show you have mouth cancer. Surgery is the most common treatment for pre-cancerous lesions and early cancers.
Pre-cancerous lesions are lesions that have not yet become cancer. Early cancers are lesions that are cancer but have not spread. Your doctor may decide to remove any pre-cancerous lesions to keep them from turning into cancer.
These are the goals of treatment for mouth cancer:
- Cure the cancer.
- Keep the way you look and how your mouth works.
- Prevent the cancer from spreading.
The type of surgery you need depends on the lesion’s location. Your healthcare provider will tell you which area is affected. The following sections explain the different types of surgeries, based on where the lesion is. Visit www.mskcc.org/cancer-care/types/mouth/mouth-cancer-treatment/mouth-cancer-surgery for more information about mouth cancer surgery.
You will get anesthesia (medication to make you sleep) before your surgery. All these surgeries are done through your open mouth.
Lip surgery
Your doctor will recommend surgery to remove a lesion on around your lip. During this surgery, your doctor will remove the lesion and the skin around it. The incision (surgical cut) will be closed with sutures (stitches).
The sutures will be inside your mouth and on your lip. They will dissolve (break down and fall out) on their own. On your skin, they will use a different type of suture that does not dissolve. You will have a follow-up appointment to remove them.
Tongue surgery
Your doctor will recommend surgery to remove a lesion on your tongue. How much they remove depends on the size of the lesion. A surgery to remove part of your tongue is called a partial glossectomy (glah-SEK-toh-mee).
The incision may be closed with sutures that dissolve. Your doctor may use a graft of man-made (synthetic) skin to cover the area. This graft will be sewn in with sutures that dissolve and fall out in a few weeks.
Hard palate and upper gum surgery
Your doctor will recommend surgery to remove a lesion on your hard palate and upper gum. What is removed during surgery depends on the lesion’s size and how deep it is.
Small lesions on the surface (called superficial tumors) will be removed and closed with sutures, a skin graft, or a local flap. A skin graft or flap is tissue that’s taken from one part of your body. It’s moved to the area that must be covered. New tissue will grow over and heal the opening.
If you have a larger and deeper lesion, part of your palate may need to be removed. After surgery, the area will be covered with a graft of skin or synthetic skin.
If your doctor uses a skin graft, they will cover it with gauze. It will be held in place with a dental plate. The dental plate will be made by your dentist at MSK. They will see you before your surgery. Your doctor will remove the gauze and dental plate 5 to 7 days after surgery.
If your doctor uses synthetic skin, they will sew it in with sutures that dissolve. The sutures will fall out in a few weeks.
Soft palate surgery
Your doctor will recommend surgery to remove a lesion on your soft palate. The incision will be closed with sutures that dissolve, or a skin graft. If your doctor uses a skin graft, they will cover it with gauze and hold it in place with sutures. Your doctor will remove the sutures at your follow-up appointment.
Floor of the mouth
Your doctor will recommend surgery to remove a lesion on the floor of your mouth. How much they remove depends on the lesion’s size and how deep it is. Your lesion will be removed and closed with sutures, a local flap, or a skin graft.
Larger lesions will be removed and covered with a graft of skin or synthetic skin. If your doctor uses a skin graft, they will cover it with gauze and hold it in place with sutures. Your doctor will remove the gauze 5 to 7 days after surgery.
If your doctor uses synthetic skin, they will sew it in with sutures that dissolve. The sutures will fall out in a few weeks.
Lining of the cheek
Your doctor will recommend surgery to remove a lesion on the lining of your cheek. The incision will be closed using a skin graft or synthetic skin.
If your doctor uses a skin graft, they will cover it with gauze and use sutures to hold it in place. Your doctor will remove the gauze 5 to 7 days after surgery.
If your doctor uses synthetic skin, they will sew it in with sutures that dissolve. The sutures will fall out in a few weeks.
Lower gums and area behind your wisdom teeth in your lower jaw
Your doctor will recommend surgery to remove a lesion on your lower gums or behind your wisdom teeth in your lower jaw. If your lesion is deep, your doctor may also remove a small piece of your jawbone (mandible). Surgery to remove a small part of your mandible is called a marginal mandibulectomy.
The incision will be covered with a skin graft or synthetic skin. If your doctor uses a skin graft, they will cover it with gauze and hold it in place with sutures. Your doctor will remove the gauze 5 to 7 days after surgery.
If your doctor uses synthetic skin, they will sew it in with sutures that dissolve. The sutures will fall out in a few weeks. Your jawbone will not need to be reconstructed. The shape of your jaw will not be affected.
How to take care of yourself after mouth cancer surgery
Diet changes after mouth cancer surgery
You can drink liquids right after your surgery. Your doctor will let you know when it’s OK for you to start eating pureed foods. You can begin to eat soft foods when your doctor tells you it’s OK.
You can also drink liquid supplements that are high in protein and calories. Examples are Ensure®, Boost®, and Carnation Instant Breakfast®.
Do not eat regular, solid foods until your doctor says it’s OK.
You may have had surgery of the lining of your mouth or lower gums. If so, do not chew on the side of your mouth where you had surgery. Your doctor will tell you when you can eat normally at your follow-up appointment.
How to take care of your mouth after mouth cancer surgery
- Your doctor will tell you if it’s OK to brush your teeth after surgery.
- Keep your mouth clean by rinsing or using an oral irrigation set. Your nurse will give you an oral irrigation set and teach you how to use it.
-
Do not use mouthwash with alcohol in it. It can irritate your mouth and slow down healing. Instead, make a rinsing solution. To do this, mix:
- 1 quart of warm water
- 1 teaspoon of salt
- 1 teaspoon of baking soda
- Rinse your mouth at least 4 times a day. Rinse after each meal or snack. Continue to rinse until your surgical site is healed. Your doctor will tell you when to stop.
How to take care of your mouth surgery incision
- Keep the sutures on your lip or neck dry for the first 48 hours (2 days). After 48 hours, you can shower as usual. Do not put direct water pressure on your incision. Instead, let the water run over your incision and use a clean towel to pat your incision dry.
- Your dissolvable sutures will loosen and fall off around 6 to 8 weeks after surgery. When you feel them in your mouth, you can spit them out. There is no special care needed while they’re in place, other than keeping your mouth clean.
- We will remove sutures that do not dissolve at your first visit with your doctor after surgery.
- If you had surgery on your lip, do not stretch out your lip until the area is fully healed. For example, try not to laugh or smile.
Speech changes after mouth cancer
- If you had surgery on your tongue, floor of mouth, or soft palate, you may talk differently. Your tongue may feel swollen and numb and may not move freely. This will get better as the area heals.
- If you have significant speech changes (such as having trouble saying words or people can’t understand you), your doctor will refer you to a speech therapist for help. Visit www.mskcc.org/cancer-care/diagnosis-treatment/symptom-management/rehabilitation/speech-hearing for more information about speech therapy.
How to manage your pain after mouth cancer
- Most people have some pain or discomfort after surgery. You will get a prescription for pain medication before you go home. Take it as prescribed.
- If the pain medication does not help you, call your doctor’s office.
- Pain medication can cause constipation (having fewer bowel movements than what’s normal for you). To prevent this, take a stool softener such as docusate sodium (Colace®) 3 times a day. If this doesn’t help, take a laxative (such as 2 tablets of Senokot®) at bedtime.
You can get both at your local pharmacy without a prescription. If you still have constipation after using these medications, call your doctor’s office. For more information, read Managing Constipation.
Schedule your mouth cancer follow-up visit
The day after your surgery, call your doctor’s office to schedule a follow-up appointment.
When to call your healthcare provider
Call your healthcare provider if you have any of the following:
- A fever of 100.4° F (38.0° C) or higher.
- Increased discomfort, redness, or swelling around your incision.
- Discharge or pus coming from your incision.
- Any questions or concerns.