This information explains eating and drinking guidelines you must follow before and after your gastrectomy. This is surgery to remove part or all of your stomach.
Your clinical dietitian nutritionist will review this information with you. If you have any questions about your diet before or after surgery, call 212-639-7312. You can set up an appointment with a clinical dietitian nutritionist.
While you’re in the hospital, a clinical dietitian nutritionist will visit you. Follow-up care after surgery may be helpful, depending on the part of your stomach that was removed. Your care team will talk with you about this.
Diet and nutrition before surgery
It’s important to get enough nutrition before and after surgery. Getting enough nutrition can help you:
- Prevent nutrition deficiencies, which means you do not have some things you need. For example, you may not be getting enough vitamins from the foods you eat.
- Stay strong.
- Maintain your weight.
- Fight infection.
- Have fewer side effects.
- Heal after surgery.
High-calorie, high-protein foods
Eat foods listed in this table to add more calories and protein to your diet. Ask your clinical dietitian nutritionist for more menu ideas if you need them.
| Food group | Food | Calories | Protein (grams) |
|---|---|---|---|
| Meat, beans, and eggs | 1 cup cooked dried beans | 240 | 4 |
| ½ cup chicken salad | 200 | 14 | |
| 1 large egg cooked with 1 tablespoon butter | 175 | 7 | |
| 3 ounces tuna canned in oil | 170 | 25 | |
| ¼ cup egg substitute | 25 | 5 | |
| Nut butters | 1 tablespoon of full fat peanut butter | 95 | 4 |
| 1 tablespoon of almond butter | 100 | 3 | |
| Dairy | ½ cup canned evaporated milk (can be used instead of water when cooking) | 160 | 8 |
| 7 ounces of 2% Greek yogurt | 140 | 20 | |
| 7 ounces of 5% Greek yogurt | 190 | 18 | |
| ½ cup premium ice cream | 220 | 14 | |
| ½ cup full fat creamed cottage cheese | 115 | 7 | |
| ¼ cup (1 ounce) shredded cheese | 100 | 7 | |
| ¼ cup half-and-half | 80 | 2 | |
| ½ cup whole milk (can be used instead of water when cooking) | 75 | 7 | |
| 1 tablespoon cream cheese | 50 | 1 | |
| 2 tablespoons sour cream | 50 | 1 | |
| Fats | 1 tablespoon butter, margarine, oil, or mayonnaise | 100 | 0 |
| 2 tablespoons gravy | 40 | 1 | |
| Sweets | 1 tablespoon honey | 60 | 0 |
| 1 tablespoon sugar, jam, jelly, or chocolate syrup | 50 | 0 | |
| Meal replacements | 1 meal replacement bar | 200 | 15 |
| 1 scoop (1 ounce) protein powder | 100 | 15 |
High-calorie, high-protein liquid nutritional supplements
Your care team may suggest taking nutritional supplements high in calories or protein. If they do, take the supplements between meals. If you take them with a meal, they can be filling. That keeps you from eating more of your food.
We list some examples of liquid nutritional supplements in the table below. You can buy most of them at any supermarket or pharmacy. If the store does not have a product, ask a pharmacist or store manager to order it for you. You can also order these products online.
Some supplements may cause diarrhea (loose bowel movements), gas, or bloating. Try supplements in small amounts to see how they affect you. If you have any of these side effects, try a low sugar supplement. You can also talk with your clinical dietitian nutritionist about other options.
| Nutritional supplement and serving size | Calories | Protein (grams) | Lactose free? |
|---|---|---|---|
| Ensure® Original (8 ounces) | 225 | 9 | Yes |
| Boost® Original (8 ounces) | 240 | 10 | Yes |
| Ensure® Plus (8 ounces) | 350 | 13 | Yes |
| Boost® Plus (8 ounces) | 360 | 14 | Yes |
| Boost® VHC (Very High Calorie) (8 ounces) | 530 | 22 | Yes |
| Ensure® High Protein (8 ounces) | 160 | 16 | Yes |
| Boost® High Protein (8 ounces) | 240 | 20 | Yes |
| Ensure® Compact (4 ounces) | 220 | 9 | Yes |
| Boost® Compact (4 ounces) | 240 | 10 | Yes |
| Glucerna® Shake (8 ounces) (For people with diabetes) | 180 | 10 | Yes |
| Ensure® Clear (8 ounces) | 250 | 9 | Yes |
| Boost® Breeze (8 ounces) | 250 | 9 | Yes |
| Carnation Breakfast Essentials® Powder (8 ounces) (Made with whole milk or lactose-free milk) | 280 | 12 | No |
| Nepro® Nutritional Shake (8 ounces) (For people with kidney disease) | 425 | 19 | Yes |
| Orgain® Nutritional Shake (11 ounces) (Organic, plant-based) | 255 | 16 | No |
| Premier Protein Shakes (8 ounces) | 160 | 30 | No |
| Kate Farms® Nutritional Shakes (11 ounces) | 330 | 16 | Yes |
| Benecalorie® (1.5 ounces) | 330 | 7 | Yes |
High-calorie, high-protein nutritional shakes
You can also make your own nutritional shakes that are high in calories and protein. For shake recipes and other tips for having more calories and protein, read Eating Well During Your Cancer Treatment.
Tips for eating more food
If you’re not eating enough or are losing weight, these tips can help you get the most from your meals.
-
Eat small meals and eat more often.
- Have a half-sized meal every 2 to 3 hours.
- Try to eat 6 to 8 small meals a day instead of 3 large meals.
- Make and follow a meal schedule. Do not wait until you’re hungry.
- Serve smaller food portions on salad plates instead of dinner plates.
- Keep your favorite foods in your home where you can get to them easily.
- Buy single-serving food items that you can eat easily. Try small bags of mixed nuts or trail mix.
-
Cook in batches so you have leftovers.
- Keep 1 extra serving in your refrigerator for the next day, but not longer.
- Freeze the other extra servings. When you’re ready to use a serving, thaw it in the refrigerator or microwave. Do not thaw on the kitchen counter. Then, reheat it until it’s steaming hot.
- Include many kinds of food groups and food types in your diet, unless your healthcare provider tells you not to.
- Get more calories from liquids than solid foods. For example, have milkshakes or nutritional supplements such as Ensure or Carnation Breakfast Essentials.
- Make dining a good experience. Eat your meals in a pleasant, relaxing setting with family or friends.
- Think of your nutrition as being just as important as your medicine.
Diet and nutrition after surgery
After your gastrectomy, the way you digest food will change. You may digest your food too fast and not absorb nutrients as well as before. That’s why you may need to change the way you eat.
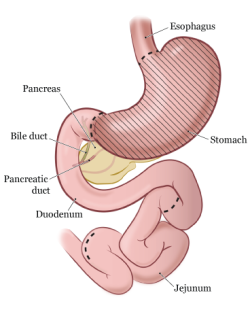
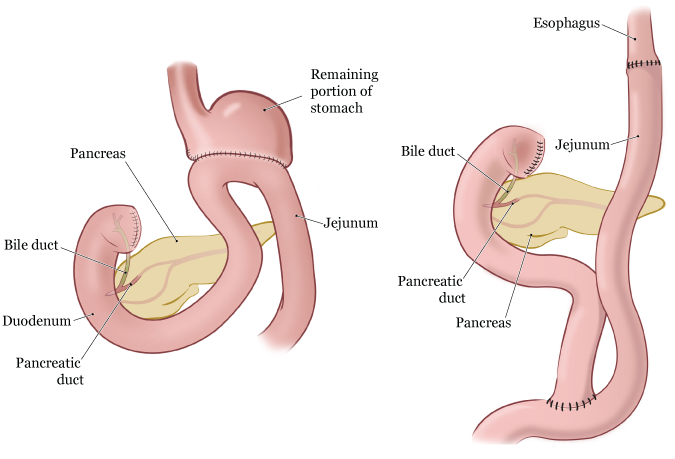
- If you have a subtotal gastrectomy, some of your stomach will be removed. You will have a smaller stomach (see Figure 2).
- If you have a total gastrectomy, your whole stomach will be removed (see Figure 3). This means you will feel full faster than you did before surgery.
Follow the guidelines in this section. You can also use the sample menus at the end of this resource to plan your meals.
Guidelines for eating after your gastrectomy
Eat smaller meals more often
After your surgery, your stomach will not be able to hold as much as it did before surgery. You will need to have 6 or more small meals a day instead of 3 main meals. This will help you eat the right amount of food.
Do not wait until you feel hungry. Create and follow a meal schedule. Have your last meal of the day at least 2 hours before bedtime. Tell your care team if you’re losing weight without meaning to.
After surgery, you may only be comfortable eating a few bites of food at a time. After a few months, you may be able to have larger meals and eat less often.
If all of your stomach was removed, you only may be able to have a few bites of food during each meal. You may need to eat or drink every 1 to 2 hours to get all the nutrients you need.
Eat slowly and chew your food well
Eat slowly to stop you from getting too full and feeling uncomfortable. Sit upright during your meals. Chew food into very small pieces. This makes it easier for your body to digest the food.
Limit the amount of liquids you have with meals
Do not have more than 4 ounces (½ cup) of liquid with your meals. This will help you eat enough solid food without getting too full. It will also keep food from moving into your small intestine too fast. It’s OK to take extra sips of liquids if your mouth feels dry or you’re coughing.
Remember that soup and protein shakes count as liquids.
Eat protein with each meal
After surgery, your body needs more protein to help you heal. Eat protein with each meal. Good sources of protein include:
- Meat
- Chicken or turkey
- Fish
- Low-fat dairy products, such as milk, yogurt, and cheese
- Eggs
- Tofu
- Nuts and nut butters
Choose foods that are easy to eat
- Choose soft, well-cooked foods. Avoid raw vegetables and tough or chewy foods like red meats or bagels.
- Avoid spicy and peppery foods soon after your surgery. They may cause discomfort.
- Avoid fatty and sugary foods if they cause discomfort. Read the “Food intolerances after surgery” section of this resource.
Guidelines for drinking after your gastrectomy
- Drink about 8 to 10 (8-ounce) glasses of liquid each day.
- Avoid carbonated (fizzy) drinks, such as soda and seltzer, if they make you feel full.
- Drink most of your liquids at least 1 hour before or 1 hour after your meals. This helps avoid feeling too full and prevents dehydration (when you do not drink enough liquids).
- Do not have more than about 4 ounces (½ cup) of liquids with your meals.
Vitamin and mineral supplements after surgery
If a large part of your stomach was removed, you may need to take extra vitamin B12. You can get vitamin B12 as an oral supplement (such as a pill) or a monthly shot.
You may also need other vitamin and mineral supplements. If you do, your care team will talk with you about this.
Food intolerances after surgery
A food intolerance is when you have discomfort or unpleasant symptoms after having certain foods or drinks. After your surgery, you may have food intolerances you did not have before.
This section explains some possible intolerances you may have. You will only need to follow the tips in this section if you have these symptoms.
Sugar intolerance
Some people have cramping, stomach pain, or diarrhea within 20 minutes of eating foods or drinks that have a lot of sugar. This is called dumping syndrome. Dumping syndrome can also be caused by eating too much at once.
Symptoms can happen 1 to 2 hours after eating a sugary meal. Some people feel weak, hungry, nauseous (like you’re going to throw up), anxious, shaky, or sweaty.
This happens because your body releases extra insulin after you eat large amounts of sugar. Having too much insulin in your bloodstream causes low blood sugar.
We can control dumping syndrome and low blood sugar by changing your diet. Avoid foods and drinks with lots of sugar, such as:
- Sugar-sweetened sodas
- Fruit juices
- Candy
- Cane sugar
- Honey
- Syrups
- Cakes and cookies
It’s OK to eat small amounts of cakes, cookies, and candies sweetened with sugar alcohols (such as sorbitol and mannitol). Eating too much can cause diarrhea.
Eating smaller meals and having protein with meals may also help with symptoms. So will eating foods with soluble fiber, such as canned fruits, bananas, peanut butter, and oatmeal.
Fat intolerance
Some people have trouble digesting large amounts of fat after surgery. You may not be absorbing all the fats you’re eating if you’re having any of these symptoms:
- Bowel movements very often
- Bowel movements that float
- Bowel movements that are very light in color, frothy, greasy, or foul smelling
If you have any of these symptoms, talk with your care team. You may need a medicine to help you digest fats.
Try having small amounts of fats at first. Then, slowly add a higher amount to your diet. Foods high in fat include:
- Butter, margarine, and oils
- Mayonnaise
- Creamy salad dressings
- Cream cheese
- Gravies
- Potato chips and corn chips
- Rich desserts
- Fried foods
- Fatty meats
Lactose (dairy) intolerance
Lactose intolerance is not being able to digest lactose. Lactose is a type of sugar found in dairy or milk products. Some people have trouble digesting lactose after having a gastrectomy.
Symptoms of lactose intolerance include gas, bloating, and diarrhea. These symptoms can happen 30 minutes to 2 hours after having dairy products.
After surgery, slowly bring dairy products back into your diet. Milk, ice cream, and soft cheeses have high amounts of lactose. Hard cheeses, yogurt, and butter have smaller amounts of lactose.
To test your tolerance to dairy foods, start by drinking a 4-ounce (½ cup) serving of milk.
- If you do not have any symptoms of lactose intolerance, you can start eating more dairy foods.
- If you have symptoms, you may still be able to eat foods with smaller amounts of lactose. Pay attention to how you feel after having different types of dairy. Pay attention to how you feel after eating dairy products along with other non-dairy foods.
If you think you may be lactose intolerant:
- Try using a product to help you digest dairy. Examples are lactase (Lactaid®) tablets or drops.
- Try dairy products processed to remove the lactose from them (such as Lactaid milk, cottage cheese, and ice cream).
- Ask your clinical dietitian nutritionist for help, if needed.
Sometimes, lactose intolerance after surgery will go away. You can try having dairy again in a couple of months to see if you still have symptoms.
Tips for managing common problems after surgery
This section explains common problems after a gastrectomy. Keep a food log and write down any symptoms or problems you have. This can help you learn why the problems are happening. You can use the blank daily food and drink log at the end of this resource.
If the tips in this section do not help, talk with your clinical dietitian nutritionist or doctor.
Tips for managing nausea
- Avoid foods that are rich, spicy, or greasy.
- Eat slowly. Try putting your fork down between bites.
- Chew your foods well. Avoid activity right after meals. These things help with digestion.
- Do not have too much to eat or drink at one time.
- Do not lie flat after meals. Wait 2 to 3 hours before lying down.
Tips for managing fullness
- Do not eat or drink too much at one time. Eat small meals.
-
Make a schedule with times for eating and drinking. This can help if you’re having trouble having 6 smaller meals instead of 3 large meals. Setting alarms throughout the day can be helpful reminders.
- You may find yourself going back to the larger portions you had before your surgery. Try making small meals or meals in the right portion ahead of time.
- Drink most of your liquids before or after meals. Drinking during your meals can make you feel full faster.
- Eat slowly. Try putting your fork down between bites. It takes 20 minutes for your brain to know you’re full.
- Avoid carbonated drinks.
- Avoid vegetables that may make you gassy. Examples are broccoli, cauliflower, cabbage, onion, brussels sprouts, and beans.
Tips for managing diarrhea
- First, try eating less sugar. Then, try less dairy. Finally, try less fat. Pay attention to see if the diarrhea gets better. If it does, eat less of those foods.
- Avoid sugar alcohols, such as sorbitol and mannitol. These are often used in gum, hard candies, cough drops, dairy desserts, frosting, cakes, and cookies. You can see if a product has these things by checking the ingredients list. It’s OK to use other sugar substitutes such as NutraSweet or Equal.
- Avoid eating large amounts of high insoluble fiber foods, such as raw vegetables, raw fruits, and salads.
- Try eating foods with soluble fiber, such as canned fruits, bananas, peanut butter, and oatmeal.
-
Make sure you’re storing foods safely.
- Put leftovers in the refrigerator or freezer right away.
- Throw away refrigerated leftovers after 2 days.
- Throw away frozen leftovers after 6 months.
- Thaw frozen leftovers in the refrigerator or microwave, not on the kitchen counter. Reheat them to safe food temperatures until they’re steaming hot.
Tips for managing reflux
Reflux is when foods or liquids that you swallow come back up your throat into your mouth. This happens because the valve between your esophagus and stomach was removed during your surgery.
Follow these tips for managing reflux:
- Sit up straight during meals and for at least 60 minutes after you’re finished.
- Wear loose-fitting clothes around your abdomen (belly).
- Eat your last meal of the day at least 2 hours before your bedtime.
- Drink your last drink of the day at least 1 hour before your bedtime.
- Always keep the head of your bed at a 30-degree angle or higher. Use a wedge to keep your upper body and head raised up. You can buy a wedge at a surgical supply store or online.
- When you bend down, try bending at your knees instead of your waist.
- Do not eat or drink too much at one time.
- Talk with your care team about taking a medicine to help manage reflux.
Eating at restaurants and social events
Food is the focus of many social events. Remember that portions served at events and restaurants tend to be large. It often takes some time to get used to eating at restaurants or events like weddings and dinner parties.
- If you finish an appetizer, you may find that you need to take your entrée home.
- If you skip the appetizer, try eating half of your entrée and taking the rest home. You can also share an entrée with a friend.
- You may have to choose between having a small soup or a drink. Or, you can choose to have just a few sips of both.
- If you want to have dessert after your meal, you may want to take it home and save it for later.
Tracking your food and liquid Intake
After your gastrectomy, you may feel full quickly or have other changes that affect your eating. Keep a food and drink log. This will help you see what foods and portion sizes are easiest for you to eat. It will also help you make sure you’re getting enough calories.
In your food and drink log:
-
Keep track of all of the foods you eat and liquids you drink. Write down:
- The time you eat or drink
- The amount (portion) and type of food or drink
- The number of calories in the food or drink
-
Write down any symptoms or problems you have after eating or drinking.
- Are you feeling too full?
- Do you have pressure in your chest?
- Are you having reflux?
- Are you having pain in your abdomen (belly) or diarrhea?
Here is an example of a food and drink log. There is also a blank log for you to use at the end of this resource.
| Time | Portion size | Description | Calories | Symptoms? |
|---|---|---|---|---|
| 4 oz | Apple juice | 60 | None | |
| 1 jumbo 5 oz | Scrambled egg Mashed potatoes | 100 160 | None | |
| 6 oz | Yogurt | 105 | None | |
| 5 oz 4 oz | Mashed potatoes Vanilla pudding | 160 110 | None | |
| 1 jumbo | Scrambled egg | 100 | None | |
| 6 oz 5 oz ¼ cup ¼ cup | Mashed potatoes Soft cooked butternut squash Stewed chicken Gravy | 192 75 58 50 | Very full, unable to finish meal | |
| Daily total 1130 calories |
Tracking your weight
It’s important to track your weight. Weigh yourself about every 3 to 5 days. It’s best to weigh yourself around the same time of day each time. Make sure you’re wearing the same amount of clothing when you weigh yourself. If you’re losing weight, make a follow-up appointment with a clinical dietitian nutritionist.
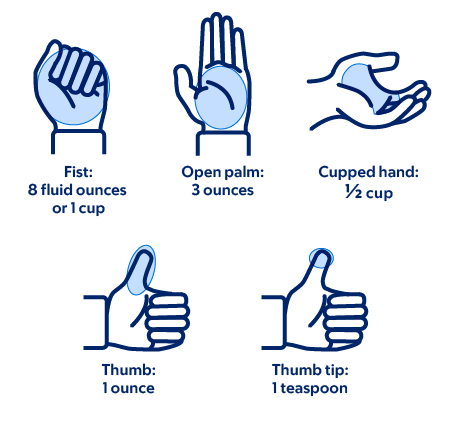
Measuring foods
To measure foods, use measuring spoons, measuring cups, or a food scale. You can also use the guidelines in Figure 4 to estimate amounts of some foods.
Finding calorie information
You can find the calorie information for packaged foods on the nutrition facts label (see Figure 5).
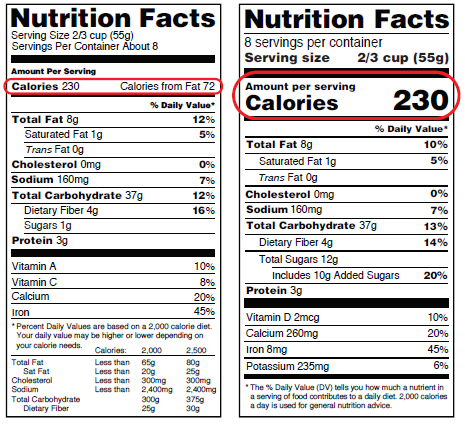
A food may not have a nutrition facts label. If so, you can look up the calorie information on a nutrition resource website, such as CalorieKing.com or MyFitnessPal.com. You can also download the MyFitnessPal application (app) to your smartphone.
Shopping list after surgery
For about 2 to 4 weeks after your surgery, eat smaller meals more often. Have foods high in calories and protein. You will not be eating large portions of foods. Instead, you will need to eat foods that give you the most nutrition in just a few bites.
The foods listed in this section will help you get the nutrients you need. These foods are also easier to digest (break down).
| Food group | Recommended foods |
|---|---|
| Milk and dairy |
|
| Vegetables |
*All vegetables should be well-cooked and very soft. |
| Fruits |
|
| Starches |
|
| Fats and oils |
*Do not eat acidic dressings if you have acid reflux. |
| Meat and meat substitutes |
|
| Drinks |
|
Kitchen items that can help after surgery
Here are some kitchen items that can help you make foods at home. You do not need to blend your food after surgery. But making soups and shakes with different foods can help you reach your calorie and protein goals.
- Blender: Use a blender to make soups and shakes. You can put meats, vegetables, and fruits in a blender. You may have to add liquid to make the food the right texture.
- Food processor: Use a food processor for shredding, slicing, chopping, or blending foods. It comes in different sizes. If you plan to make just 1 portion of food, buy a small processor.
- Small (salad) plates: Use small plates to help meals seem less overwhelming.
- Measuring cups and spoons: Use measuring cups and spoons to help with guiding portion sizes as you start eating after surgery.
Resources
MSK support services
Integrative Medicine and Wellness Service
www.msk.org/integrativemedicine
Our Integrative Medicine and Wellness Service offers many services to complement (go along with) traditional medical care. For example, we offer music therapy, mind/body therapies, dance and movement therapy, yoga, and touch therapy. Call 646-449-1010 to make an appointment for these services.
You can also schedule a consultation with a healthcare provider in the Integrative Medicine and Wellness Service. They’ll work with you to make a plan for creating a healthy lifestyle and managing side effects. Call 646-608-8550 to make an appointment for a consultation.
Resources for Life After Cancer (RLAC) Program
646-888-8016
At MSK, care does not end after your treatment. The RLAC Program is for patients and their families who have finished treatment.
This program has many services. We offer seminars, workshops, support groups, and counseling on life after treatment. We can also help with insurance and employment issues.
External resources
Academy of Nutrition and Dietetics (AND)
www.eatright.org/
AND is a professional organization for registered dietitians. The website has information about the latest nutrition guidelines and research and can help you find a dietitian in your area. The academy also publishes The Complete Food & Nutrition Guide which has over 600 pages of food, nutrition, and health information.
American Institute for Cancer Research
www.aicr.org
800-843-8114
The AICR has information on diet and cancer prevention research and education.
FDA Center for Food Safety and Applied Nutrition
www.fda.gov/AboutFDA/CentersOffices/OfficeofFoods/CFSAN/default.htm
The FDA has helpful information on food safety.
6-Meal diet sample menus
The sample menus in this section show a soft diet in 6 small meals. They include 4 ounces of liquid with each meal. This is to keep you from feeling too full during meals. They also include 8 ounces of liquid between meals, to keep you hydrated. Remember that soup and protein shakes also count as liquids.
-
Not all of the menu items are sugar-free. If you have diabetes, high blood sugar, or are having dumping syndrome:
- Use sugar-free or light yogurt in place of regular yogurt.
- Limit fruit juices.
- If you drink fruit juices, dilute them with water.
-
Menu items with an asterisk (*) have lactose. If you’re lactose-intolerant:
- Try Lactaid milk, cottage cheese, or ice cream.
- Take Lactaid tablets or drops before having dairy products.
- Choose almond milk, rice milk, or soy milk and non-dairy cheeses.
You may have had a large part or all of your stomach removed. If so, you may need to start with even smaller portion sizes than we list on the sample menus. Please talk with your clinical dietitian-nutritionist for more information.
Sample menu 1
| Time | Meal | Foods and Liquids |
|---|---|---|
| Breakfast |
| |
| Drink |
| |
| Snack |
| |
| Drink |
| |
| Lunch |
| |
| Drink |
| |
| Snack |
| |
| Drink |
| |
| Dinner |
| |
| Drink |
| |
| Snack |
| |
| Drink |
|
Sample menu 2
| Time | Meal | Foods and Liquids |
|---|---|---|
| Breakfast |
| |
| Drink |
| |
| Snack |
| |
| Drink |
| |
| Lunch |
| |
| Drink |
| |
| Snack |
| |
| Drink |
| |
| Dinner |
| |
| Drink |
| |
| Snack |
| |
| Drink |
|
Sample menu 3
| Time | Meal | Foods and Liquids |
|---|---|---|
| Breakfast |
| |
| Drink |
| |
| Snack |
| |
| Drink |
| |
| Lunch |
| |
| Drink |
| |
| Snack |
| |
| Drink |
| |
| Dinner |
| |
| Drink |
| |
| Snack |
| |
| Drink |
|
Sample menu 4
| Time | Meal | Foods and Liquids |
|---|---|---|
| Breakfast |
| |
| Drink |
| |
| Snack |
| |
| Drink |
| |
| Lunch |
| |
| Drink |
| |
| Snack |
| |
| Drink |
| |
| Dinner |
| |
| Drink |
| |
| Snack |
| |
| Drink |
|