This information describes enteroceles and rectoceles. It also describes how they are repaired.
About enteroceles
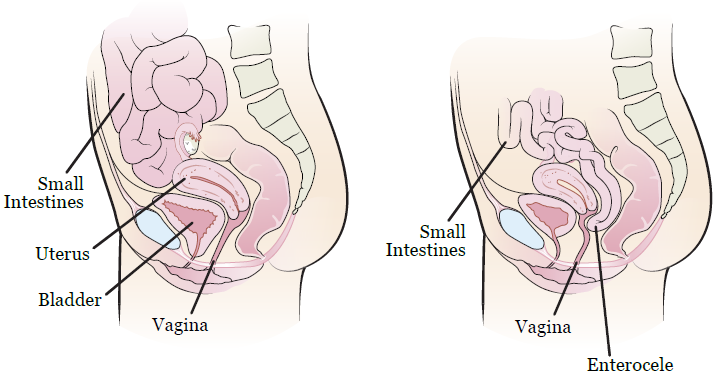
An enterocele (en-TUH-roh-seel) is when your small intestine moves downward. This makes your intestine push on the back wall of your vagina, making it bulge (see Figure 1). An enterocele is also called a small bowel prolapse.
About rectoceles
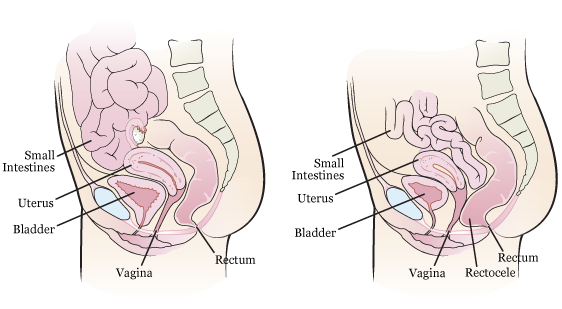
A rectocele (REK-toe-seel) is when your rectum moves forward. This makes your rectum push into the back wall of your vagina, making it bulge (see Figure 2). A rectocele is also called a posterior prolapse.
Causes of enteroceles and rectoceles
Having gynecologic (GY-neh-kuh-LAH-jik) surgery, such as a hysterectomy (HIS-teh-REK-toh-mee), can cause an enterocele. Gynecologic surgery is surgery on the female reproductive system. A hysterectomy is surgery to remove your uterus.
Chronic constipation can cause a rectocele. This is when you have trouble pooping over a long period of time.
Enteroceles and rectoceles can also be caused by:
- Aging.
- Family history.
- Vaginal delivery of heavy babies.
- Menopause. This is the end of your menstrual cycles (monthly periods).
Symptoms of enteroceles and rectoceles
If you have an enterocele or rectocele, you may:
- Have a heavy feeling in your vagina.
- Feel a bulge in your vagina.
- Have trouble emptying your bladder.
- Have trouble passing a bowel movement (pooping). You may need to press on your vaginal wall to help you poop.
- Feel pain during sex.
How to treat enteroceles and rectoceles
You can make your pelvic muscles stronger with physical therapy (PT).
You may have a pessary device put into your vagina. The device will hold up the organs that cause the bulge. This support may help ease your symptoms.
You may need repair surgery if these treatments do not improve your symptoms. If you need repair surgery, your care team will talk with you about how to get ready. Read Getting Ready for Surgery to learn more.
About your repair surgery
Repair surgery makes the wall of your vagina stronger using sutures (stitches). This stops your small intestine or rectum from bulging into your vagina. Your small intestine and rectum are not part of your surgery.
A urologist or urogynecologist (yoor-oh-GY-neh-KAH-loh-jist) will do your repair surgery. A urologist treats the parts of the body that make and pass urine (pee). A urogynecologist treats females with pelvic floor disorders.
You will need general anesthesia (medicine to make you sleep) for repair surgery.
Your surgery will take 1 to 2 hours.
Risks of repair surgery
Most people do not have problems after repair surgery. Some may need another repair surgery to correct the problem.
After your surgery, you may have:
- Infection.
- Vaginal bleeding.
- Bladder spasms (cramping).
- Pain that lasts a few days, up to 2 weeks.
- Narrowing of your vagina.
- Pain during sex.
- Injury to your bladder or ureters. Ureters are tubes that take urine from your kidneys to your bladder.
- Incontinence (losing control of your bladder). You may have strong urges to urinate (pee). This can cause leakage. You may have trouble holding in your urine long enough to reach the toilet.
- Long-term problems urinating (peeing). You may need a catheter (thin, flexible tube) put into your bladder to help drain your urine.
After your repair surgery
Dressing and catheter
You will have a dressing (gauze bandage) in your vagina after your surgery. This will help stop any bleeding.
You will also have a catheter to drain urine from your bladder. Your nurse will take out the gauze and catheter the day after your surgery.
You may have bleeding from your vagina for about 4 to 6 weeks after surgery. You can wear a pad or panty liner to protect your clothes. Do not use tampons.
Safety instructions
You can shower 48 hours (2 days) after your surgery. Do not take tub baths, swim, or sit in a pool or hot tub. Ask your healthcare provider when it is safe to do these things.
Do not have sex or put anything in your vagina for 6 weeks after your surgery. This includes tampons.
Do not lift anything heavier than 10 pounds (4 ½ kilograms) for 6 weeks after your surgery. Avoid high-energy exercise for 3 months after your surgery. This includes running or jogging, bike riding, and heavy lifting.
Ask your healthcare provider when it is safe to go back to work and do your everyday tasks.
Follow-up appointment
You will need to schedule a follow-up appointment 2 weeks after your surgery.
When to call your healthcare provider
Call your healthcare provider if:
- You have a fever of 101 °F (38.3 °C) or higher.
- Your vagina is bleeding more than when you were in the hospital.
- You feel pain that does not go away with pain medicine.
- You have not had a bowel movement (poop) in over 48 hours (2 days).
- You have not passed gas in over 24 hours (1 day).
- You have nausea (feeling like you’re going to throw up), vomiting (throwing up), or both.
- Any questions or concerns.
