This information will help you understand malignant (cancerous) mesothelioma (MEH-zoh-THEE-lee-OH-muh), including risk factors, diagnosis, surgery, and treatment.
About mesothelioma
Mesothelioma is a rare type of cancer of the tissue that lines your internal organs. There are a few different types of mesothelioma.
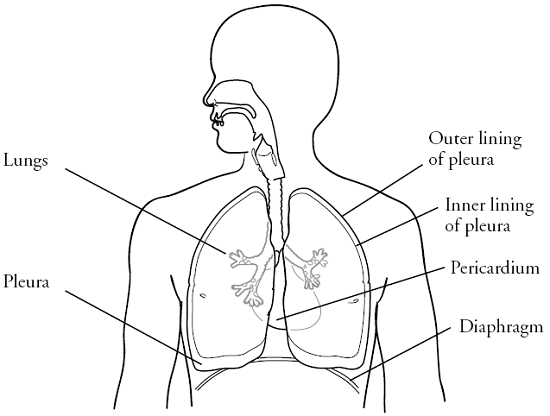
- Pleural mesothelioma affects your pleura, which is the sac that surrounds your lungs (see Figure 1). This is the most common type of mesothelioma.
- Peritoneal (PAYR-ih-toh-NEE-ul) mesothelioma affects your peritoneal membrane, which is the tissue that surrounds your abdominal organs (the organs in your belly).
- Pericardial (PAYR-ih-KAR-dee-ul) mesothelioma affects your pericardium, which is the sac that surrounds your heart (see Figure 1). This type of mesothelioma is rare.
- Testicular mesothelioma affects the lining of your testicles. This type of mesothelioma is rare.
Risk factors for mesothelioma
The main known risk factor for mesothelioma is exposure to asbestos. Asbestos is a mineral fiber that’s found in some older buildings.
People who work in mining, milling, construction, plumbing, heating, insulation, carpentry, electrical, or shipyard work generally have the most exposure to asbestos. They’re at higher risk of developing mesothelioma. Family members of these workers are also at higher risk because they may have been exposed to asbestos in the clothes and hair of the workers. However, people outside of these professions can also develop mesothelioma.
Diagnosing mesothelioma
To see if you have mesothelioma, you will have a biopsy. During the biopsy, your healthcare provider will remove a small piece of tissue from the area where the cancer may be. A pathologist will look at the sample of tissue under a microscope to see if it’s cancer.
There are several ways to do a biopsy, including thoracentesis, video-assisted thoracic surgery (VATS), open lung biopsy, or diagnostic laparoscopy (LA-puh-ROS-koh-pee). Your healthcare provider will talk with you about which one is best for you.
Thoracentesis
Thoracentesis is a procedure in which a needle is used to remove fluid from between the layers of your pleura. It can be done in your healthcare provider’s office or in a hospital.
Video-assisted thoracic surgery (VATS)
VATS is a type of minimally invasive surgery. During VATS, your healthcare provider will make 1 to 3 small incisions (surgical cuts) in your chest. They will put a laparoscope (long, thin video camera) and 2 long, thin surgical tools into the incisions. They will use the laparoscope and tools to remove tissue to be tested.
VATS is usually done in an operating room.
Open lung biopsy
During an open lung biopsy, your healthcare provider will make a small incision between your ribs and remove a piece of your pleura. This procedure is done in the operating room.
Diagnostic laparoscopy
A diagnostic laparoscopy is a type of minimally invasive surgery. During a diagnostic laparoscopy, your healthcare provider may make 1 to 3 small incisions in your abdomen (belly). They’ll put a laparoscope and 2 long, thin surgical tools through the incisions. They’ll use the laparoscope and tools to study the progress of your cancer, determine whether surgery to remove your cancer may be possible, and perform a biopsy.
A diagnostic laparoscopy is done in an operating room as an outpatient procedure under general anesthesia.
Paracentesis
Paracentesis is a procedure in which a needle is used to remove fluid from between the layers of your peritoneal membrane. It can be done in your healthcare providers’ office or in a hospital.
Other tests
Your healthcare provider may want you to have other tests, such as:
- A computed tomography (CT) scan or a positron emission tomography (PET) scan to see if the cancer has spread.
- A pulmonary function test (PFT), a ventilation perfusion scan, or both to see how your lungs are working.
- A stress test to check your heart.
- Bloodwork to check how your organs are working.
If you need to have any other tests, your healthcare provider will discuss this with you. All of these tests will help your healthcare provider plan the best treatment for you.
Treatment
Your treatment may include surgery, radiation therapy, and chemotherapy. Your healthcare team will work with you to make a treatment plan that’s based on the stage of your cancer and your overall health.
Surgery
The goal of surgery for mesothelioma is to remove all of the visible cancer. How much tissue is removed during surgery depends on where the cancer is and which type of mesothelioma you have. Your healthcare team will talk with you about what to expect if you choose to have surgery.
Radiation therapy
Radiation therapy uses high-energy rays to kill cancer cells and help lower the risk of recurrence (the cancer coming back). Your healthcare team will go over radiation planning, treatment, and possible side effects with you.
Chemotherapy
Chemotherapy is a medication or a combination of medications that’s used to treat cancer. The most commonly used chemotherapy to treat mesothelioma includes 2 medications: pemetrexed (Alimta®) and cisplatin. Your healthcare team will discuss the benefits and risks of chemotherapy with you.
Your healthcare provider may also recommend other medications, immunotherapy, or the possibility of joining a clinical trial.
Managing pleural effusions
A pleural effusion is when there’s a buildup of fluid between the layers of tissue surrounding your lungs. This can limit how much your lungs can expand and make you feel short of breath. Shortness of breath is a symptom of pleural effusion.
If you have a pleural effusion, your healthcare provider may do a procedure called a thoracentesis. In this procedure, your healthcare provider will put a needle into your chest to remove the fluid. This will help you breathe and feel more comfortable.
If this doesn’t keep the fluid from coming back, you may need to have a PleurX® drainage catheter placed in your pleural space. Your nurse will give you more information about PleurX catheters, if needed.
Managing ascites
Ascites is when there’s a buildup of fluid between the layers of tissue surrounding the organs in your abdomen. This can cause pain and swelling. Ascites is a symptom of peritoneal mesothelioma.
If you have ascites, your healthcare provider may do a procedure called a paracentesis. In this procedure, your healthcare provider will put a needle into your abdomen to remove the fluid. This will help decrease the swelling and pain.
If this doesn’t keep the fluid from coming back, you may need to have a drainage catheter placed in your abdomen. Your nurse will give you more information about this, if needed.
MSK resources
You can also visit the Peritoneal & Pleural Mesothelioma Cancers section of www.msk.org for more information.
Anesthesia Pain Service
212-639-6850
MSK’s Anesthesia Pain Service will work with you to manage your pain both while you’re in the hospital and after you’re discharged.
Integrative Medicine and Wellness Service
www.msk.org/integrativemedicine
Our Integrative Medicine and Wellness Service offers many services to complement (go along with) traditional medical care, including music therapy, mind/body therapies, dance and movement therapy, yoga, and touch therapy. To schedule an appointment for these services, call 646-449-1010.
You can also schedule a consultation with a healthcare provider in the Integrative Medicine and Wellness Service. They will work with you to come up with a plan for creating a healthy lifestyle and managing side effects. To make an appointment, call 646-608-8550.
MSK Library
library.mskcc.org
You can visit our library website or email [email protected] to talk with the library reference staff. They can help you find more information about a type of cancer. You can also visit the library’s Patient Education Resource Guide.
Nutrition Services
www.msk.org/nutrition
212-639-7312
Our Nutrition Service offers nutritional counseling with one of our clinical dietitian nutritionists. Your clinical dietitian nutritionist will talk with you about your eating habits. They can also give advice on what to eat during and after treatment. To make an appointment, ask a member of your care team for a referral or call the number above.
Emotional support
Cancer diagnosis and treatment can be very stressful and overwhelming. You may feel depressed, anxious, confused, afraid, or angry. You may have strong feelings about any permanent changes. These changes can have an impact on your emotional well-being. Help is available for you at any time. If you would like counseling, your nurse can give you a referral to see a social worker, psychiatrist, or counselor. You can also find more information below.
Counseling Center
www.msk.org/counseling
646-888-0200
Many people find that counseling helps them. Our counseling center offers counseling for individuals, couples, families, and groups. We can also prescribe medications to help if you feel anxious or depressed. To make an appointment, ask your healthcare provider for a referral or call the number above.
Social Work
www.msk.org/socialwork
212-639-7020
Social workers help patients, families, and friends deal with common issues for people who have cancer. They provide individual counseling and support groups throughout your treatment. They can help you communicate with children and other family members.
External resources
American Cancer Society (ACS)
www.cancer.org
800-227-2345
Cancer.net
www.cancer.net
571-483-1780 or 888-651-3038
National Cancer Institute (NCI)
www.cancer.gov
800-422-6237 (800-4-CANCER)
Mesothelioma Applied Research Foundation
www.curemeso.org
877-363-6376
Mesothelioma.com
www.mesothelioma.com
800-336-0086