This information will help you prepare for your urodynamic evaluation, including what to expect before, during, and after your procedure.
About Your Urodynamic Evaluation Procedure
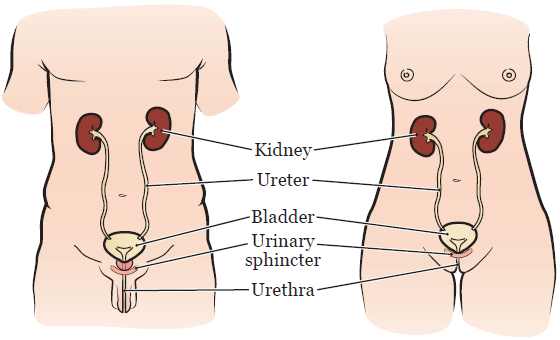
A urodynamic evaluation is a procedure to test how well your bladder, urinary sphincter, and urethra are working (see Figure 1).
Your bladder stores urine (pee) until you’re ready to urinate. Your urinary sphincter controls the flow of urine out of your bladder. Your urethra is the tube that carries urine from your bladder out of your body.
Your healthcare provider will use this procedure to see:
- How well your bladder stores urine.
- How well your bladder empties urine.
- If your bladder leaks urine.
- How well you urinate.
Some people may also need to have a cystoscopy. This is a procedure to look at your urethra, bladder, and openings to your ureters (the tubes that carry urine from your kidneys into your bladder). Your healthcare provider will tell you if you need to have a cystoscopy after your urodynamic evaluation.
Before Your Procedure
- Tell your healthcare provider if you take any bladder medications. You may need to stop taking these medications 2 weeks before your procedure.
- Your healthcare provider will give you a prescription for an antibiotic. You will need to take the antibiotic on the day of your procedure.
- Fill out a voiding diary to keep track of how often you urinate. Your nurse will show you how to do this.
The Day of Your Procedure
- Take your antibiotic as prescribed.
- Don’t drink caffeinated liquids such as caffeinated tea, coffee, or soda.
- You can eat your meals like you normally do.
During Your Procedure
Your procedure will be done at the Sidney Kimmel Center for Prostate and Urologic Cancers. Take the elevator to the concourse level and check in at the desk.
For your procedure, you will change into a hospital gown and lie down on an exam table. Your healthcare provider will insert a very small tube into your bladder or urinary diversion, if you have one. This tube will be used to fill your bladder with liquid and measure the pressure inside your bladder. They will put another very small tube into your rectum or stoma. This tube will be used to measure the pressure outside your bladder. The tubes are connected to others that are attached to a computer.
Next, your nurse will place 2 small electrodes close to your anus to measure muscle contractions. The electrodes are like the ones used during an electrocardiogram (EKG).
After the tubes and electrodes are in place, contrast dye (or contrast) will begin to flow through the tube into your bladder or urinary diversion. Contrast is a liquid that’s sometimes used in x-rays to help your healthcare providers see your organs better. A member of your healthcare team will take several x-rays to look at the shape of your bladder.
While your bladder is being filled with contrast, your nurse will ask you to tell them:
- When your bladder feels full.
- When you have the urge to urinate.
- When you have a strong urge to urinate.
You may be asked to strain at certain times while your bladder is filling. This may show urine leakage. Once you have a full bladder and a strong urge to urinate, you will empty your bladder with the tubes still in place. More x-rays will be taken.
When your procedure is finished, the tubes and electrodes will be removed.
Cystoscopy
If you’re having a cystoscopy after your urodynamic evaluation, it will be done in a separate room. During the cystoscopy, your healthcare provider will insert a scope (hollow tube with a tiny light on the end) into your urethra. They will look at a monitor that shows the inside of your bladder. A cystoscopy will be done for male patients to rule out bladder stones, tumors, polyps, and blockage by the prostate gland.
After Your Procedure
You may have discomfort or slight bleeding when you urinate. Try to drink 8 (8-ounce) glasses (2 liters) of liquids each day for 2 days after your procedure.
Call Your Healthcare Provider if You:
- Have bleeding or discomfort that doesn’t improve within 48 hours after your procedure
- Have a fever of 101° F (38.3° C) or higher
- Can’t urinate