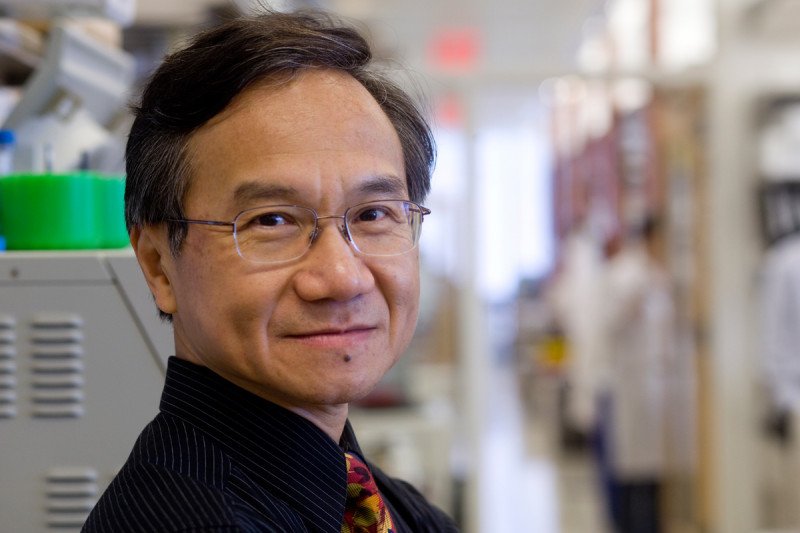
Nai-Kong Cheung, head of the neuroblastoma research program in Memorial Sloan Kettering’s Department of Pediatrics and Enid A. Haupt Chair in Pediatric Oncology, believes that a better understanding of tumors will lead to improved treatments for children with this cancer.
What is neuroblastoma?
Neuroblastoma starts in primitive cells of the sympathetic nervous system. Some neuroblastoma tumors have spread and require aggressive treatment. Others are less threatening and can actually disappear or remain unchanged with minimal or no treatment. Our priority is to identify the 50% of patients who do not need treatments, such as radiation or chemotherapy. For those with high-risk disease, we design treatments that are not only more effective but also less toxic.
How did you become interested in studying and treating children with neuroblastoma?
It was heart-wrenching to witness children and their families stricken by neuroblastoma. I felt there must be more that we as physician-scientists could do for them. I resolved to devote my professional life to finding treatments to beat this disease.
How do you and your team determine which type of neuroblastoma a child has?
Sophisticated imaging and molecular pathology tools help us. We can now identify children whose tumors do not need chemotherapy or radiation with increasing certainty. For them, we can achieve a survival rate greater than 90%. This is a substantial improvement compared with a decade ago. Sparing children unnecessary therapy is always a blessing. Devastating treatment-related issues can follow even if a child is cured of neuroblastoma.
What about children whose tumors need more intensive treatment?
We have also made a lot of progress controlling high-risk disease in recent years. For almost three decades, we have been using medicines that can go precisely to tumor cells to treat neuroblastoma that has spread. These drugs are called monoclonal antibodies. They empower the body’s own immune cells to keep cancer at bay. Antibodies can also carry radioisotopes to deliver liquid radiation. We have improved the way we combine chemotherapy, surgery, radiation, and immunotherapy for high-risk metastatic neuroblastoma. We showed that by combining the monoclonal antibody 3F8 with a growth factor for white cells called GM-CSF, we could destroy tumor cells hiding in the bone marrow. For a cancer that was once incurable, a cure is definitely within reach today.
What happens if a tumor comes back after initial treatment?
We are developing better strategies and antibody drugs to treat or prevent recurrences in the brain or surrounding cerebrospinal fluid (CSF). Such recurrence happens in more than 10% of our patients. We inject antibody medicine directly into the CSF to kill tumor cells that hide there. In our studies, many patients who went through this treatment lived longer than expected and with few serious side effects.
On another front, we continue to improve our antibody drugs to make them more effective for humans. We also succeeded in demonstrating the safety and effectiveness of a cancer vaccine to prevent further relapse. A cure is now possible even for those whose cancers have returned. These developments are examples of successful collaborations among MSK researchers.
How do you manage side effects in children with neuroblastoma?
Cancer treatments for children with high-risk neuroblastoma include chemotherapy, radiation, surgery, and immunotherapy. We are mindful that there will be short-term and long-term side effects from such aggressive treatment. Therefore, drugs have to be made tumor-specific to prevent or reduce organ damage. The treatment must be personalized to maximize benefit while minimizing side effects.
What is a typical day like for you?
For 25 years, half of my time was spent taking care of patients. Now 100% of my time is focused on new drug development. Given the emerging possibilities of immunotherapy in the past five years, children with cancer should not miss out on getting novel and effective medicines.
What keeps you motivated?
We continue to bridge our laboratory findings to the clinic, creating new drugs to increase treatment options. We want these drugs to be so effective that children will not have to face relapses and so specific that their organs will not be damaged. We want to see our patients as cancer survivors leading normal lives.
Nai-Kong Cheung has received commercial research grants from Y-mAbs Therapeutics. Dr. Cheung is an inventor on issued patents licensed by MSK to Y-mAbs and holds equity interests in Y-mAbs.


