Chimeric antigen receptor (CAR) T cells are a type of “living drug” that can treat aggressive forms of blood cancer. Because the cells persist in the body and respond dynamically to cancer, they can sometimes take an unpredictable course, dividing more in some people than others and causing side effects.
One potentially serious side effect of CAR therapy is cytokine release syndrome (CRS). This sudden surge in immune activity can cause high fever, high blood pressure, and death if not skillfully managed. It is an obstacle to the treatment becoming more widely available beyond select medical centers. Though approaches exist to eliminate out-of-control CAR T cells, they all involve permanently terminating the therapy. Doctors and patients have therefore been reluctant to use these methods, even when side effects are severe.
Now, a team of researchers at Memorial Sloan Kettering and University Hospital in Würzburg, Germany, has identified a simple drug treatment that can temporarily shut down CAR T cell function without destroying the cells. The drug, dasatinib (Sprycel®), is a type of tyrosine kinase inhibitor approved for the treatment of leukemia. It works by blocking an important step of CAR T cell activation called phosphorylation.
Using a mouse model of CRS developed by the MSK researchers, the team found that prompt administration of dasatinib could increase the survival of mice facing severe CRS from 25% to 70%. What’s more, the effect is reversible and does not impair the cells’ long-term tumor-killing ability.
“If these findings hold up in patients, this study will have a major impact on CAR therapy, including its cost and restrictions owing to the occurrence of CRS,” says Michel Sadelain, Director of the Center for Cell Engineering at MSK and a co-author on the paper, which published was published on July 3 in the journal Science Translational Medicine.
With dasatinib, he explains, CAR T cells could be switched off temporarily and then allowed to switch back on once the side effect is over, like a kind of snooze button.
Lead author Michael Hudecek and his co-authors conclude that “the evaluation and implementation of dasatinib as an on/off control drug in CAR T cell immunotherapy should be feasible and straightforward.”
About CAR T
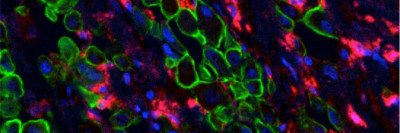
CAR T cells are genetically engineered immune cells that have been equipped with a synthetic receptor designed to recognize cancer cells and activate an immune response.
MSK researchers have played a pivotal and pioneering role in the development of CAR therapy. Today, multiple teams of researchers at MSK are investigating how to make CAR therapy better, safer, and more affordable. A list of currently available CAR T clinical trials can be found here.