A virus you likely carry could hold clues to your future health.
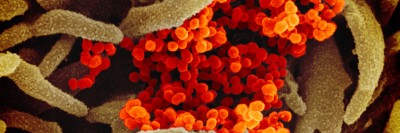
Epstein-Barr virus (EBV) infects nearly everyone, and for most people it hides quietly in the body for life. But for some, this common virus can do far more than linger and is linked to increased risk of developing chronic diseases of the lung and heart, lupus, and certain cancers.
A new collaborative research study by researchers at Memorial Sloan Kettering Cancer Center (MSK), AstraZeneca, and Baylor College of Medicine, has identified 22 specific genetic variants that are linked to both higher active levels of EBV and chronic disease risk. The team discovered that the genetic differences — many in immune-system genes — could make it harder for the body to keep EBV under control. People with these genetic variants might be more likely to develop chronic EBV-related ailments.
MSK computational biologist Caleb Lareau, PhD, helped lead the research along with Slavé Petrovski, Vice President, Centre for Genomics Research, AstraZeneca, and Ryan Dhindsa, Assistant Professor, Pathology & Immunology, Baylor College of Medicine. The findings were published in the journal Nature on January 28.
A Gold Mine of Data About Viruses
Traces of viral DNA are generally dismissed as “noise” and cast aside when researchers run a typical whole-genome analysis. But rather than ignoring the EBV DNA, Dr. Lareau and his colleagues used a novel computational method to quantify how much of this genetic material was circulating in the blood. They found that EBV DNA levels vary among individuals and are influenced by genetic factors, particularly those related to the immune system.
“We saw the untapped potential of this routinely discarded viral DNA and generated valuable insights at a scale previously unimaginable, turning trash into treasure,” says Dr. Lareau, Assistant Member of the Computational and Systems Biology Program and one of the corresponding authors. “Our approach can be extended beyond EBV, enabling the detection and analysis of other viruses hidden within large genome-sequence datasets.”
Dr. Lareau was recently awarded a five-year, $5 million grant to work on the Human Virome Program, an ambitious project that seeks to map the many viruses that are part of the body’s ecosystem. Sponsored by the National Institutes of Health, the project aims to understand how this collection of viruses — known as the virome — may influence human health in unexpected ways.
“The big questions are about how the various viruses you have been exposed to, combined with your unique genetic fingerprint and other factors, influence your likelihood of developing different diseases — including cancer,” says Dr. Lareau, who is also Assistant Professor, Computational Biology and Medicine at Weill Cornell Medicine.
Analyzing a Massive Data Set
In the new collaborative study — a team effort spearheaded by MSK computational biologist Sherry Nyeo and research fellow Erin Cumming, along with Oliver Burren of AstraZeneca — researchers used a powerful new computational method to analyze the full genome sequence and health data from 750,000 people.
The researchers developed computational models capable of processing millions of gigabytes of sequencing data to create a new metric called EBV DNAemia. This measure reflects high levels of EBV genetic material circulating in the blood — found in about 10% of people previously infected — and allowed the team to uncover links between viral burden, genetic differences, and specific health outcomes.
For example, people with higher EBV levels have about 50% higher risk of rheumatoid arthritis and nearly twice the risk of chronic obstructive pulmonary disease compared with those who have lower EBV levels. Insight into the genetic drivers behind this could help clarify who is at greater risk of longer-term disease burden while also informing the next wave of research into therapeutic and potentially early intervention strategies.
The Immune System’s Command Center
The 22 genetic variants uncovered in the study were linked to high levels of EBV DNA as well as higher disease rates. Many of these genes sit in the immune system’s command center, the Human Leukocyte Antigen (HLA) region of the genome. This region is a set of genes that controls how viral fragments are presented to immune cells to elicit an immune response.
Variants in genes like ERAP1 and ERAP2 can tip this balance influencing viral presentation — while strong presentation helps to contain EBV, weak presentation lets it linger and could raise future health risks.
The team also found links to genes outside the HLA region involved in T cell activation and interferon pathways, such as PTPN22 and SH2B3, which are both known drivers of autoimmune diseases. These findings reveal overlapping genetic pathways that govern both EBV control and autoimmune risk, highlighting immune-regulating genes as possible biomarkers but also as potentially therapeutic targets.
Mapping viral levels and understanding their genetic drivers could be a critical step toward the future of chronic disease care. In addition, the computational method can be used beyond EBV to study the long-term effects of similar viruses within existing genomic-sequencing data.
Key Takeaways
- The Epstein-Barr virus (EBV) infects nearly everyone but usually hides quietly in the body for life.
- In some people, EBV increases the risk of developing chronic diseases.
- Researchers identified 22 specific genetic variants that are linked to both higher active levels of EBV and chronic disease risk.
- People with these genetic variants might be more likely to develop the chronic EBV-related ailments.
This story was written by staff at MSK, AstraZeneca, and Baylor.
Additional Authors, Funding and Disclosures
Additional MSK authors on the study include Sherry S. Nyeo, Erin M. Cumming, Meghana S. Pagadala, Jacob C. Gutierrez, Thahmina A. Ali, Laura C. Kida, Hoyin Chu, and Kushal K. Dey.
This work was supported by NIH grants U01AT012984, P30CA008748, R00HG012579, R00HG012203, and R01HG014008, and a Michelson Prize Next-Generation Grant.
Dr. Lareau is a consultant to Cartography Biosciences.
Read the article: “Population-scale sequencing resolves correlates and determinants of persistent Epstein-Barr Virus DNA,” Nature, DOI:10.1038/s41586-025-10020-2