Researchers Roisin O'Cearbhaill (left) and Christopher Klebanoff are conducting immunotherapy trials for a range of gynecologic cancers.
The American Cancer Society estimates that more than 113,000 people in the United States are diagnosed with a gynecologic cancer every year. Memorial Sloan Kettering is a leader in treating people with these cancers, which include tumors of the cervix, ovaries, and uterus.
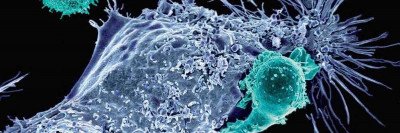
Among the new treatments being developed for gynecologic cancers are a type of immunotherapy called T cell therapies. These are treatments in which a patient’s own immune cells are modified to recognize and attack cancer cells. MSK doctors and scientists were the first to develop these treatments for leukemia and lymphoma. Now, many researchers are focused on further advancing this approach to make it effective against solid tumors.
“For certain blood cancers, cellular therapy can be remarkably potent, perhaps even curative,” says physician-scientist Christopher Klebanoff, whose lab is focused on developing new cell therapy approaches. One challenge of immunotherapy is directing the immune cells only to tumors so they don’t cause injury to healthy tissues.
Treating Cancer with CARs and TRUCKs
The most well-known cell therapy is chimeric antigen receptor (CAR) T therapy, which has shown success in treating certain blood cancers. CAR T modifies a patient’s immune cells (T cells) so they can recognize a protein (called an antigen) on the outer surface of cancerous cells. These supercharged T cells then seek out and destroy the cancer. For many cancers, especially cancers originating from a solid organ, the antigen isn’t quite as easy for the T cell to find, making cell therapies more challenging to develop.
This has led to a related tactic called T cell receptor (TCR) therapy, in which T cells are engineered to detect antigens on the inside of the cancer cell. “The ability to do this is one of the greatest tricks in biology,” Dr. Klebanoff says. “That is, how can you allow an immune cell to look inside other cells to detect if the proteins inside are normal or abnormal?”
As it turns out, the way this “looking” works is actually indirect: As part of normal cellular operations, proteins eventually get broken down and recycled to make new proteins. One step in this recycling process displays protein fragments on the surface of cells — allowing them to be seen by engineered T cells. TCR therapies are designed to take advantage of this natural process that the immune system uses to survey tissues in the body.
Some of the newest cell therapies known as TRUCKs — T cells redirected for antigen‐unrestricted cytokine‐initiated killing — work by combining the antitumor abilities of CAR T or TCR therapy with a molecule called a cytokine. The cytokine recruits another wave of immune cells to the tumor.
A Personalized Approach to Cancer Care
Medical oncologist Roisin O’Cearbhaill is the research director for the Gynecologic Medical Oncology Service and a leader in studying new cell therapies and immunotherapy approaches for treating gynecologic cancers, including a treatment for cervical cancer and other tumors caused by the human papillomavirus (HPV). “We’re building up our clinical trial program at MSK so that we will be able to offer more cellular therapies for patients with gynecologic cancers,” she says.
“With cell therapies, we use our knowledge about specific molecular and genomic properties of the patient’s cancer,” Dr. O’Cearbhaill explains. “And we may also use certain markers on their blood cells in order to get the best possible match for a targeted therapy for that individual patient.”
“For each of our patients, we take a very personalized approach to match the best possible medicines, including experimental medicines offered in clinical trials, with the patient’s disease,” Dr. Klebanoff says. “I’m a big believer in the concept of partnership and shared purpose, and this is how we work in collaboration with our patients. We have a shared purpose to try to improve things both for them and for others with similar diseases in the future.”
Clinical Trials Offering Cell Therapies for Gynecologic Cancers
MSK currently has a number of clinical trials that are examining this approach.
- Dr. O’Cearbhaill is co-leading a phase I study with Dr. Klebanoff that is assessing the safety and effectiveness of using a TCR therapy called KITE-439 to treat cancers caused by a strain of HPV called HPV 16. The majority of cervical cancers as well as many cancers of the mouth, throat, vagina, vulva, penis, and anus are associated with HPV 16. In this study, a patients’ immune cells are modified to recognize and attack tumor cells that contain HPV 16.
- The doctors are also co-leading a phase I trial for a cell therapy called KITE-718, which targets cancers containing MAGE-A3/A6, a protein found in some ovarian and cervical cancers as well as other kinds of cancer.
- To study another treatment for ovarian cancer and cancers of the fallopian tubes and the peritoneal cavity (the lower abdomen), Dr. O’Cearbhaill is leading a phase I trial for a CAR T therapy that targets a protein called MUC16, which is made by many of these tumors. MUC16, also called CA125, is best known as a biomarker used to monitor treatment for ovarian cancer.
- Dr. O’Cearbhaill is also leading a phase I/II trial for a TRUCK drug called TC-210, which is being tested in combination with chemotherapy. This cell therapy targets tumors that make a protein called mesothelin, which is found in several cancers, including some ovarian tumors.
Dr. Klebanoff’s laboratory and MSK receive research funds from Kite/Gilead, the sponsor of both TCR clinical trials. MSK receives clinical trial funding from Celgene and TCR2 Therapeutics for the CAR T cell and TRUCK studies, respectively.
Outside this work, MSK receives funding for clinical research that Dr. O’Cearbhaill is leading from Tesaro/GlaxoSmithKline, the Ludwig Cancer Institute, Abbvie, Regeneron, Atara Biotherapeutics, MarkerTherapeutics, Syndax Pharmaceuticals, Genmab Therapeutics, Sellas Therapeutics, Genentech, and the Gynecologic Oncology Foundation. Dr. O’Cearbhaill has served on advisory boards for Genmab, Regeneron, and GlaxoSmithKline.