Graft-versus-host disease (GVHD) is a major complication of bone marrow and blood stem cell transplantation. Although these transplants can cure patients with leukemia, lymphoma, or other blood disorders by replacing diseased blood-forming cells with healthy ones, GVHD can seriously impair recovery and even cause death.
Memorial Sloan Kettering researchers are studying how the intestinal tract heals from GVHD in hopes of developing new treatments for this serious condition. In a study published recently in Nature, an MSK team reports a discovery on how the patient’s immune system helps repair intestinal damage caused by GVHD. The findings also suggest that drugs based on a molecule from the immune system could be used as an effective GVHD treatment.
Donated Tissue Attacks
GVHD occurs after a transplant when donor immune cells called T cells recognize the recipient’s tissue as foreign and attack it. This complication can damage the liver, skin, digestive tract, or other organs. One of the most common sites of injury in GVHD is a section of the intestine called the epithelial layer, which lines the organ.
MSK physicians have pioneered a groundbreaking procedure for reducing GVHD risk by removing T cells from the group of donor cells prior to the transplant. However, not every patient can receive this type of transplant, and it has risks of its own.
Memorial Sloan Kettering physician-scientist Alan Hanash, who treats blood stem cell transplant patients, suggests the search for new therapies may benefit by expanding focus beyond the donor T cells to find ways to boost tissue repair after damage occurs.
“Much of the work in our field has centered on suppressing T cells without a lot of understanding of what’s actually happening in the tissues,” he says. “Our research group has begun concentrating on how the tissues are being damaged and, more importantly, how they recover from that damage.”
An Unexpected Immune System Role
In 2012, Dr. Hanash and physician-scientist Marcel van den Brink discovered that an immune signaling molecule called interleukin-22 (IL-22) helps the intestines recover from GVHD damage.
Immune cells that can produce IL-22 reside within the intestines, ready to respond when needed after infections or tissue damage. These cells help protect the body against infections and maintain the barrier between intestinal tissue and bacteria.
In the 2012 study, the MSK team discovered that these immune cells have another function: after the intestinal epithelial cells are damaged — as in GVHD — IL-22 also somehow protects the intestinal stem cells necessary for maintaining the epithelial layer. However, how this happens was unclear.
“There are multiple epithelial cell types in the intestinal tract,” Dr. Hanash says. “There are the mature intestinal epithelial cells, which are maintained by the stem cells, and there are niche cells that help to nurture and support the stem cells. We didn’t know whether IL-22 was acting only on mature cells, directly targeting the stem cells, indirectly helping the stem cells by promoting the function of the supportive niche cells — or perhaps all of these things.”
Direct Stimulation of Stem Cells
Fast-forward to now: In the new study, Dr. Hanash’s team found that IL-22 acts directly upon the intestinal stem cells to stimulate creation of new intestinal cells.
“Normally, the stem cells are able to maintain and replenish the tissue sufficiently,” Dr. Hanash says. “We now believe that when the intestinal epithelial tissue is damaged, IL-22 gets turned on and directly signals the stem cells to go into overdrive to promote recovery of the tissue, indicating that we’re no longer in maintenance mode — we’re now in recovery mode.”
The researchers used both mouse models and human tissue to study epithelial regeneration. This approach allowed them to tease apart the various biological signals and to show that IL-22 acts directly on the stem cells.
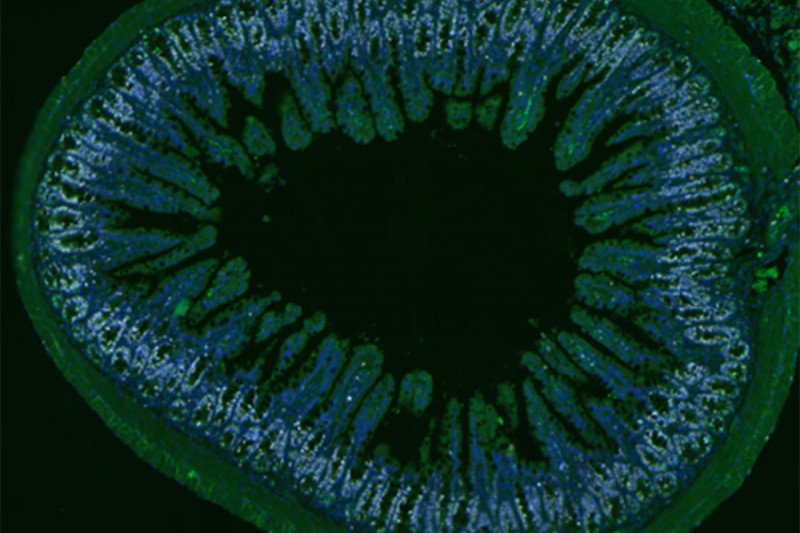
In one experiment, the scientists created three-dimensional “mini-guts” grown from intestinal stem cells that resemble the main features of the normal epithelium in the human gut. When they exposed these mini-guts to IL-22, the stem cells proliferated and dramatically increased the growth of the mini-guts.
In another experiment, mice that received bone marrow transplants and began to develop GVHD had reduced intestinal damage and a much better chance of surviving if they were treated with IL-22.
“This suggests that treatment with IL-22 can have real therapeutic effects,” Dr. Hanash says.
New Hope for Transplant Patients
To speed this treatment to patients, the MSK researchers have partnered with a pharmaceutical company that has developed a modified, potentially more potent form of IL-22. They plan to launch a phase II clinical trial at MSK in early 2016 to treat transplant patients experiencing GVHD of the intestinal tract. The drug will be given promptly when the complication emerges to head off serious damage, which is more difficult to treat.
Sergio Giralt, Chief of MSK’s Adult Bone Marrow Transplantation Service, says the findings hold great promise for transplant patients, as well as for other patients suffering intestinal damage.
“Dr. Hanash’s work now allows us to explore a strategy that can enhance healing of the gastrointestinal tract from the damages of graft-versus-host disease,” he says. “If successful, IL-22 could also be used for other causes of severe gastrointestinal damage that require tissue regeneration.”
Dr. Hanash emphasized the cross-disciplinary nature of this research, which involved immunologists and stem cell biologists. He says the interplay between specialties is increasingly important as evidence accumulates that the role of the immune system is broader than generally thought.
“It’s not a case of your intestines, your heart, or your liver all functioning independently — that’s not the way our bodies work,” he says. “Things are very interconnected. And one of those connections seems to be the immune system. It’s not just fighting off foreign invaders — it’s also deeply involved in tissue maintenance and repair.”