The majority of young women at an increased risk of breast cancer due to chest radiation treatment for childhood cancer are not following breast cancer screening recommendations, according to a recently released, detailed assessment appearing in the January 28, 2009, issue of the Journal of the American Medical Association. [PubMed Abstract]
Researchers report that for this population, breast cancer risk elevates as soon as eight years after treatment with a median age of diagnosis from 32 to 35 years. By age 45, estimates show that between 12 to 20 percent of women treated with moderate-to high-dose chest radiation (RT) will be diagnosed with breast cancer. Because of this, for the past decade, the recommendation has been to initiate breast cancer surveillance with annual mammography starting at age 25 or eight years after radiation, whichever occurs last.
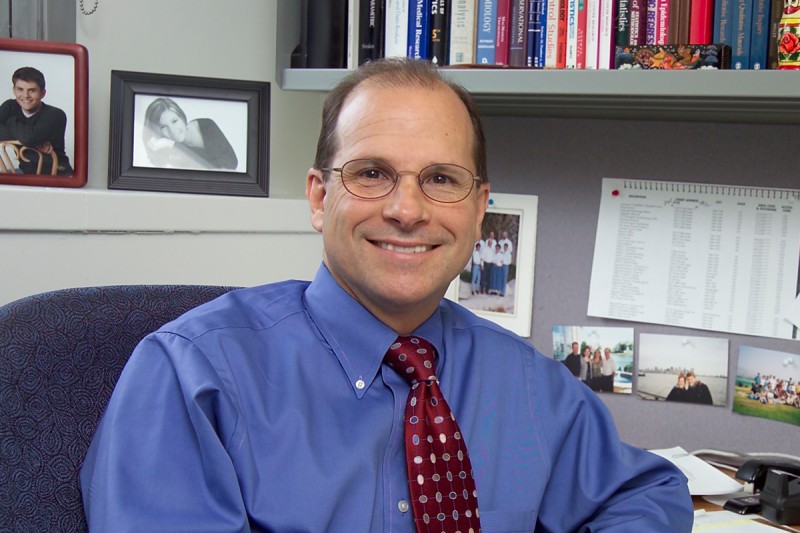
“We estimate that there are approximately 20,000 to 25,000 women who are 25 years or older who were treated with chest radiation as a child or young adult,” said Kevin C. Oeffinger, MD, Director of Memorial Sloan Kettering Cancer Center’s Program for Adult Survivors of Pediatric Cancers, and the study’s lead author. “Ideally, every one of these patients should be involved in a regular screening program.”
The study included 625 women, aged 25 through 50, who had been treated with chest RT for a pediatric cancer, and were participants in the Childhood Cancer Survivor Study (CCSS), a multi-institutional cohort comprised of long-term survivors diagnosed with a pediatric malignancy from 1970-1986. To better evaluate this population’s breast cancer screening practices, the authors compared their breast cancer screening practices to that of two other similarly aged groups - the first group was comprised of female cancer survivors not treated with chest RT, and the second were siblings of cancer survivors from the full CCSS cohort.
Of women aged 25 through 39 who were treated with chest RT, only 36.5 percent responded that they had a screening mammogram within the past two years; 47.3 percent reported that they had never had a mammogram; and 23.3 percent had a screening or diagnostic mammogram within the previous year. Among women age 40 through 50 who were treated with chest RT, the numbers were slightly higher, with 76.5 percent reporting a screening mammogram within the past two years. This was compared to the group not treated with chest RT who reported 70 percent, and the CCSS sibling group, who reported 67 percent.
“Most young women at risk of breast cancer following chest radiation for a pediatric cancer are not being appropriately screened, highlighting the fact that many women and their physicians are unaware of this risk of breast cancer at a young age,” said Dr. Oeffinger.
According to the assessment, the strongest predictor of mammography in women ages 25 through 39 is having a physician recommendation. The study also points to other factors, such as whether the physician is aware of the risk associated with chest RT, and how women perceive mammography. Having a positive view of screening mammography was associated with an increased likelihood of screening, regardless of age, the authors wrote.
“Moving forward, we must develop targeted interventions and work toward increasing the screening rate,” said Dr. Oeffinger. “We can do this by continuing to educate women about their risk and providing both them and their physician with the necessary information.”
