Karen Milich got the surprise call at 7:30 on a Saturday night. It was Bob Li, her medical oncologist at Memorial Sloan Kettering Cancer Center (MSK), telling her that he had obtained a slot for her on a clinical trial of a brand-new experimental drug called AMG 510. Karen, who had been living with advanced lung cancer for nearly a year, got up the next day and drove 20 hours from her home in Florida to New York City. About a week later, she started taking the drug.
That was August 2019. Since that time, Karen’s cancer has been wiped out. “I always tell Dr. Li I want to take my AMG to prevent my cancer like someone else takes an aspirin to prevent a heart attack,” Karen says. “I don’t feel any side effects from it at all.”
In May 2021, the U.S. Food and Drug Administration (FDA) approved AMG 510, now called sotorasib (Lumakras™), for a subset of people with lung cancer. The approval was based on the international clinical trial co-led by Dr. Li, which was published in The New England Journal of Medicine in June 2021.
Sotorasib looks like any other pill, but it represents an astounding breakthrough in cancer science. It blocks a cancer-causing protein that results from a mutation in a gene called KRAS (pronounced “kay-rass”). KRAS, discovered in 1982, was one of the first cancer genes ever found. Yet despite decades of research, scientists kept hitting roadblocks. That’s because the protein’s smooth, round shape lacked notches or grooves where drugs could attach. Scientists eventually gave this tenacious protein a label: undruggable.
When Karen was first diagnosed in the fall of 2018, sotorasib was not available. She received chemotherapy, radiation, and immunotherapy, but her cancer continued to grow. Then she learned she had been accepted into the MSK trial.
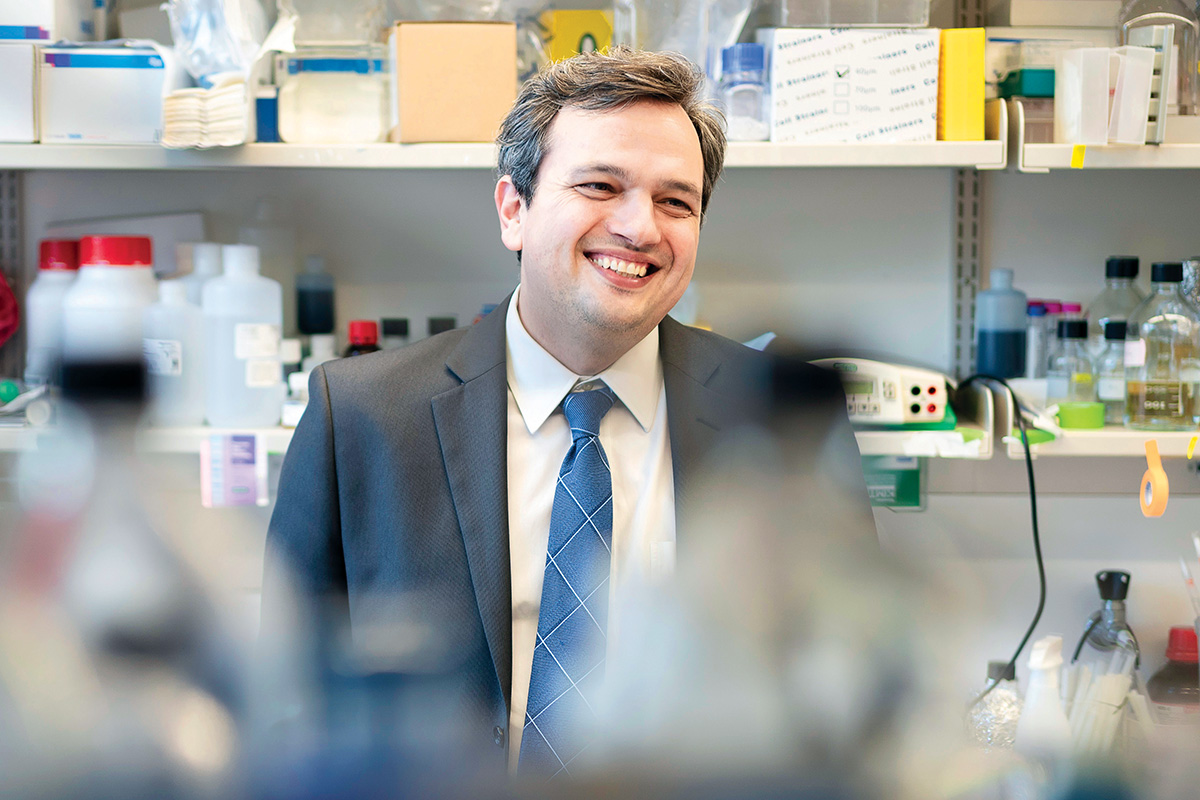
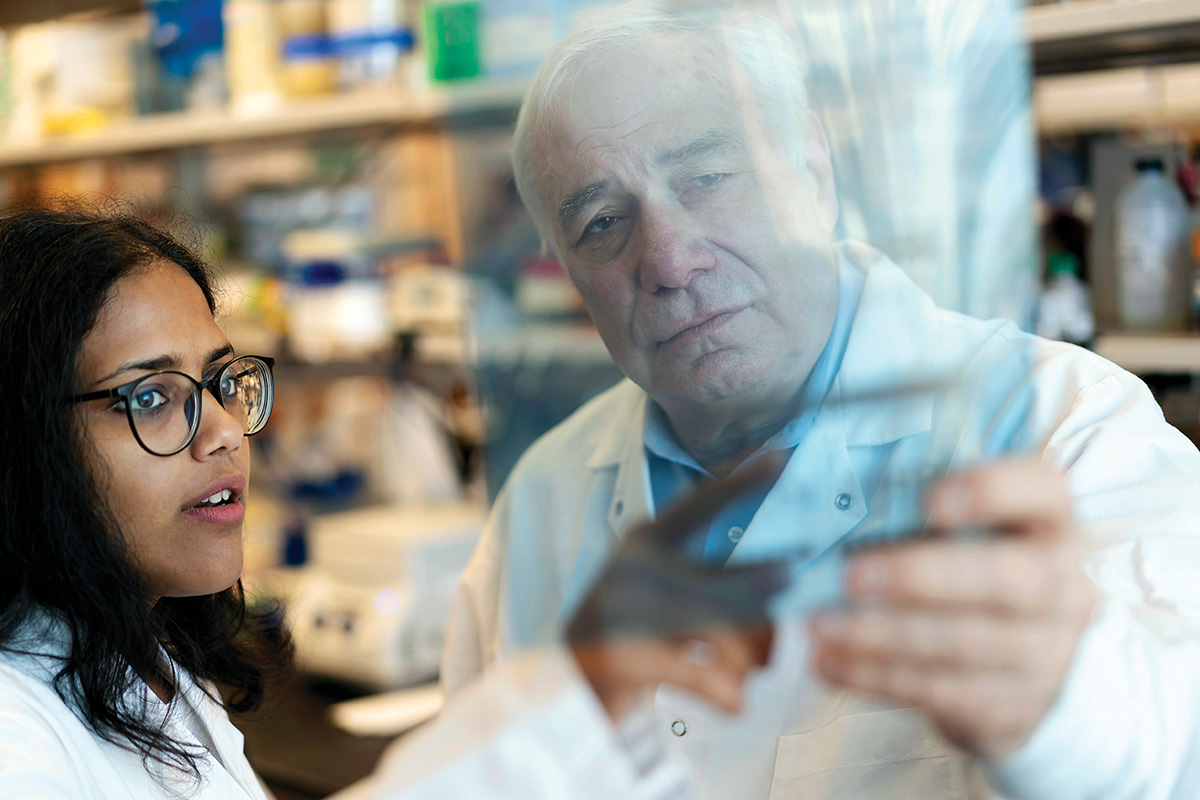
Sotorasib was developed thanks to years of hard work, much of it done at MSK, including in physician-scientist Neal Rosen’s lab in the Sloan Kettering Institute. In a paper published in Science in 2016, MSK physician-scientist Piro Lito and Dr. Rosen (Enid A. Haupt Chair in Medical Oncology) showed how it was possible to block the most common form of mutated KRAS in lung cancer, called KRAS-G12C. The FDA approved sotorasib for treating lung cancers with this specific KRAS mutation.
At the American Association for Cancer Research annual meeting in April 2022, researchers presented longer-term follow-up data for the clinical trial that led to sotorasib’s approval. Notably, nearly one-third of patients continued to survive after two years — a significant share for patients with advanced disease who had exhausted other treatment options.
“Karen’s got a remarkable story, but she’s not the only one who benefited,” Dr. Li says. “It’s a testament to what a milestone this is, to be able to target this protein that was previously considered to be really bad news.”
For patients who develop resistance to sotorasib, Drs. Lito and Li have recently published in Nature potential strategies to overcome these mechanisms. They also have launched clinical trials of combination therapies to continue to keep in check cancers driven by KRAS-G12C. One approach — combining sotorasib with immunotherapy — needs further study, after some patients showed signs of liver toxicity. Dr. Li’s research has found these side effects were lessened by giving low-dose sotorasib followed by a combination with pembrolizumab (Keytruda®), which is currently being developed as a potential first-line therapy for patients with KRAS-G12C-mutant lung cancer.
“What really sets MSK apart in this area is the combination of lab and clinical research focused on understanding how these drugs work and the best way to administer them,” Dr. Lito says.
In October 2021, MSK surgeon Vivian Strong (Iris Cantor Chair) used minimally invasive surgery to remove a small tumor in Karen’s abdominal cavity that was not responding to treatment. Karen’s latest tests show no evidence of active cancer. “I’m thankful to God every day for Dr. Li, MSK, and the trial,” Karen says. “They’re all incredible.”
Neal Rosen’s research has been supported by MSK Board Member Bruce C. Ratner.
Piro Lito is an alumnus of the Josie Robertson Investigators program at MSK, created and sustained by the Robertson Foundation.