To diagnose and treat cancer effectively, researchers need to learn about a tumor’s size, location, and metabolic activity. Some imaging techniques do this by focusing on the way cancer cells process nutrients. Tumors suck up more glucose (sugar) than normal cells, for example. After giving a patient a small amount of radioactive glucose, doctors can see the location of cancer cells as well as their metabolism on a PET scan.
A new form of imaging called hyperpolarized MRI (HP MRI) takes this approach a step further, providing a highly detailed picture of a tumor’s metabolic activity. The laboratory of Kayvan Keshari, a Memorial Sloan Kettering biochemist and imaging specialist, is investigating the use of HP MRI to show how tumors may be responding to treatment. In recent years, they established that this approach can work to image prostate cancer and brain tumors.
Now Dr. Keshari’s team has demonstrated that HP MRI can reveal whether prostate cancer is likely to grow or spread. The researchers may also have discovered what enables the tumor to become aggressive.
“Wanting to know whether a tumor is aggressive is the biggest question faced by people with prostate cancer,” Dr. Keshari says. “HP MRI could be a fast, noninvasive way to determine if someone actually needs treatment, like surgery or radiation, or whether the cancer can be closely monitored instead. And knowing what’s driving the uptake of nutrients and causing the tumor to be aggressive could lead to new avenues of drug development.”
The findings are reported today in the journal Cell Metabolism.
Major Signal Boost
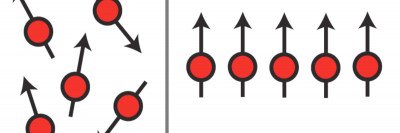
Conventional MRI uses radio waves and a powerful magnet linked to a computer to create detailed pictures of the inside of the body. HP MRI is based on the fact that at a low temperature and in a high magnetic field, electrons have a very high level of polarization, meaning nearly all the electrons are aligned. With HP MRI, the molecules of a sugar solution are oriented to the MRI’s magnetic field before the solution is injected into the patient.
The hyperpolarization boosts the signal captured by the MRI more than 10,000-fold. As the solution is processed by the cancer cells, doctors get an immediate, clear snapshot of a tumor’s metabolic activities. For example, HP MRI can detect when a cancer cell converts a sugar molecule from one form to another. Researchers can glean important information about tumor activity by tracking and measuring this conversion.
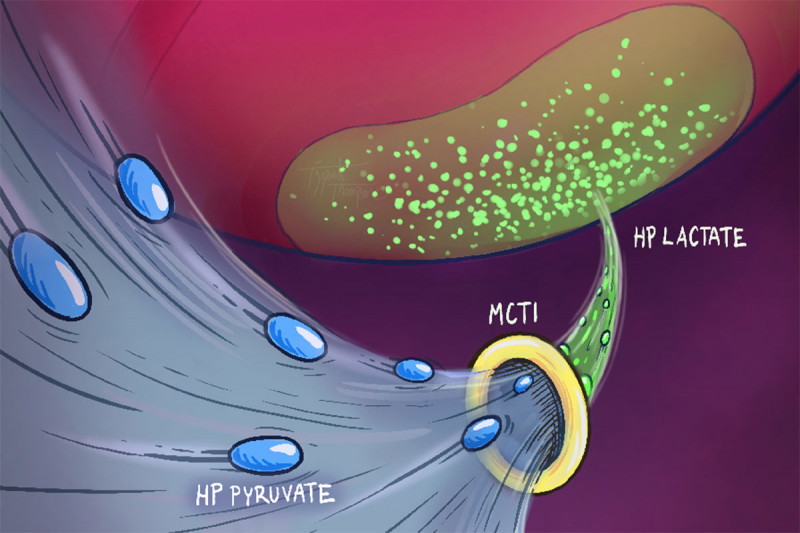
Earlier research by Dr. Keshari’s team suggested that one marker for aggressive prostate cancer is a high level of a molecule called lactate. This is a byproduct of the metabolic process through which cells convert glucose into energy. Cells first break down glucose into pyruvate, which is then converted into lactate.
The researchers wanted to see if this pyruvate-to-lactate conversion could be tracked and measured by HP MRI. If so, a stronger HP MRI signal would indicate a higher lactate level, and presumably, more-aggressive cancer.
Signal Strength and Aggressiveness
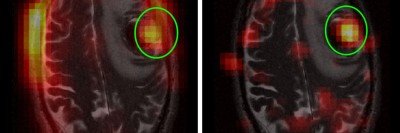
In the study, the researchers looked at HP MRI images of prostate cancer in people who were going to have their prostate surgically removed as part of their treatment. The patients were injected with HP pyruvate and imaged with HP MRI to measure their lactate levels.
The researchers studied the relationship between these images and the Gleason grade given to the tumor after it was removed. (The Gleason grade is a number assigned by pathologists examining a prostate biopsy. A higher grade indicates more-aggressive cancer.) They found that a signal indicating higher lactate levels in the cancer cells correlated with a higher Gleason grade in the tumor sample.

Genetic analysis of the samples also showed that higher lactate levels correlated with higher expression of a gene that makes a protein called MCT1. This protein helps transport pyruvate as well as lactate into cells to be metabolized. This is likely the reason why these high-grade prostate cancers make such high levels of hyperpolarized lactate.
“The increase in MCT1 levels suggests that targeting the protein with drugs could inhibit lactate metabolism and slow prostate cancer growth,” Dr. Keshari says.
The researchers also found that prostate tumors with higher lactate levels were more likely to have mutations in a gene called PTEN. Mutations in this gene, which acts as a tumor suppressor, are associated with many cancers, and many drugs are being tested to target this mutation.
The next step will be to expand the use of HP MRI in larger groups of people with prostate cancer, including those with cancer that has spread to another part of the body, to validate the link between what the imaging shows and the cancer’s aggressiveness. The imaging method needs to be clinically proven before being used in a person’s official diagnosis.
“We think HP MRI will continue to teach us a lot about prostate cancer and help us assess the aggressiveness of the disease, suggest drug strategies, and eventually guide treatment decisions,” Dr. Keshari says.